Fingers mobilization exercise
Table of Contents
What is mobilization for Fingers?
- Finger Mobilization is a passive, skilled, manual therapy procedure that appeals to joints related to the soft tissue at various speeds and amplitudes utilizing a physiological or accessory movement for therapeutic purposes
- small amplitude force applies at a fast velocity, and a large amplitude force applies at to slow velocity
- it is a manual technique that involves appealing to the target forces on a painful, stiff, or negotiated jointly with regard to improving its overall function. Which is not convenient in all situations, joint mobilizations help enhance the range of motion, reduce pain, and minimize stiffness.
- Joint mobilization is a hands-on treatment that is usually executed by physiotherapists healthcare professionals who specialize in rehabilitation for movement disorders and chiropractors, health professionals treating conditions of the musculoskeletal system that include bones, muscles, and soft tissue, ligaments
Introduction of finger complex

- metacarpophalangeal joint
- interphalangeal joint
- carpometacarpal joint of the thumb
Metacarpophalangeal joint of the finger
- The metacarpophalangeal (MCP) joints are diarthrodial joints where the large convex heads of the distal aspect of the metacarpals fabricate with the concave-shaped proximal aspect of each phalange. The fabricating surface of each metacarpal head and proximal phalange is contained hyaline cartilage. There are five individual MCP joints in each hand and these joints serve as passages between the palm and the fingers.
Blood Supply of the MCP joint
- Blood is transferred to the hand by the ulnar and radial arteries which anastomose in the superficial palmar and deep palmar arches. These arches have numerous branches, many of which supply the MCP joints involving the pollicis artery, the radial artery of the index finger, common palmar digital arteries, and the dorsal and palmar metacarpal arteries.
- Lymphatic drainage for the hand happens via superficial channels that run alongside the cephalic and basilic veins along with deep channels that course with the arteries. These lymphatics drain to lymph nodes without the elbow involving the cubital and epitrochlear lymph nodes, before ultimately draining into the axillary or infraclavicular lymph nodes.
- The muscles encompassing the metacarpal phalangeal joint gain innervation via branches from the three main nerves of the forearm: median nerve, ulnar, nerve, and radial nerve. The MCP joints receive their innervation from the posterior interosseous nerve, the deep terminal branch of the ulnar nerve, and also the palmar branches of the median nerve.
- Both intrinsic and extrinsic muscles encompass the MCP joint. Intrinsic muscles are those muscles that arise without the hand while extrinsic muscles are those which is outside the hand. The MCP joint may also be grouped by their respective movement type which mentions below with particular muscle attachment
Muscles of the MCP joint
- Extension
- Digits 2 to 5: Extensor digitorum, extensor indices (second finger), extensor digiti minimi (fifth finger)
- Thumb muscle: Extensor pollicis longus, Extensor pollicis brevis
- Flexion
- fingers 2 to 5: Flexor digitorum superficialis, flexor digitorum profundus, Flexor digiti minimi brevis (fifth finger), Lumbricals
- flexion movement of the thumb: Flexor pollicis longus, Flexor pollicis brevis
- Abduction
- fingers 2 to 4: Dorsal Interossei
- Fifth finger: Abductor digiti minimi
- abduction movement of the thumb: Abductor pollicis longus, Abductor pollicis brevis
- Adduction
- Digits 2 to 5: Palmer interossei
- Thumb adductors: Adductor pollicis
The interphalangeal joint of the finger
