Anerior Labral Repair(Banskart) Rehabilitation Guidelines
Table of Contents
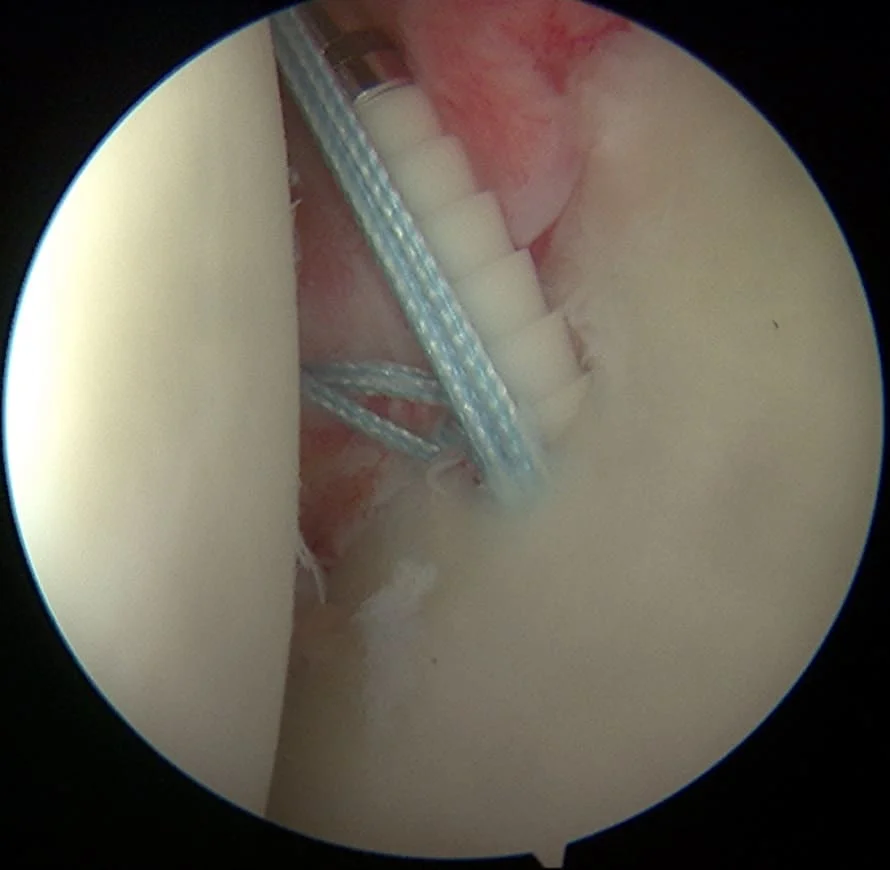
Definition
Anterior labral rehabilitation guidelines refer to a set of recommended protocols and strategies designed to facilitate the recovery and rehabilitation of injuries to the anterior (front) aspect of the labrum in the shoulder joint. The labrum is a ring of cartilage that lines the rim of the shoulder socket and provides stability to the joint.
In the context of anterior labral injuries, rehabilitation guidelines typically include various exercises, stretches, and therapeutic interventions aimed at promoting healing, restoring range of motion, improving strength and stability, and eventually enabling the individual to return to their normal activities or sports. These guidelines are often developed by medical professionals, such as orthopedic surgeons, physical therapists, and sports medicine specialists.
Some common components of anterior labral rehabilitation guidelines might include:
Initial Rest and Protection: After an injury, a period of rest and immobilization might be recommended to allow the labrum to heal. This could involve using a sling or brace to limit movement.
Pain and Inflammation Management: Techniques to manage pain and reduce inflammation might include icing, anti-inflammatory medications, and other modalities as prescribed by a healthcare provider.
Range of Motion Exercises: Gradually introduce gentle and controlled movements to prevent stiffness and maintain or improve the content of motion in the shoulder joint.
Strengthening Exercises: Progressive exercises to strengthen the muscles around the shoulder joint, particularly those that support the labrum and help stabilize the joint.
Proprioceptive and Neuromuscular Training: Activities that enhance the body’s awareness of joint position and movement, as well as training the muscles to react appropriately to different movements and positions.
Functional Exercises: Activities that simulate the movements and demands of the individual’s daily activities or sports to ensure a safe return to these activities.
Gradual Progression: Rehabilitation should gradually progress, gradually increasing the intensity, complexity, and load of exercises as the individual’s condition improves.
Patient Education: Educate the patient about their injury, the rehabilitation process, and proper body mechanics to prevent future injuries.
Monitoring and Adjustment: Regular assessments by healthcare professionals to monitor progress and adjust the rehabilitation plan as needed.
It’s important to note that anterior labral injuries can vary in severity, and rehabilitation protocols may be tailored to the specific needs of each individual. These guidelines are generally part of a comprehensive treatment plan that may also involve other interventions like manual therapy, soft tissue techniques, and sometimes surgical intervention, depending on the extent of the injury. Always consult a qualified healthcare professional for personalized advice and guidance based on your situation.
Anterior Labral Repair (Banskart)Rehabilitation Guidelines
Phase I Secure ROM
- postoperative week 0-6
Goals
- Rebuild Painless ROM
- Slow muscle atrophy of the entire upper limb complex
- To improve neuromuscular control of the scapula in a neutral glenohumeral position
- Reduces pain and inflammation
Precautions
- The patient should remain on leash at all times except dressing/swimming/PT until 4th week
- Avoid straining (and repairing) the anterior inferior labrum.
(No shoulder extension / IR behind back / Lift / ER in abduction)
Activities
- Postoperative week 0-4
- Post-operative support and/or splint can be removed 2-3 times a day.
