Chronic Ankle Instability
Table of Contents
What is a Chronic Ankle Instability?
One of the persisting problems following an ankle sprain injury, especially a lateral ankle sprain (LAS), is chronic ankle instability (CAI). According to estimates, 40% of those who have a LAS go on to acquire CAI. Chronic ankle instability is characterized as the persistence of post-injury symptoms for more than six months after the initial injury, including swelling, diminished strength, instability (occasional giving way), and altered balancing responses.
Increased ligamentous laxity, proprioceptive deficits, activity constraints that influence the ability to perform tasks like walking or leaping, occupational and sporting restrictions, and other effects on ankle structure and function are only a few of the effects of CAI. Reduced range of motion, subsequent tissue damage, and limitations in osteokinematics may all occur in people with chronic ankle instability.
It may lower the quality of life, discourage people from exercising, and promote post-traumatic osteoarthritis. People with CAI also tend to be “ankle sprain copers” and have greater injury-related worry levels than the general population. These related issues might linger for many years.
Following a unilateral ankle sprain, up to 72% of patients are unable to regain their prior level of function, and 85% of those with CAI experience issues with the opposite ankle.
People with Chronic ankle instability have limited osteokinematics, post-traumatic osteoarthritis, reduced range of motion, and subsequent tissue damage in the ankle structure. Proprioception, balance, movement pattern, muscular weakness, and a bilaterally altered H-reflex are all consistently affected by CAI.
Definition of Chronic Ankle Instability (CAI)
Chronic ankle instability is a condition characterized by the recurring giving way or feeling of instability in the ankle joint. It often occurs after a previous ankle sprain or injury that did not heal properly or was not rehabilitated effectively. This condition can lead to functional limitations, decreased quality of life, and a higher risk of future ankle injuries.

Chronic ankle instability (CAI) is described as “repetitive bouts of lateral ankle instability resulting in numerous ankle sprains.” Chronic instability is defined as a feeling of discomfort in the ankle, a “giving way” sensation, and recurring ankle sprains that last for at least six months after the original injury.
These signs include: Ankle lateral pain, persistent swelling, Having trouble walking on uneven ground
Impairments include: Increasing ligamentous laxity, impairments in proprioception
Limitations on activities are as follows: being unable to walk, being unable to jump.
In terms of involvement:
Stop playing sports
reduction in or withdrawal from professional activity
lowering workout levels
Modification of the sport
Long-term Outcomes:
Patients with Chronic ankle instability report a decline in their level of physical well-being. Treatments may increase stability, but they are time-consuming and may need specialist tools. followed up with individuals seven years after ankle inversion injuries. What are discovered was:
32 percent of patients complained of ongoing discomfort, edema, or repeated sprains.
72% of the participants with residual impairment claimed that their ankle was a functional hindrance.
4% of patients had significant disabilities and discomfort when at rest.
19% of people experienced persistent inversion injuries.
43% of those surveyed said utilizing an external ankle support would help them make up for it.
85% of those who get CAI following a unilateral sprain reported issues in the opposite ankle.
Furthermore, sprains were shown to reoccur 30% of the time within a year after the initial injury.
Long-term effects that have also been observed include:
Articular cartilage abnormalities on the medial side of the joint as a result of:
Tearing of the anterior talofibular ligament
and the calcaneofibular ligament
peak cartilage strain may be changed and elevated
This eventually results in OA of the tibiotalar cartilage.
Deficiency in anterior talar location:
Changes in ankle stability’s movement patterns:
Attempting to reduce reliance on the lateral ligaments and boost bone stability by landing with increased dorsiflexion.
Greater maximal calcaneal eversion and body frontal displacement during a drop jump.
Peak ground response force in a drop landing occurs more quickly.
Additional medial ground reaction force.
The final swing of gait results in a reduction in metatarsal height.
Symptoms of Chronic ankle instability:
- Recurrent Ankle Sprains: Individuals with chronic ankle instability often experience repeated ankle sprains. These sprains may occur with relatively minor activities, such as walking on uneven ground or stepping off a curb.
- Feeling of Giving Way: One of the hallmark symptoms is a frequent sensation that the ankle is “giving way” or “rolling.” This can happen during weight-bearing activities, causing the person to lose their balance.
- Chronic Pain: Pain may be a constant or intermittent symptom. It can occur on the outside (lateral) or inside (medial) of the ankle and may be associated with previous injuries or inflammation.
- Swelling: Swelling of the ankle joint, particularly after physical activity or an episode of instability, is common.
- Weakness: Individuals with chronic ankle instability often report a feeling of weakness or lack of control in the ankle joint. This sensation may be especially noticeable when trying to perform activities that require balance and stability.
- Stiffness: Some people experience stiffness in the ankle joint, particularly in the mornings or after periods of rest.
- Decreased Range of Motion: Limited mobility in the ankle can be a symptom of chronic instability, making it difficult to move the ankle through its full range of motion.
- Tenderness: The ankle may be tender to the touch, especially in areas where previous injuries have occurred or where ligaments are stretched or damaged.
- Instability on Uneven Surfaces: An increased sense of instability may be felt when walking on uneven surfaces or navigating obstacles.
- Fatigue: The muscles around the ankle may become fatigued more quickly, leading to a sense of tiredness or heaviness in the affected leg.
Types of Chronic Ankle Instability
The following are some examples of how CAI affects function and health according to the International Classification of Function, Health, and Disability (ICF) model:
The subcategories of Chronic ankle instability that are most well-acknowledged are mechanical instability and functional instability. Mechanical and functional instability are two sides of a continuum in Hertel’s model of ankle stability. When both circumstances exist, sprains recur often.
1. Mechanical instability:
The ankle joint complex has pathologic ligamentous laxity, which is referred to as mechanical instability. Thirty percent of individuals who have MI experience ligamentous laxity after their initial ankle sprain.
MAI is caused by:
- ligament instability
- degenerative and or chronic inflammatory process
MAI is presented as:
- excessive inversion
- laxity of the rear foot
- excessive anterior laxity of the talocrural joint
2. Functional instability:
Functional ankle instability has no accepted definition that applies everywhere. According to Evans et al.’s definition, functional instability is a self-reported feeling of weakness. Functional instability is defined by Lentell et al. as ankle discomfort and the idea that the damaged ankle is less functional than the other ankle or less functional than it was before the injury. Functional instability, according to Tropp et al., can be described as a joint motion that is still under voluntary control but does not go beyond normal physiologic limitations.