- The interphalangeal joint of the hand is the hinged variety of synovial type uniaxial joints in the middle of the phalanges of the fingers that give flexion towards the palm of the hand.
- There are two parts on each finger (except for the thumb, which has only one joint)
- Proximal interphalangeal joints” PIJ or PIPJ”, those in the middle of the first also termed proximally phalanges
- Distal interphalangeal joints” DIJ or DIPJ”, those in the middle of the second (intermediate) and the third (distal) phalanges
Ligaments & Joint Capsule of the IP joint
- encompassing each interphalangeal joint there is a fibrous joint capsule, the inner lining of which is constituted of a synovial membrane. Strengthening each joint capsule are two collateral ligaments and a palmar ligament also termed a palmar/volar plate. Dorsally, the joint capsule is strengthened by a widening of the extensor tendons. This extensive ligamentous contribution to each joint capsule accelerates the articular surface of the phalangeal base, improving joint conformity.
Muscles of the IP joint
- The extraordinary dexterity presented by the fingers is imitated in the number of muscles that can act upon muscle. Both intrinsic and extrinsic hand muscles are liable for generating flexion-extension movements at the interphalangeal joints of the hand.
- Muscles acting on the interphalangeal joints of the hand and the movements they generate
- Flexion of IP joint of thumb muscle – Flexor pollicis longus
- PIP joints of fingers 2 to 5 – Flexor digitorum superficialis, flexor digitorum profundus
- DIP joints of finger 2 to 5 – Flexor digitorum profundus
- Extensors IP joint of the thumb – Extensor pollicis longus
- PIP joints of digits 2 to 5 – Extensor digitorum, lumbricals, dorsal interossei, extensor indices (digit 2), palmar interossei (digits 2,4,5)
- DIP joints of digits 2 to 5 – Extensor digitorum, lumbricals, dorsal interossei, extensor indices (digit 2), palmar interossei (digits 2,4,5)
- Flexion of the interphalangeal joint of the thumb is consummate through the action of the flexor pollicis longus muscle. The proximal interphalangeal joints of fingers 2 to 5, are simultaneously flexed via the flexor digitorum superficialis and flexor digitorum profundus, then also extends to the distal phalanx, and is, therefore, the only muscle eligible for flexing the distal interphalangeal joints.
- Extension of the interphalangeal joint of the thumb is demonstrated by the extensor pollicis longus. Both the proximal and distal interphalangeal joints of fingers 2 to 5 are extended through the movement of the extensor digitorum, lumbricals, and dorsal interossei. Digit 2, the index finger, gets additional extension via the extensor indices, when the palmar interossei compensate with an extension of digits 2, 4, and 5. The muscles responsible for extending digits 2 to 5 do through their tendinous aponeurotic insertion into the extensor expansion. This hood-like expansion extends down the length of fingers 2 to 5 and is embedded on each side by the palmar ligament. It rolls to maintain the direction of pull of the extensor tendons in the midline of each finger.
Range of Motion of the IP joint
- The typical range of motion (ROM) at the proximal interphalangeal joint (PIPJ) and distal interphalangeal joint (DIPJ)
- The range of motion of the thumb subsists of up to about 90° flexion and 10° extension, with passive hyperextension possible when a large amount of force is enforced on the distal phalanx. The degree of flexion of the proximal interphalangeal joints increases slightly beyond digits 2-5, however, can be generally said to be in the range of 100° to 110°. In the case of the distal interphalangeal joints, 3rd finger shows the greatest degree of flexion (80°), with 5th finger promoting the least (70°).
Carpometacarpal joint of the thumb

