Facial Nerve: The Seventh Cranial Nerve
The facial nerve (also known as the seventh cranial nerve) is a nerve that carries signals from the brain to the muscles of the face. This nerve is responsible for the ability to move the muscles of the face, and it also carries information related to sensation in the face. Specifically, the facial nerve is responsible for the ability to smile, raise eyebrows, close the eyes, and other facial functions. The facial nerve is also responsible for the ability to taste and feel the texture of food in the mouth.
The facial nerve, or cranial nerve (CN) VII, is the nerve of facial expression. The facial nerve has two functions: to carry sensory information to the brain and to cause the muscles of the face to move.
Table of Contents
Anatomy Facial Nerve:
It emerges from the pons of the brainstem, controls the muscles of facial expression, and functions in the conveyance of taste sensations from the anterior two-thirds of the tongue. It arises from the brainstem from an area posterior to the cranial nerve VI (abducens nerve) and anterior to cranial nerve VIII (vestibulocochlear nerve).
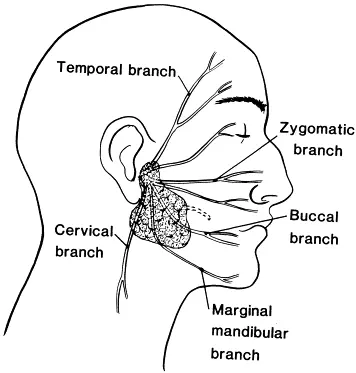
Branches of Facial nerve
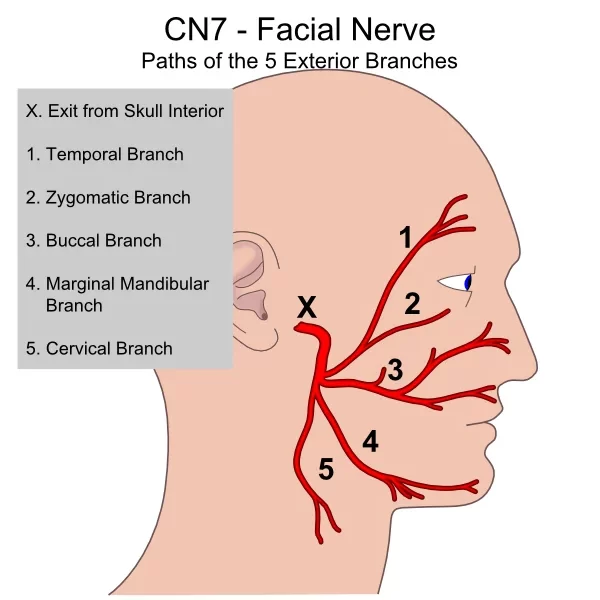
As the nerve exits the stylomastoid foramen it gives off a sensory branch to part of the external acoustic meatus & tympanic membrane.
It then passes between the stylohyoid and digastric muscle and enters the parotid gland, where it lies between the deep and superficial lobes of the gland. Here it divides into two main branches (at the pes asnerinus): superior temporofacial and inferior cervicofacial branches.
From the anterior border of the gland, 5 branches emerge:
1.temporal
2.zygomatic
3.buccal
4.mandibular
5.cervical
Within the parotid gland, the facial nerve terminates by bifurcating into five motor branches. These innervate the muscles of facial expression:
Temporal branch – Innervates the frontalis, orbicularis oculi and corrugator supercilii
Zygomatic branch – Innervates the orbicularis oculi.
Buccal branch – Innervates the orbicularis oris, buccinator, and zygomaticus muscles.
Marginal Mandibular branch – Innervates the mentalis muscle.
Cervical branch – Innervates the platysma.
Function of Facial nerve:
Facial expression:
The main function of the facial nerve is motor control of all of the muscles of facial expression. It also innervates the posterior belly of the digastric muscle, the stylohyoid muscle, and the stapedius muscle of the middle ear. All of these muscles are striated muscles of branchiomeric origin developing from the 2nd pharyngeal arch.
Facial sensation:
In addition, the facial nerve receives taste sensations from the anterior two-thirds of the tongue via the chorda tympani.
Testing of Facial muscles:
Motor Function:
FRONTALIS: Ask the patient to look up or wrinkle the forehead; inspect for asymmetry.
ORBICULARIS OCULI: Ask him or her to close her eyes tightly. Look for incomplete closure or incomplete “burying” of the eyelashes on the affected side.
NASALIS: Observe the nasolabial folds and mouth while the patient is concentrating on the eyes. As the orbicularis oculi contract tightly, there are milder associated contractions of muscles about the mouth and nose; these milder contractions are better suited to displaying slight weakness than when these muscles are tested directly.