Recurrent ankle sprains and a constant feeling of instability (giving way) are symptoms of functional instability in individuals. The ankle would move normally throughout the assessment and would have negative ligament laxity. To put it another way, it will be the individual who reports their own symptoms, such as pain and weakness, and who feels that their damaged ankle is less functional than the other. Numerous reasons, including muscular weakness, irregular muscle recruitment, reduced ankle range of motion, balance issues, poor sensorimotor function, and impaired joint proprioception, might be the cause of the persistent sense of instability.
FAI results in:
- sense of giving way
FAI is caused by:
- delayed neuromuscular response
- proprioceptive deficits
- impaired balance
Excessive inversion, laxity of the back foot, and excessive anterior laxity of the talocrural joint are common manifestations of mechanical instability. Ligament instability or a persistent inflammatory degenerative process may be the reason. On the other hand, individuals with functional instability complain of feeling their ankles give way. This symptom may be brought on by a delayed neuromuscular response, proprioceptive impairments, or unstable balance.
The majority of patients have both mechanical and functional instabilities when they first arrive. To distinguish between the two categories based on symptoms and physical test results is a hot topic in the literature. Whether or not MI was present, abnormalities in postural stability were discovered in a group diagnosed with FI. Another research looked at the peroneal response timings following inversion disturbance and found that people with FI alone had longer durations.
People with CAI have limited osteokinematics, post-traumatic osteoarthritis, reduced range of motion, and subsequent tissue damage in the ankle structure. Proprioception, balance, movement pattern, muscular weakness, and a bilaterally altered H-reflex are all consistently affected by CAI.
The Development of Chronic Ankle Instability:
A focal point that sets off a chain of following events when it happens. An interaction of innate and external risk factors affects this focus point. In a sporting event or routine everyday activity, intrinsic variables like old age, poor neuromuscular control, trauma history, etc. may combine with external factors to predispose a person or an athlete to injury. This individual won’t be injured since they have enough neuromuscular control, flexibility, and strength.
On the other hand, the likelihood of injury may increase if these conditions are not met. If this happens, the likelihood of healing or re-injury will depend on the combination of internal and extrinsic variables once more. Recognizing this process has significant implications for determining risk factors and creating rehabilitation plans.
Investigators have looked at the mechanism of CAI after an acute ankle injury to find risk variables and understand how they affect healing. Various functional limits and impairments after two weeks, six months, and one year after a first Lateral ankle sprain injury. Their investigation identified a variety of sensory abnormalities that physicians may use to assess the likelihood that CAI will develop. However, it is still unclear whether these deficiencies existed before the injury or whether they appeared as a result of it.
Sensorimotor Deficits Associated with CAI
Injury to the ligamentous structure results in more than just anatomical limitations. There is a wide range of symptoms and restrictions. It is hypothesized that structural deficiencies, such as changes in ligamentous tensile strength, disturb afferent-efferent communication, resulting in problems with peripheral manifestation of central control.
a motion capture system was used to examine the kinematics and kinetics of the LL during the acute stage following a first LAS injury. To evaluate static postural control, the single-limb standing test was used. The Star Excursion Balance Test (SEBT) was used to assess dynamic postural control and examine LL kinematics and kinetics, maximal hip-knee-ankle flexion-extension moments, and reach lengths in the anterior, posterolateral, and posteromedial directions. The Cumberland Ankle Instability Tool and the Foot and Ankle Ability Measure were two self-reported assessments that participants also completed in addition to landing and drop vertical exercises, gait analysis tasks, and other tasks.
The individuals were separated into two groups: the Cumberland Ankle Instability Tool (CAI) group and ankle sprain copers and the tests were repeated six months later and a year later.
The following deficiencies have been linked to acute ankle sprains and chronic ankle instability, according to these studies and others:
Static Postural Control Deficits:
In those with CAI more frequently. They appeared as a connection between frontal plane ankle motion and sagittal plane hip motion, indicating that the damage had resulted in the development of a hip strategy. Despite having been previously documented in chronic phases, this discovery is new for acute Lateral ankle sprain.
Participants in this single-limb standing test used the hip-dominant technique rather than the ankle-dominant method to maintain their postural balance while their eyes were open and when they were closed. The range of motion in the hip joint increased as a result.
As a result, following a LAS, it becomes challenging for the person to use each part of the kinetic chain independently; as a result, they become “locked” to give stability. The researchers also expressed uncertainty as to whether this ‘locking’ pattern existed in these people prior to the strain.
Dynamic Postural Control Deficits:
In all orientations showed that decreased hip-knee flexion moment and ankle dorsiflexion, although the reach lengths were only decreased in the posterolateral and posteromedial directions. It’s interesting to note that the abnormalities seen bilateral, supporting the idea that LAS may also appear centrally in addition to its peripheral symptoms. These signs and symptoms persisted for two weeks, six months, and a year after the accident.
Gait Deficits:
Biomechanical changes occur in those who have CAI. During the gait analysis test, they demonstrated a reduction in push-off tendencies, which appeared as decreased hip extension and greater ankle displacement in the frontal plane.
Deficits in Jumping and Landing Tasks:
The following were noted during landing and jumping tests: hip stiffness and bilaterally increased extension moments during landing; bilateral increases in hip flexion before initial contact (preparation for landing); and inter-limb asymmetries. The higher vulnerability to contralateral damage may be explained by the inclination to offload the injured limb and shift the strain to the unaffected side, as seen by the greater asymmetry.
These deficiencies were observed in people with CAI who had both acute and subacute stages of these problems. This is in reference to the theory that these deficiencies are causing Chronic Ankle Instability to develop. It is still unclear, though, whether these deficiencies led to the damage in the first place or whether they emerged as a result of the injury. Future research is required to pinpoint the risk variables for LAS using a follow-up design that enables us to connect these risk factors to the emergence of CAI or their role in recovery.
Predicting CAI
According to research by Doherty et al., doctors can anticipate the onset of CAI in the acute and sub-acute stages following a first ankle sprain if the following conditions exist.
inability to do duties requiring jumping and landing within two weeks after the injury. By 67.6%, these tasks were successful in predicting the emergence of CAI. These tests were reported to have an 83.3% sensitivity and a 55.3% specificity.
With better sensitivity and specificity (75 and 91%, respectively), hip and knee flexion in the posterolateral and posteromedial directions on the SEBT at six months after LAS damage was able to predict CAI by 84.8%.