PROM/AAROM and Codman Pendulum Exercises - Photometry
- Gentle stabilization/mobilization of the scapula
- Active elbow flexion and extension
- Can squeeze a softball
- Post-operative week 5-6
- The charger and/or the child are terminated
- Begin lower limb and core strengthening, light cardio
- PROM progresses to full PROM at week 6 (including ER with shoulder abduction)
- If necessary, begin to tighten the posterior capsule (added earlier if released)
- Scapulothoracic stabilization/mobilization/isometric progression
- Once Full PROM is achieved, the therapist can add AAROM to all levels
Phase II Early approval
- Post-operative weeks 7-12
Goals
- Run AROM and continue
- Gradual recovery of shoulder/scapular strength, power, and endurance
- Prepare to return to functional activities
Precautions
- No lifting more than 10 pounds, sudden lifting or pushing, overhead lifting Activities
- Post-operative weeks 7-12
- Promote gentle PREs in all planes of motion (add biceps for protection
repair) - Begin active assisted exercises, deltoid/rotator isometrics at 8 weeks
- Add light PNF patterns (Bodyblade/Plyoball/etc. in non-provocative positions)
- Gradually strengthening the rotator cuff
- Stabilization/mobilization/strengthening of the scapula as it progresses
Phase III Functional rehabilitation
- Post-operative week 13-16
Goals
- Gradually return to full AROM mode Activities
Post-operative week 13-16 - Continue to strengthen the rotator cuff and elbow flexion
a. Emphasize external rotation and latissimus eccentrics muscles - Emphasize timing and rhythm with PNFs (Bodyblade Overhead, Plyoball Throwing)
- Stabilize the humerus-scapular joint in a functional position
- Continue to treat the whole body (heart, heart, and lower extremities).
Phase IV Return to activity
- Months after studies 4-5
Goals
- Complete and painless Activities
- Aggressive eccentric strengthening and scapular stabilization
- Start a plyometric program
- Continue resistance training
- Begin an interval throwing program when ROM/strength is adequate (upper corridors)
- Support ROM and flexibility
Phase V Return to sports
- Months after operations 6-7
Goals
- Complete and painless Activities
- Return to full activity as permitted
Causes
Trauma or Injury: A significant blow to the shoulder, such as a fall onto an outstretched arm or a direct impact, can cause the labrum to tear. This is especially common in athletes who engage in sports with repetitive overhead movements, like baseball players and swimmers.
Repetitive Overhead Movements: Activities that involve repetitive overhead motions, such as throwing, serving in tennis, or swimming, can gradually wear down the labrum and increase the risk of tears over time.
Degenerative Changes: As a person ages, the labrum can naturally undergo degenerative changes, becoming more prone to tears. This is more common in older people.
Labral Fraying: Over time, the labrum can develop small frays or fringes, especially with repeated motions. These frayed edges can potentially lead to larger tears.
Structural Abnormalities: Some individuals might have anatomical variations in their shoulder joint, such as a shallow socket (glenoid), which can predispose them to labral tears. This is many times referred to as shoulder instability in the patient.
Poor Mechanics or Muscle Imbalances: Muscle imbalances or poor shoulder mechanics can put extra stress on the labrum and surrounding structures, increasing the risk of injury.
Weightlifting or Heavy Lifting: Engaging in heavy weightlifting, particularly exercises that involve lifting heavy weights overhead, can strain the labrum and lead to tears.
Direct Impact: A direct blow to the shoulder, such as from a fall or collision, can cause the labrum to tear or detach from the bone.
Congenital Factors: Some individuals may be born with anatomical abnormalities that make their labrum more susceptible to injury or tears
FAQ
What is the anterior labrum, and why is rehabilitation necessary?
The anterior labrum is a ring of cartilage in the front of the shoulder joint that helps stabilize the joint. Rehabilitation is necessary when there is an injury or tear in this structure, often due to trauma or overuse, to restore function and prevent further damage.
How do I know if I have an anterior labral injury?
Common symptoms include shoulder pain, instability, clicking or popping sensations, and limited range of motion. An orthopedic specialist can diagnose it through physical exams and imaging tests.
Do I need surgery for an anterior labral tear, or can it be treated with rehabilitation alone?
The treatment approach depends on the severity of the tear. In many cases, conservative rehabilitation is initially attempted. Surgery may be necessary for more severe tears or if conservative methods fail to improve symptoms.
What does anterior labral rehabilitation involve?
Rehabilitation typically includes physical therapy exercises to strengthen the shoulder muscles, improve range of motion, and stabilize the joint. It also focuses on pain management and functional recovery.
Can I do these exercises at home, or should I work with a physical therapist?
While some exercises can be done at home, it is generally recommended to work with a physical therapist. They can tailor the program to your specific needs, monitor your progress, and ensure proper form to prevent further injury.
How long does anterior labral rehabilitation take?
The duration varies based on the severity of the injury and the individual’s response to treatment. Rehabilitation could range from 1 to 2 weeks to several months
Are there any specific exercises I should avoid during anterior labral rehabilitation?
Certain exercises or movements that put excessive stress on the shoulder joint should be avoided, such as heavy overhead lifting or extreme ranges of motion. Your physical therapist will provide guidance on what to avoid.
What can I do to manage pain during rehabilitation?
Pain management strategies may include ice, anti-inflammatory medications, and modifying activities that worsen pain. Your healthcare provider can prescribe appropriate pain relief methods.
Can I return to sports or strenuous activities after anterior labral rehabilitation?
Returning to sports or strenuous activities should be gradual and based on your progress and the advice of your healthcare team. Full recovery may take time, and rushing it can lead to reinjury.
How can I prevent future anterior labral injuries?
To reduce the risk of future injuries, it’s essential to maintain shoulder strength and flexibility, use proper form during activities, and avoid overexertion. Regular shoulder exercises and proper warm-up techniques can help.