- carpometacarpal joint of the thumb is a saddle variety
muscle and movements of the CMC joint of the thumb
- Flexion
- Adductor pollicis
- Flexor pollicis longus
- Opponens pollicis
- Flexor pollicis brevis
- Extension
- Extensor pollicis brevis
- Extensor pollicis longus
- Abductor pollicis longus
- Abduction
- Abductor pollicis brevis
- Abductor pollicis longus
- Adduction
- Adductor pollicis
- Extensor pollicis longus
- First dorsal interosseus
- Opposition
- Opponens pollicis
- Flexor pollicis brevis
- Abductor pollicis brevis
- Flexor pollicis longus
- Abductor pollicis longus
- Reposition
- Extensor pollicis longus
- blood supply: palmar and dorsal carpal anastomotic arches
- nerve supply: ulnar nerve and it’s a deep branch
The condition needs mobilization of the finger
- trigger finger/thumb
- mallet finger
- swan neck deformity
- button hole deformity
- dupuytren contracture
- dequervian tenosynovitis
- carpal tunnel syndrome
- flexor tendon injuries
- ape thumb
- opera glass hand
- game keeper’s thumb
- ulnar drift
The Procedure required mobilization of the finger after surgical approaches
- Surgical Repair of Acute Ulnar Collateral Ligament Injury of the Thumb
- Open Reduction for Joint Dislocation
- Arthroplasty
- synovectomy
- osteotomy
- arthrodesis
- reconstructive surgery
- tendon transfer
Goals for wrist joint mobilization
pain, muscle guarding, and spasm
- painful joint, reflex, muscle guarding, and muscle spasm can be expressed with gentle joint play techniques to encourage neurophysiological and mechanical effect
Neurophysiological effect
- small amplitude oscillatory and distraction movement are used to stimulate mechano-receptors that may prevent the transmission of nociceptive stimuli at the spinal cord or brain stem level
Mechanical effect
- small amplitude distraction or gliding movement of the joint is used to cause synovial fluid movement, which is a vehicle for taking nutrients to avascular portions of the articular cartilage
- gentle joint play techniques help to maintain nutrient exchange and prevent the painful and degenerating effects of statis when the common is swollen or painful, and can not go through a range of motion
- when adapted to treat pain, muscle spasms, and muscle guarding these techniques should not put a stretch on the reactive tissue
Reversible joint hypomobility
- reversible joint hypomobility can be treated with progressively vigorous joint play stretching technique to elongate hypermobile capsular and ligamentous connective tissue
- sustained or distraction stretch forces are used to distend the shortened tissue mechanically
Positional faults/subluxations
- A faulty position of one bony participant in relation to its opposing surface may outcome in limited motion or pain
- positional faults can start with traumatic injury, after periods of immobility, muscle imbalance
- the faulty position may be preserved by maladapted neuromuscular control beyond the joint
- during attempting an active range of motion, faulty tracking of the joint surface outcome in pain, or limited motions
Progressive limitations
- diseases that progressively diminish movement can be treated with joint play techniques to maintain available motion or reduce progressive mechanical restrictions
- the patient’s response aspect the dosage of distraction or glide to treatment and the state of the disease
Functional immobility
- when the patient is unable to functionally move a joint for a longer period of time
- the joint can be treated with nonstretch gliding or distraction technique to maintain available joint play and prevent the degenerating and restricting effect of immobility
Grades of mobilization of the wrist joint
Non-thrust oscillation techniques
- the oscillation may be initiated through physiological movement
- grade 1:small amplitude rhythmic oscillation is applied at the start of the range, rapid oscillation like manual vibration
- grade 2:large amplitude rhythmic oscillation is applied within range, not reach the limit, perform 2 or 3 seconds for 1 to 2 minutes
- grade3:large amplitude rhythmic oscillation is demonstrated up to an available range of motion, stress into tissue resistance, perform 2 or 3 seconds for 1 to 2 minutes
- grade4:small amplitude rhythmic oscillation is executed at the available range of movement, the stress in tissue resistance, rapid oscillation like manual vibration
- grade 1 and 2 are applicable to treat joint limitation of movement by pain or muscle guarding
- grade 3 and 4 are applicable for stretch technique
Nonthrust sustained joint play techniques
- This system explains only joint play techniques that separate (distract) or glide the joint surface
- grade 1(loosen): small amplitude distraction is demonstrated when no stress is put on the capsule, it equalizes cohesive force, muscle tension, and atmospheric pressure acting on joint
- grade2(tighten): enough distraction or glide is given to tightening the tissue surrounding the elbow joint
- grade3(stretch): a distraction or glide is given with an amplitude large enough to put a stretch on the joint capsule surrounding the periarticular structure
- grade 1 distraction is given with all glide motion
- Give periodic distraction for 7 to 10 seconds with a few seconds of rest among several cycles
- grade 2 distraction is helpful in identifying the sensitivity of the joint, once the joint reaction is known treatment dosage accelerates and decelerates
- gentle grade 2 distraction initiated periodically used to inhibit pain and maintain joint play when ROM is not allowed
- grade 3 distractions or glides are used to stretch joint structure, increase joint play motion
- for limited joints apply a minimum of 6 seconds of stretch force chased by partial release (grade 1 or 2)
- reps:3 to 4-second intervals
The metacarpophalangeal and interphalangeal joints of the fingers
- the distal end of the proximal trabecular surface is convex and the proximal end of the distal trabecular surface is concave
- because all trabecular surface is the same for all digits of the fingers
- all techniques are given in the same way to each joint
- Resting position: the resting position is in slight flexion for all joints
- Treatment plane: distal articulating surface
- stabilization: the forearm and hand are supported on the treatment table
- stabilize the proximal articulating surface with the fingers of one hand
Metacarpophalangeal joint and interphalangeal joint distraction