On the Foot and Ankle Ability Measure, the self-reported function was worse.
Prevention Strategies:
The condition, which is widespread in athletes and other people who lead sedentary lifestyles and may have a significant negative impact on performance, makes CAI prevention crucial. Four pillars serve as the foundation for the preventative techniques that will be covered below.
- Evaluation of all the injured joints
- Techniques for addressing hypermobility
- The restoration of hypomobility
- Protecting the healing structures.
The lateral joint capsule of the ankle and the ligaments supporting the lateral talocrural, subtalar, distal, and proximal tibiofibular joints are among the structures that prevent excessive inversion and supination as a result of the mechanism of ankle sprain damage. As a result, one or more of these joints will either become hypo or hypermobile.
Hypermobility, Increased joint play motion leading to aberrant movement patterns on the instantaneous axis of rotation (IAR) of the joint with physiologic movement is a sign of hypermobility, ligamentous laxity, or mechanical instability. The fundamental cause of increased laxity following ligament sprains or tears is that the healing process was insufficient to restore the previous tension, altering proprioceptive input from excessively stressed tissues and requiring the use of compensatory motor movements. Ligament injury is what causes the overpronation or unstable mortise that is seen.
The cervical and interosseous ligaments have both been identified as the cruciate of the subtalar joint. Due to the persistent laxity after the accident, it is thought that these two ligaments were injured in an ankle sprain. Early loading of damaged cervical and interosseous ligaments may disrupt the healing process and cause the ligaments to recover in a lengthened posture since their purpose is to restrict end-range pronation and supination. Therefore, to enable regeneration at a more ideal length following ankle injury, many doctors advise restricting pronation by using an orthotic device.
Hypomobility, On the other hand, hypomobility can cause joint instability by changing the lower extremity’s kinetic chain after LAS. Hypomobility, whether it be physiologic or accessory, alters movement patterns, causing aberrant stresses and altered proprioceptive input. At the subtalar joint, talocrural joint, distal tibiofibular joint, or proximal tibiofibular joint, hypomobility may be seen. In order to recover ankle dorsiflexion, various rehabilitation techniques combine mobilization with mobility and ROM exercises.
Limited dorsiflexion is frequent after LAS. It can be due to capsular adhesion or tightness in the gastrocnemius-soleus. However, the accessory motion may be restricted, but the physiological movement is retained by compensation mechanisms from nearby regions. When DF is restricted at the talocrural joint, for instance, a vertical limp during walking can be achieved to preserve the forward motion of the lower leg.
Hypomobility, which Meadows defines as “a biomechanical problem with the joint jamming at one end of the range of motion and blocking movement away from that range,” may also be caused by subluxation or malposition of the talus. It happens as a result of the talus’s anterior displacement brought on by excessive inversion. If held in situ, the torn anterior talofibular ligament heals in an extended position and lacks the mechanical integrity that prevents the talus from moving anteriorly. The result is reduced dorsiflexion and limited posterior glide.
Patients who have had LAS and those who are more likely to develop CAI should be screened for both hypo and hypermobility, and measures to manage both problems should be incorporated into the rehabilitation.
The degree of function isn’t always indicative of the ankle joint complex’s best possible recovery after LAS. Therefore, the rehab staff shouldn’t quicken the course of therapy. Preventing overload and aberrant tissue stress involves keeping an eye on the load placed on the afflicted tissues and keeping an eye out for inflammation.
Joint stability techniques and normalized joint mechanics should be used in rehab in addition to a gradual increase in load to prevent further CAI. In terms of avoiding CAI, a rehabilitation program created to address the consequences of injury on the ankle joint complex may show promise.
Clinically Relevant Anatomy
Ankle sprains are a frequent sports injury, and 20% of people who have an acute ankle sprain go on to develop chronic ankle instability. The anterior talofibular ligament (ATFL), calcaneofibular ligament (CFL), and/or posterior talofibular ligament (PTFL) are injured in two million lateral ankle sprains each year in the US. This indicates a significant risk of recurrence and permanent impairment.
Deficits in postural control, proprioception, muscular reaction time, and strength are frequently seen after an acute ankle injury and can result in chronic ankle instability (CAI). An ultimate CAI result was predicted by the inability to perform leaping and landing exercises within two weeks of a first lateral ankle sprain (LAS), as well as by poorer dynamic postural control and lower self-reported function six months after a first LAS. Both functional instability (objectively stable with subjective sensations of instability owing to sensory or neuromuscular impairments) and mechanical instability (motion beyond normal physiological limits) are included in CAI.
Clinical Presentation:
Patients with chronic ankle instability typically have a history of severe inversion injuries as well as recurring ankle sprains in the past. They take extra care to avoid activities like weight carrying, intense activity, and walking on uneven terrain.
A spectrum of deficiencies that may be assessed using a number of sensorimotor assessments comprise CAI. Ankle instability is clearly accompanied by conscious afferent somatosensory information reception, reflex responses, and efferent motor control deficits. We still don’t completely understand the precise cause of these deficiencies local to the ankle ligaments or at the spinal or supraspinal levels of motor control. However, it is evident that ankle instability affects both the feedforward and feedback systems of motor control.
Invertor and evertor muscle weakness, together with a decline in proprioceptive capacities brought on by the loss of mechanoreceptors, have been identified as the two primary causes of chronic ankle instability. When a lateral ankle sprain (LAS) occurs, different mechanoreceptors in the joint capsules, ligaments, and tendons around the ankle complex also sustain damage in addition to the structural integrity of the ligaments. These receptors work as a group to provide input on joint pressure and tension, which in turn allows for the perception of joint movement and position.
This data is combined with the vestibular and visual sensory systems via afferent nerve fibers to generate a sophisticated control system that affects posture and coordination. After an injury, afferent input may change, which may change the way that muscles contract to fix the problem. Thus, functional limitations and ongoing instability after an initial injury may be caused by LAS damage to the mechanoreceptors around the ankle joint.
Proprioception
According to some descriptions, mechanoreceptors found in the skin, ligaments, muscles, tendons, and joint capsules provide sensory data to the brain’s central nervous system, which is the source of proprioception. Ligamentous tissues that contain mechanoreceptors may partially differentiate as a result of trauma, which may cause proprioceptive deficiencies and ultimately contribute to CAI. After acute LAS and in those with CAI, postural-control abnormalities during quiet standing have frequently been described.