ORBICULARIS ORIS: Ask the patient to smile, show teeth, or pull back the corners of the mouth. Look for asymmetry about the mouth.
BUCCINATOR: ask the patient to whistle and observe if air comes out or not.
Sensory:
The four primary tastes are bitter, sweet, sour, and salty. Screen for disorders of sweet or salty taste with salt and sugar. With the patient’s eyes closed and tongue protruded, take a tongue blade and smear a small amount of salt or sugar on the lateral surface and side of the tongue. Instruct the patient to tell you the identity of the substance. Rinse the mouth thoroughly and repeat the test on the other side, using a different substance.
Disorder of Facial nerve:
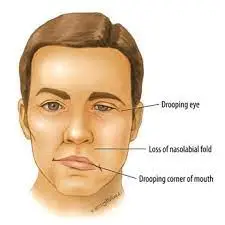
Facial Palsy:
People may suffer from acute facial nerve paralysis, which is usually manifested by facial paralysis. Bell’s palsy is one type of idiopathic acute facial nerve paralysis, which is more accurately described as a multiple cranial nerve ganglionitis that involves the facial nerve, and most likely results from viral infection and also sometimes as a result of Lyme disease. Iatrogenic Bell’s Palsy may also be a result of an incorrectly placed dental local anesthetic (Inferior alveolar nerve block). Although giving the appearance of a hemiplegic stroke, effects dissipate with the drug. When the facial nerve is permanently damaged due to a birth defect, trauma, or other disorder, surgery including a cross facial nerve graft or masseteric facial nerve transfer may be performed to help regain facial movement.
Diagnosis:
-Electromyography (EMG): This test can confirm the presence of nerve damage and determine its severity. An EMG measures the electrical activity of a muscle in response to stimulation and the nature and speed of the conduction of electrical impulses along a nerve.
-Imaging scans: Magnetic resonance imaging (MRI) or computerized tomography (CT) may be needed on occasion to rule out other possible sources of pressure on the facial nerve, such as a tumor or skull fracture.
Treatment of Facial Palsy:
Medication:
Commonly used medications to treat Bell’s palsy include:
-NSAIDs – Non-steroidal Anti-Inflammatory Drugs such as Aceclofenac, Diclofenac
-Corticosteroid medicine mainly prednisone, are a powerful anti-inflammatory agent. Corticosteroids may work best if they’re started within several days of when your symptoms started, however, it has side effects recommended only when NSAIDs are not working in a severe form of Facial Palsy.
Antiviral drugs: The role of antivirals remains unsettled. Antivirals alone have shown no benefit compared with placebo. Antivirals added to steroids are possibly beneficial for some people with Bell’s palsy, but this is still unproven.
Physical Therapy:

Paralyzed muscles can shrink and shorten, causing permanent contractures. A physical therapy treatment can help teach you how to massage and exercise your facial muscles to help prevent this from occurring.
Surgery:
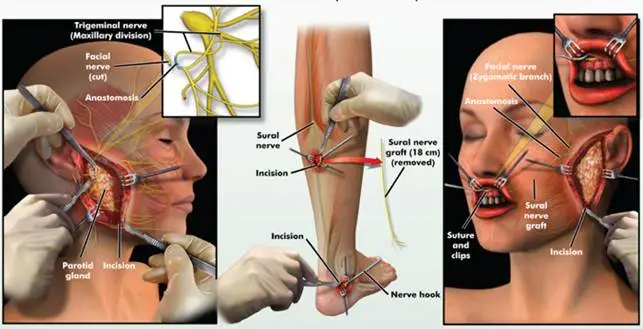
decompression surgery was used to relieve the pressure on the facial nerve by opening the bony passage that the nerve passes through.
Home Treatment:
-Protecting the eye you can’t close. Using lubricating eye drops during the day and an eye ointment at night will help keep your eye moist. Wearing glasses or goggles during the day and an eye patch at night can protect your eye from getting poked or scratched.
-Taking pain reliever medicine such as Aspirin, ibuprofen (Advil, Motrin IB, others) or acetaminophen (Tylenol, others) may help ease your pain.
-Doing your physical therapy exercises. Massaging and exercising your face according to your physical therapist’s advice may help relax your facial muscles.





I’ve had bels palsy for 9 years now, I have a lot of twitching constantly going on in my face and a lot of pressure behind my eyebrow. I have tried everything from acupuncture to chiropractic techniques and I’ve taken every kind of vitamin recommended for this disorder. Is there anything else I can due to overcome this paralysis? Thank you