- patient position: sitting with forearm supported on the treatment table
- place the rolled towel under the wrist joint for comfort
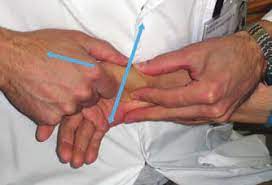
Therapist position and hand placement
- use the proximal hand to stabilize the proximal bone, and wrap the fingers and the thumb of your other hand around the distal bone close to the joint
mobilizing force
- apply long axial traction to separate the joint surface
- distraction glide is used to treat initial pain control, improve general mobility
Metacarpophalangeal joint and interphalangeal joint volar glide

- patient position: sitting with forearm supported on the treatment table
- place the rolled towel under the wrist joint for comfort
Therapist position and hand placement
- use the proximal hand to stabilize the proximal bone, and wrap the fingers and the thumb of your other hand around the distal bone close to the joint
mobilizing force
- the glide force is rubbed by the thumb or thenar eminence against the proximal end of the bone to be pushed
- progress by carrying the joint to the end of its available range
- rubbed slight distraction and glide force
- rotation may be added prior to rubbing the gliding force
- volar glide is used to increase flexion
Metacarpophalangeal joint and interphalangeal joint dorsal glide

- patient position: sitting with forearm supported on the treatment table
- place the rolled towel under the wrist joint for comfort
Therapist position and hand placement
- use the proximal hand to stabilize the proximal bone, and wrap the fingers and the thumb of your other hand around the distal bone close to the joint
mobilizing force
- the glide force is rubbed by the thumb or thenar eminence against the proximal end of the bone to be pushed
- progress by carrying the joint to the end of its available range
- rubbing slight distraction and glide force
- rotation may be added prior to rubbing the gliding force
- dorsal glide is used to increase extension
Metacarpophalangeal joint and interphalangeal joint radial glide

- patient position: sitting with forearm supported on the treatment table
- place the rolled towel under the wrist joint for comfort
Therapist position and hand placement
- use the proximal hand to stabilize the proximal bone, and wrap the fingers and the thumb of your other hand around the distal bone close to the joint
mobilizing force
- the glide force is rubbed by the thumb or thenar eminence against the proximal end of the bone to be pushed
- progress by carrying the joint to the end of its available range
- rubbing slight distraction and glide force
- rotation may be added prior to rubbing the gliding force
- radial glide is used to increase abduction
Metacarpophalangeal joint and interphalangeal joint ulnar glide

- patient position: sitting with forearm supported on the treatment table
- place the rolled towel under the wrist joint for comfort
Therapist position and hand placement
- use the proximal hand to stabilize the proximal bone, and wrap the fingers and the thumb of your other hand around the distal bone close to the joint
mobilizing force
- the glide force is rubbed by the thumb or thenar eminence against the proximal end of the bone to be pushed
- progress by carrying the joint to the end of its available range
- rubbing slight distraction and glide force
- rotation may be added prior to rubbing the gliding force
- ulnar glide is used to increase adduction
Carpometacarpal joint of the thumb
- Resting position: midway between radial abduction and adduction and between palmar abduction adduction
- stabilization: fixate the trapezium with the nearer hand to the patient
- treatment plane: the treatment plane is in the trapezium for abduction and adduction
- in the proximal metacarpal for flexion and extension
Carpometacarpal distraction
- patient position: the forearm and hand relax on the treatment table
Hand placement
- fixate the trapezium with the nearer hand to the patient
- grasp the patient’s metacarpal by wrapping your fingers around it
mobilizing force
- apply long axial traction to separate the joint
Carpometacarpal ulnar glide

patient position and hand placement
- stabilize the trapezium by clasping it directly or by wrapping your fingers around the distal row of carpals
- place the thenar eminence of your other hand against the base of the patient’s first metacarpal on the side opposite to the desired glide
mobilizing force
- apply the force with your thenar eminence against the base of metacarpal
- ulnar glide to increase radial adduction
Carpometacarpal radial glide