Muscle weakness
Researchers have hypothesized that persistent ankle instability is associated with peroneal muscle weakening in addition to sensory impairments. If the evertor muscles are weak, they will be less able to avoid inversion sprain by resisting inversion and bringing the foot back to neutral. Patients with persistent ankle instability have been shown to have eccentric rather than concentric evertor weakening. Concentric invertor strength deficiencies in CAI patients have been reported by other researchers. The inversion weakness was explained by two different theories.
The capacity of the ankle invertors to begin moving in the direction of the initial damage may have been selectively inhibited by reflex, to begin with. A second potential factor is deep peroneal nerve dysfunction brought on by excessive peroneal nerve stretching. Another argument they put out is that a lateral ankle sprain causes the motor neuron pool responsible for invertor muscle function to become less excitable, but the motor neuron pool responsible for evertor function is not significantly impacted.
Diagnostic Procedures:
Ligament flexibility is what causes mechanical ankle instability, but postural control deficiencies, neuromuscular deficits, muscle weakness, and proprioceptive deficits are what produce functional ankle instability. The International Ankle Consortium has recently modified the selection criteria for chronic ankle instability, and there may be seven subcategories, including subjective instability, frequency of repeated sprains, and mechanical instability interaction.
During a physical examination, the strength of the peroneal muscles should be assessed as well as the hindfoot motion. It is important to look for ligamentous laxity symptoms. It is important to carry out stability tests like the anterior drawer and talar tilt test. Proprioception is frequently impaired in individuals with chronic ankle instability; grade III ankle sprains account for 86% of cases of peroneal nerve damage and 83% of cases of tibial nerve stretch injury. The modified Romberg test can be used to measure proprioception. The patient stands on the unaffected ankle while keeping their eyes open and then closing them, repeating the process with the afflicted ankle.
Clinicians can use diagnostic methods to confirm the existence of various ankle abnormalities, such as restricted range of motion and reported impairment. This can aid in defining or diagnosing a particular illness. Before selecting a diagnostic instrument, clinicians should think about whether study data indicate “consistent positive utility”:
Anterior drawer test: To relax the gastrocnemius, perform the anterior drawer test while slightly flexing your knees. To isolate the anterior talofibular ligament, Kovaleski et al. advise testing with the knee flexed to 90° and the ankle at 10° of plantar flexion. It is suggested to compare the two sides. A positive test result is indicated by excessive anterior translation and a weak terminal feel.
Stress radiography: used to measure the degree of laxity in the ankle joint. It demonstrates how the bony joint structures may separate as a force is applied. Clinically, it is useful to determine when the ligamentous tissues are being overstretched. When compared to the contralateral side, a total anterior translation higher than 9 mm or a translation larger than 5 mm (or both) suggests considerable anterior talofibular ligament laxity. A talar tilt angle higher than 10° or one that is more than 5° greater than the opposing limb is indicative of pathologic laxity of the calcaneofibular ligament.
MRI: The most beneficial MRI is for persistent ankle instability. On an MRI, a torn ligament may appear as edema, a fiber discontinuity, a slack or wavy ligament, or it may not be seen at all. To properly align the ATFL and CFL, the ankle should be in neutral or modest plantar flexion. Cost, availability, duration, motion artifact, and the inability to precisely predict chronic effects following acute damage are some of the limitations of MRI.
Diagnostic ultrasound: Evidence demonstrates that diagnostic ultrasonography provides a somewhat strong confirmation of lateral ligamentous damage. When doing the anterior drawer and talar tilt tests on those with a history of CAI, it reveals greater lateral ligament length.
Stable force plates: a suggestion for testing hop stability and gait.
Cortisone injections with image guidance are used as a clinical diagnostic technique. The European Society of Musculoskeletal Radiology’s Delphi-based consensus of specialists discovered that intraarticular foot and ankle anesthetic injections administered under imaging guidance offer accurate information regarding the cause of pain.
Outcome Measures:
Patient Report
Lower Extremity Functional Scale (LEFS):
Measurement of “patients’ initial function, ongoing progress, and outcome” for a variety of lower-extremity diseases is the goal of the Lower Extremity Functional Scale (LEFS).
For usage with individuals who have lower extremity problems, the LEFS is designed.
Method of Use: Patients choose a response from the following scale for each of the mentioned activities:
Unable to Perform Activity or Extreme Difficulty
A Good Amount of Difficulty
somewhat challenging
A Modest Amount of Difficulty
No Challenge
The patient’s score is totaled at the page’s bottom. 80 points is the highest attainable score and denotes an extremely high function. The lowest possible score is 0, which represents an extremely poor function.
Foot Function Index (FFI):
The FFI has been demonstrated to be a useful instrument for use with rheumatoid arthritis patients, poor-functioningFoot and Ankle Ability MeasureFoot and Ankle Ability Measure people with foot illnesses, and those who have non-traumatic foot or ankle issues. It is applicable to both clinical and academic contexts.
However, it might not be ideal for those who do daily life tasks independently or better.
Method of Use:
23 self-reported elements make up the FFI (questionnaire), which is organized into three areas based on patient values: pain, disability, and activity restriction. The patient must rate each question according to how well it depicts their foot during the last week on a scale from 0 (no pain or difficulty) to 10 (worst pain conceivable or so bad it requires help).
Nine questions make up the pain subcategory, which assesses foot discomfort in various contexts, such as when wearing shoes or being barefoot.
The disability subcategory has nine items that assess how difficult it is to execute various functional activities due to foot issues, such as how difficult it is to climb stairs.
The five elements that make up the activity limitation subcategory assess limitations in activities brought on by foot issues, such as spending the entire day in bed. Scores are recorded using a visual analog scale (VAS), with lower scores indicating less pain and higher scores indicating greater discomfort. Scores are computed for both the overall category and subcategory.
Foot and Ankle Ability Measure:
A self-report outcome tool called the Foot and Ankle Ability Measure (FAAM) was created to evaluate physical function in people with foot and ankle-related disabilities. There are translations of this self-report outcome tool available in Persian, English, German, and French. The Foot and Ankle Ability Measure is a 29-item questionnaire with two subscales: the Activities of Daily Living Subscale, which consists of 21 items, and the Sports Subscale, which consists of 8 items. The Sports subscale, a population-specific subscale created for athletes, evaluates more challenging activities that are necessary for athletics.
Except for the additional 5 items included on the FADI, the FAAM, and the FADI are identical. The Foot and Ankle Disability Index’s four “pain-related” elements and a person’s capacity for sleep have been eliminated. The FAAM’s Sports subscale is identical to the FADI’s Sports subscale.