patient position and hand placement
- stabilize the trapezium by clasping it directly or by wrapping your fingers around the distal row of carpals
- place the thenar eminence of your other hand against the base of the patient’s first metacarpal on the side opposite to the desired glide
mobilizing force
- apply the force with your thenar eminence against the base of metacarpal
- radial glide to increase radial abduction
Carpometacarpal dorsal glide

patient position and hand placement
- stabilize the trapezium by clasping it directly or by wrapping your fingers around the distal row of carpals
- place the thenar eminence of your other hand against the base of the patient’s first metacarpal on the side opposite to the desired glide
mobilizing force
- apply the force with your thenar eminence against the base of metacarpal
- dorsal glide to increase palmar abduction
Carpometacarpal volar glide

patient position and hand placement
- stabilize the trapezium by clasping it directly or by wrapping your fingers around the distal row of carpals
- place the thenar eminence of your other hand against the base of the patient’s first metacarpal on the side opposite to the desired glide
mobilizing force
- apply the force with your thenar eminence against the base of metacarpal
- volar glide to increase palmar adduction
Precaution for finger joint
- People who have not promoted arthritis of the finger can take steps to help recover joint damage in their hands. Some tips for preventing joint damage involve:
- applying an ergonomic keyboard and mouse when working at the computer
- avoiding carrying out heavy items that can put a strain on the fingers and hand
- applying splints or braces to diminish the risk of injury when using the hands for repetitive activities, such as sewing or chopping food
- If a person is living with pain in their hands then some steps take which mention below
- practicing gentle motion hand exercises that promote movement and help lessen stiffness
- exploring physical therapy and occupational therapy from certified professionals
- conversation with a doctor about medications and topical pain relievers to help with the pain
- use hot or cold therapy
- modify their daily routine to avoid taking stress on their hands and fingers
- consult a doctor about steroid injections
- apply kinetic tape as a preventive measure
- using transparent software in place of typing
- neglect putting excess strain on the fingers by using large joints, such as the elbows or shoulders, to carry the weight of shopping bags
- using other body parts besides the hands near a door
- using the palm of the hand to grasp a phone or tablet to avoid putting strain on the fingers
- changing daily habits, such as stirring food using a shoulder motion
- using utensils with large, easy-to-grip handles
Hypermobility
- the joint of a patient with potential necrosis of the ligaments should not be manipulated with stretching techniques
Joint effusion
- the joint effusion as a result of trauma or disease
- rapid swelling of the joint generally indicates bleeding in the joint and may occur with diseases
- medical intervention is necessary for aspiration of the blood to decrease the necrotizing effect on the articular cartilage
- slow swelling for more than 4 hours generally declares serious joint effusion or edema on the joint due to mild trauma irritation or disease
- do not stretch swollen joints with mobilization because the capsule is already stretched by being expanded to contain the extra fluid
- the limitation of movement is from extra fluid and muscle response to pain, not from shortened fibers
- a slight oscillating movement that does not stress or stretch the capsule may need to block the transmission of a pain stimulus so it is not anticipated and may use to regain fluid flow during maintaining available joint play
- if the patient’s response to slight techniques is accelerated pain or joint irritability
- the techniques were applied too forcefully or should not do with the current state of pathology
Inflamation
- whenever inflamation is present, stretching cause increase pain and muscle guarding and result in greater tissue damage
- gentle distraction motions may temporarily diminish the pain response
FAQS
- Does the swan neck deformity reduces by mobilization ??
soft tissue release and gentle mobilization reduce pain and stiffness around the joint
- How does joint mobilization reduce pain?
grade 2:large amplitude rhythmic oscillation is start within range, not reaching the limit, demonstrate 2 or 3 seconds for 1 to 2 minutes
that transfer center way into the joint range of motion, attending any part of the range and yet not reaching the end range. This technique can be given to treat joint stiffness by accelerating the range of motion and joint pain - can finger stiffness go away with the mobilization?
fingers mobilization is established to be effective in post-traumatic or post-operative finger injury cases.
- How long do you do joint mobilization for the fingers?
Typical treatment of a finger joint may add a series of three to six mobilizations carried on up to 30 seconds, with one to three oscillations or glide per second
- how much time is taken for mobilization after total synovectomy?
after 1 or 2 months of POP, mobilization is applied because the synovial formation of bone takes time to connect the bone