Each item is rated on a 5-point Likert scale (4 to 0), with ‘no difficulty at all’ denoting the easiest option and ‘unable to accomplish’ denoting the most difficult. The item score totals, which for the ADL subscale range from 0 to 84 and for the Sports subscale from 0 to 32, were converted to percentage scores. For each subscale, greater scores indicate better levels of function, with 100% denoting no dysfunction.
(level 1) came to the conclusion that the FADI and FAAM were the best patient-assessed instruments for assessing functional limitations in patients with chronic ankle instability, but they also noted that more research on the FAAM in a particular group of CAI patients is required.
Method of Use:
Sports and ADL subscales receive different scores.
Each response on the ADL subscale is given a score between 4 and 0, with 4 denoting “no difficulty” and 0 denoting “unable to do.” Responses with an NA are not counted. The item score total is calculated by adding the scores for each of the things. The maximum possible score is calculated by multiplying the total number of items with an answer by 4. The best possible score is 84 if the person responds to all 21 questions. The highest score is 80 for unanswered questions, 76 for unanswered questions overall, etc. The greatest possible score is divided by the sum of the item scores. To obtain a percentage, multiply this figure by 100. More physical function is indicated by a higher score.
Cumberland Ankle Instability Tool:
A 9-item, 30-point scale known as the Cumberland Ankle Instability Tool (CAIT) assesses the degree of functional ankle instability. The CAIT may distinguish between stable and unstable ankles using a numerical value.
Method of Use:
Patients are able to assess the perceived level of difficulty associated with carrying out various physical activities using this self-report questionnaire. It is feasible to evaluate each ankle separately by completing the CAIT for both the left and right ankles. The injured ankle or ankles must be checked off just one statement in each item.
Scoring
The CAIT’s nine questions result in a final score of 30.
Extreme functional ankle instability: 0 points
Thirty points: a healthy ankle
Recent research reveals that a cutoff score of 25 resulted in enhanced test features, increasing the tool’s accuracy in distinguishing between those with and without chronic ankle instability. The initial study set a cutoff value of 27.
Objective Tests
Star Excursion Balance Test
Dynamic tests like the Star Excursion Balance Test (SEBT) call on proprioception, flexibility, and strength. For athletic and physically active people, it is a test of dynamic balance that poses a substantial challenge. The test can be used to evaluate physical performance, but it can also be used to identify athletes who are more likely to sustain lower extremity injuries, to screen for deficits in dynamic postural control caused by musculoskeletal injuries (such as chronic ankle instability), and to monitor orthopedic injury rehabilitation in healthy active adults.
The SEBT has been discussed and tested as a tool for testing dynamic postural control in the lower limb, detecting functional deficiencies in the return to sport phase, and identifying those who are at high risk for future injuries.
Technique:
There is some preparation work that must be done before the SEBT can be performed. Cut four pieces of athletic tape to a length of 6 to 8 feet apiece. Two pieces will be used to create a “+,” and the other two will be positioned on top to create a “x,” creating a star shape. All lines must have a 45° angle separating them from one another. The SEBT’s objective is to maintain a single-leg stance on one leg while extending the opposing leg as far as feasible.
The test subject is required to balance on one leg while extending the other leg as far as they can in eight different directions. The participant must reach in 8 distinct postures, once in each of the following directions: anterior, anteromedial, medial, posteromedial, posterior, posterolateral, lateral, and anterolateral (for example, when standing on his or her left leg). Athletes who are more likely to sustain lower extremity injuries and people with chronic ankle instability may be better identified using the anterior, posteromedial, and posterolateral orientations.
The Star Excursion Balance Test has shown the person’s lack of dynamic postural control when they show a considerably reduced reach while standing on the damaged limb compared to standing on the healthy leg.
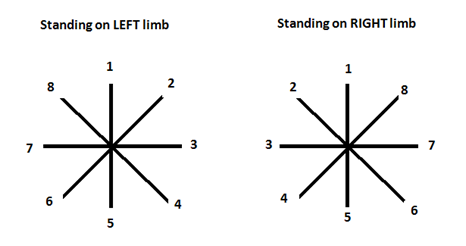
A factor analysis revealed that one reach direction in particular (posteromedial) was able to effectively identify those with chronic ankle instability as well as perform all eight directions. The test initially included reaching in eight directions while standing on each foot.
Y Balance Test
A method for determining an individual’s risk of damage is the Y Balance Test (YBT). It can be used for the upper and lower quarters. As its methodology is based on research on the Star Excursion Balance Test, the YBT for the Lower Quarter (LQYBT) has undergone extensive investigation. In high school basketball players, the Star Excursion Balance Test reliably predicted LE injuries, while the LQYBT has identified athletes at higher risk for injuries.
Technique:
It has been established that the YBT for the UQ (UQYBT) is a valid test for evaluating unilateral UE function in a closed chain situation. The UQYBT additionally requires the patient to do three separate UE reaches while in the push-up posture. To evaluate if the UQYBT is applicable, more study is required.
Treatment of Chronic Ankle Instability
The degree of ankle instability and the patient’s level of activity will determine the course of treatment.
To determine the best course of action, it is crucial to distinguish between functional and anatomical ankle instability. Chronic ankle instability may necessitate surgical intervention, in contrast to acute ankle sprain. For individuals with persistent ankle instability, nonsurgical treatment is strongly advised before doing any surgical surgery. Orthotics should be given if necessary, along with neuromuscular and proprioceptive training, during the rehabilitation phase.
Exercises that improve proprioception, balance, and functional ability are frequently done after an ankle joint injury in addition to strengthening the muscles since research has shown that recurrent ankle joint injuries produce neuro-sensorial, proprioceptive, and mechanical deficits.
Conservative Management:
Medicine
It could be advised to use anti-inflammatory medications like ibuprofen or naproxen.
A topical lotion or other mild painkillers like paracetamol may also be utilized.
Balance training
Reduced postural control, reduced awareness of joint position, and greater instability are issues seen in CAI patients. These issues are assumed to have their roots in altered sensorimotor system function. A crucial component of the current CAI recovery procedures is balance training. On the sensorimotor deficiencies typical of CAI, such as postural control, dynamic balance, joint position perception, and segmental spinal reflexes, the benefits of balance training have been identified. A great balance rehabilitation activity for CAI has been recommended, the Star Excursion Balance Test.
Progressive loading
It has been demonstrated that isokinetic muscle training improves ankle proprioception, muscular strength, and functional ability.
Braces
Individuals with CAI should wear a brace for high-risk activities like returning to sports for six months after an ankle sprain. Individual requirements such as dependence risk, probability of proper usage, cost, etc., should be taken into account.
Surgical Intervention
Surgery should be taken into consideration when bracing and taping techniques are ineffective in supporting chronically unstable ankles that repeatedly fail to heal. By using tendon grafts or nearby tissues, the damaged ligaments are restored surgically. The Broström treatment, one of the surgical techniques, largely restores the torn ligaments. A tendon transfer is used to supplement the original repair in order to increase stability and protect the repair. To identify and treat ankle instability, arthroscopy is available to assist.
Associated lesions:
Lesions that develop from contributing variables are frequently linked to lesions that cause chronic ankle instability. They don’t often accompany persistent ankle instability, and even when they do, not all of these lesions manifest at once. Chronic regional pain syndrome, neuropraxia, sinus tarsi syndrome, peroneal tendinopathy, dislocation or subluxation, impingement syndromes, fractures of the anterior calcaneal process, fibula, and lateral talar process, loose bodies, and osteochondral lesions of the talar dome or distal tibia are some of the associated lesions that are associated with chronic ankle instability.
Sinus Tarsi Syndrome:
Dancers, basketball and volleyball players, as well as obese persons, frequently get sinus tarsi syndrome. Additionally, people with flatfoot and hyper-pronation abnormalities frequently experience it. It is characterized by discomfort and sensitivity in the sinus tarsi, or lateral side of the back foot. It might happen after one ankle sprain or several. Despite the possibility that magnetic resonance imaging might reveal signs of inflammation, the diagnosis is made by exclusion. Primary repair of the ligaments in the sinus tarsi, tendon augmentation, or both are used to treat sinus tarsi syndrome.
Osteochondral Defects:
Talus injuries are known as osteochondral defects (OCD). They might include bone layers and cartilage fractures as well as bone-layer blistering and cyst-like abnormalities inside the bone. OCD can come from a single stressful event or repeated trauma. Osteochondral abnormalities show edema, instability in the ankle joint, and persistent discomfort. Uncertainty exists regarding the precise mechanism of both pain and instability. Depending on the kind, size, and location of the lesions, treatment is ideally effective.
Peroneal Tendinopathy:
Chronic inflammation of the peroneal tendon causes peroneal tendinopathy, which weakens the active ankle stabilizers. This occurs when a person engages in a repeated motion that irritates the tendon over time. Additionally, peroneal tendinopathy may be brought on by inadequate and quick training as well as harmful shoe wear. Peroneal tendinopathy is more common in people with a hindfoot varus posture. Although surgical debridement and promotion of healing, either open or endoscopically, are becoming more and more popular, conservative treatment is still used to treat the majority of peroneal tendinopathy patients.
Subtalar Instability:
The cause of the occurrence known as subtalar instability is unknown. It appears to have been misdiagnosed. It may exhibit signs of persistent ankle instability. Clinically, the inward rotation of individuals with subtalar instability has increased. It is treated with an anatomic ligament repair technique, a tendon transfer, or a tenodesis method like Chrisman-Snook.
Physiotherapy Management:
A surgical approach to treating acute lateral ankle injuries is only used in exceptional circumstances; conservative treatment is the preferred course of action. There are several conservative treatment options at this point:
- A neuromuscular workout
- Balance instruction
- Mobilization
- Peronei’s neuromuscular control (theraband and isokinetic exercise have little impact on ankle evertor strength)
- Taping and braces
- Strength- and flexibility-training
Neuromuscular Training:
Patients exhibited improved function and saw a favorable short-term result from neuromuscular training alone. A crucial component of the majority of conservative treatment regimens is this kind of training.
A somewhat inverted ankle posture is seen during first contact and midstance in athletes with unstable ankles, which results in an altered gait pattern.
The athlete’s ankle orientation during jump landing was promptly altered after six weeks of neuromuscular training to a substantially more inverted direction. However, running and walking had little impact.
College volleyball players with functional ankle instability (FAI) experienced greater postural control after undergoing four weeks of neuromuscular training.
Guide to Neuromuscular Training:
Neuromuscular training is the unconscious activation of dynamic restraints in preparation and response to joint motion and loads to maintain and restore functional joint stability.



Neuromuscular training objectives:
To improve lower-limb postural control
Training to regain active stability
Exercises:
Closed-chain and functional postures are used for the exercises:
1. Single limb stance on a wobble board or balance mat:
STARTING POSITION:
Stand tall with your feet shoulder-width apart. Put a balancing board beneath your right foot. Raise your one leg before you while keeping your right leg balanced. Bend your right knee slightly.
MOVEMENT:
Maintain your balance for the needed time and repeat with the other leg.
TIP: Keep your knees pointed towards your toes at all times. Maintain your weight on the whole soles of your feet at all times. Always keep your head and chest forward.
2. Single limb ball toss sideways:
STARTING POSITION:
1: Take both hands and grip a ball at your waist.
2: Face the wall with one side of your body.
3: Pick up the foot closest to the wall and stand on one foot only.
4: Turn at the waist and move the ball away from the wall before turning around and throwing the ball against it.
5: Catch the ball and continue this action for the appropriate number of repetitions before changing feet and switching sides.
A single-leg ball side throw is a calisthenics and pilates exercise that primarily focuses on the obliques and targets the abs, calves, and quadriceps to a lesser extent.
The only piece of single-leg ball side throw equipment you need is a medicine ball. There are, however, several single-leg medicine ball side throw variants that you may try out, some of which may require various sorts of single-leg ball side throw equipment or none at all.
3. Single leg theraband kicks and step downs:
Instructions:
Standing on one leg in a clear safe location, wrap the theraband around something substantial and then your ankle.
Try to maintain your balance while kicking your leg out in different directions.
The band will put your equilibrium to the test.
The goal is to avoid putting your other foot on the ground.
If this occurs, attempt to recover and continue with the activity.
Balance Training
While researching functional ankle instability and health-related quality of life, researchers discovered that balance training can benefit various joints and result in overall benefits.
Balance training improves both static and dynamic postural control dramatically.
Rehabilitation has an impact on sensorimotor system function.
Balance training significantly improves functioning, instability, and dynamic balance outcomes in persons with chronic ankle instability.
Guide to Balance Training
The following balancing metrics should guide therapeutic practice. However, no link with the function was discovered:
Excursion of the center of pressure (COP)
Time-to-boundary (TTB) after landing
Peak plantar analysis
SEBT (Star Excursion Balance Test)
Proprioception
Kinesthesia and joint position sensing (JPS) are typically compromised in chronic ankle instability patients. Proprioception testing methodology involves the following steps:
The threshold-to-detection of passive motion is used to measure kinesthesia.
Active and passive joint placement reproduction is used to test joint position sense.
Therapeutic Interventions
Once a week, perform a multi-station fitness routine:
Balance pad, ankle disc training
Experiment using elastic tubing for perturbation:
Three times each week, four workouts (front pull, back pull, crossover, and reverse crossover) are performed. The typical treatment consists of three sets of 15 repetitions of standing on the afflicted limb with a resistance band.
The goal is to keep alignment and stability.
In 4 weeks, the equilibrium improved.
Mobilization
Because of the following reasons, limited ankle dorsiflexion during running and walking gait is considered a risk factor for repeated sprains:
- Inability to attain the ankle joint’s closed-packed posture during stance
- Supination has a tendency to lock the midfoot.
- Because the center of gravity shifts laterally, the ankle joint becomes subject to supination and sprain.
MWM approaches for treating peripheral joints were superior to placebo but not to other medical or physiotherapy therapies.
Patients with chronic ankle instability benefited promptly from a mobilization with movement intervention by improving the dorsiflexion range of motion.
Therapeutic Interventions:
The following should be included in Mulligan’s mobilization with movement (MWM) technique:
- Fibular glide at the proximal and distal tibiofibular joints
- Talar gliding
Tibiofibular Joint:
Ventral glide at proximal tibiofibular joint:
Indications
To enhance mobility at the fibula’s head.
To repair the subluxated head’s positional flaw.
The patient’s position:
Side-lying with the trunk and hips rotated slightly towards prone lying.
The leg on top is bent forward to rest on the table or the pillow.
Hand placement and therapist posture
The therapist approaches the patient from behind and inserts one hand under the tibia to stabilize it.
The opposite hand is posterior to the fibula’s head, with fingers wrapping anteriorly.
Force of mobilisation:
The force is exerted anterolaterally with the heel of the hand.
Braces and Taping:
Athletic taping steps:
- Starting just behind the ball of the foot, wrap prewrap upward until the ankle (and about 3 inches above the ankle) is covered.
- Apply two anchor strips to the topmost area of the pre-wrap using athletic tape. Starting at the front of the leg, wrap the tape until the strips overlap by 1 to 2 inches. Apply a second strip halfway past where the previous one was.
- Apply the tape to the top of one anchor strip, advance it over the ankle, over the heel, and terminate at the same point on the opposite side of the leg to make a stirrup piece. This should resemble a stirrup.
- Repeat, but this time insert an extra stirrup piece somewhat more in the centre of the top of the foot, running around the ankle and allowing the tape to cling to the anchor strip.
- Wrap another anchor strip around the stirrup tape, about halfway from the beginning of the last anchor strip. This aids in the retention of the stirrup piece. Wrap in this manner until you reach the top of your foot.
- Wrap the heel in a figure-eight pattern. Bring the tape over the foot, angling down towards the heel, beginning on the inside part of the arch. Continue the figure-eight across the foot and ankle for two complete wraps. Finish by wrapping tape over the arch or heel of the lower leg and around the opposite side. Additional anchor strips may be required. There shouldn’t be any skin showing on you.
Kinesio taping steps:
- Start a piece of kinesio tape 4 to 6 inches above the ankle on the outside of the ankle. As you draw the tape over the heel, bring it to the opposite side, over the inside aspect of the ankle, and stop at the same level as the previous piece of tape to create a stirrup-like appearance.
- Place another piece of tape on the back of your foot, centered on the Achilles (heel) tendon. Wrap the tape over your ankle and around your foot. The tape should be snug enough that the foot flexes while feeling supported. Some individuals cross the tape around their ankles rather than circle it. This is accomplished by placing a strip of tape beneath the arch and bringing the two ends across the front of the lower leg to form an X. The tape ends are attached behind the leg.
Therapeutic Intervention:
The following taping techniques were clinically assessed:
- Subtalar inversion is combated with a lateral subtalar sling.
- Fibular repositioning, but the exact mechanism for reducing the incidence of sprains is unknown
- The muscle activation of the peroneus (fibularis) longus was unaffected by the Kinesio Taping Method’s use to avoid ankle sprains.
Flexibility and Strength Training:
Flexibility:
Stretching the soleus and gastrocnemius three times for 30 seconds each is a common belief in traditional flexibility exercises for chronic ankle instability. A new protocol recommends walking backward and performing plantar fascia stretches.
Stretching the flexor hallucis longus and the big toe with the neural roll-down and toe extension technique.
Strength:
On the discovered concentric evertor strength deficits:
- There is no connection between deficiencies and a decline in functional stability.
- difficult to identify evertor weakness
- Slow-speed isokinetic testing may maximize differences.
- Deficiencies of investors
Muscle co-contraction is crucial during strengthening activities. Treatment plans ought to contain:
- The calf raises on each side
- brief footwork drills
- Rehabilitation efforts ought to take strength into consideration.
Treatment Protocol:
The following is the recommended treatment plan for chronic ankle instability:
General Principles:
Setting goals is essential:
Group effort
The athlete carries the responsibility
- Talk about posture stability
- Include proximal stability, focusing on the hip and knee joints in particular.
- Concentrate on the foot’s and the ankle’s local stabilizers
- The goal is to regain the range of motion in dorsiflexion.
- Incorporate cardiovascular exercise
- Integrate workouts into the gym to increase adherence.
- Examine your shoes and your sport-specific technique.
Phase 1
Cardio-vascular fitness to include:
1. Cycling:
Ankle ligaments and muscles are strengthened by cycling. It lubricates the joint and aids blood flow around your ankles.
Cycling works every part of the lower body, from the hips to the ankles. Increase the effort as you become more utilized to the pedal motion to build stronger, more toned muscles.
Your ankles move constantly while you pedal, which strengthens and stretches the ligaments in your ankles. You have a lower chance of suffering ankle injuries as a result.
Cycling is a great workout to include in your everyday regimen. It develops its muscles without putting undue strain on your joints and enhances all lower body functions.
2. Hydrotherapy or swimming:
Swimming in a pool enables someone to walk much more quickly than on dry land during the acute injury stage. Exercises involving partial weight bearing are effectively performed in the buoyancy and anti-gravity of water. Hydrostatic pressure, in the first place, aids in reducing edema. Second, gait training in the water does not require the use of crutches or other assistive devices. Without these aids, the disabled person can walk normally and the affected muscles will fire on their own.
3. Walk:
- Backwards and forwards
- Step length; “Pink Panther”; heel-toe; big toe; foot placement; ladder;
Postural Control/ Balance exercises to include:
- Pilates:
Pilates is a form of exercise that focuses on improving core strength, flexibility, balance, and overall body awareness. While Pilates can be a valuable component of a rehabilitation or fitness program for many individuals, its role in managing chronic ankle instability (CAI) may be limited. However, it can be a complementary approach to improve overall strength, balance, and stability, which may indirectly benefit individuals with CAI.
Controlled movements and balance difficulties are frequent components of Pilates workouts. These exercises can help improve proprioception (the body’s sense of joint position) and enhance overall balance, which can be valuable for individuals with CAI who experience instability.
2. Ankle Mobility Exercises:

Ankle circle:
Lay down a foam roller or a towel that has been tightly coiled.
Your right knee should be bent as you sit on the ground with your left leg extended in front of you.
Place the towel or foam roller under your left leg, which is extended in front of you.
Slowly rotate your ankle ten times in a clockwise direction.
Reverse this action and slowly rotate your ankle ten times in an anticlockwise circular motion.
On the opposite leg, repeat the stretch.
On each side, carry out this stretch two more times.
Dorsiflexion:
Lifting your foot off the ground or bringing your toes closer to your body are two examples.
This movement is regulated by the tibialis anterior muscle, which is situated at the front of the lower leg.
Maintaining your heels on the ground while bringing your toes up towards your shins is how you dorsiflex. You do this motion when you walk and prepare to place your foot on the ground.
Plantar Flexion:
Plantar flexion is the term for the action of pointing your toes away from your body. Get comfortable standing on your toes.
Squeeze the balls of your feet together to do plantar flexion.
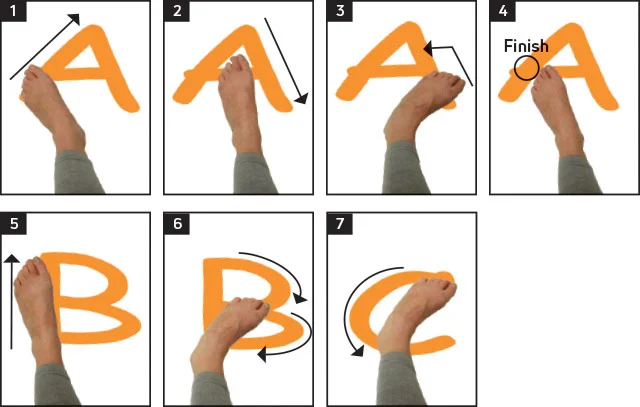
Ankle alphabet:
Place your feet flat on the floor while sitting on a chair.
Straighten out your damaged leg in front of you so that it is in the air.
Write the letters of the alphabet, from A to Z, on your big toe.
Repeat this exercise two or three more times if you experience no pain. If you do have pain, you should wait until your ankle is more robust.
Figure Eight rotation:
Similar to the toe movement exercise, the figure-eight rotation exercise involves rotating your toes in a figure-eight pattern as opposed to a circular one using your big toe. The main benefit of this exercise is that the toes and fingers of the foot become more flexible.
Repeat for 2-3 sets 10 times for each toe. Exercises like the Figure-8 rotation are extremely simple and fundamental.
3. Short foot exercises:
Take a seat and feet on the ground.
Keep your right foot in mind. Think about softly attempting to “shorten” the distance between your big toe’s base and your heel.
Your foot should develop a slight arch as a result of this action when the muscles on the underside contract.
Hold: Continue this contact for a short period of time, often 5 to 10 seconds.
Release: Let go of the tension in your foot muscles and permit your foot to regain its original posture.
4. Tibialis posterior re-education:

Strengthening exercises to include:
- Leg press
- Calf raises, theraband exercises
- Hamstring curls
- Bridging (glutes)
- Abdominal
- Neurodynamics and Flexibility
- Heel raise on Leg press:
- Adjust the leg press machine as mentioned in the previous response.
- Instead of placing your feet flat on the footplate, position them with your toes pointing upward (dorsiflexed) and your heels hanging off the edge.
- Push the footplate away from you while keeping your heels elevated.
- Lower the weight slowly, allowing your heels to drop below the footplate to maximize the range of motion.
- Push the weight back up through your toes and the balls of your feet, focusing on your ankle muscles.
- Perform the desired number of repetitions.
2. Calf raises:
Find a surface, such as a step, where you can bring your heels down below your toes. and keep something close by that you can grasp with your hands to maintain balance.
Standing on the step with your feet shoulder-width apart, make sure your heels are hanging over the edge and the balls of your feet are flat on the floor.
Hold onto anything, such as a chair, if necessary for balance as you gradually lower your heels until they are at the same level as your toes.
Hold this posture for two to three seconds before slowly raising your body back up such that your feet are once more in line with your toes.
Ten repetitions of this exercise will constitute one set.
Perform three sets, taking a break in between each.
3. Theraband exercises:
Ankle Plantarflexion:
Cross your legs in front of you as you sit down.
Wrap the band’s one end around the ball of the foot you will be working out.
With one or both hands, hold the opposite end of the band.
Slowly press down with your foot as if you were pressing the gas pedal in a motor vehicle.
Return to the starting position gradually.
Ankle Dorsiflexion:
Over a sturdy table leg or bedpost, loop one end of the band.
As you sit, extend your legs in front of you.
The other end should be wrapped around your foot’s top.
Feel the band pulling against your foot as you raise your toes towards your head.
Retract the foot gradually.
Ankle inversion:
As you sit, extend your legs in front of you.
Wrap the band’s one end around the ball of the foot you will be working out.
At the ankles, cross your other leg over top.
Position the band so you can grasp the other end with one or both hands beneath the ball of the top foot and up the leg.
While tugging against the band with your foot while holding the band.
Retract the foot gradually.
Ankle eversion:
As you sit, extend your legs in front of you.
Wrap the band’s one end around the ball of the foot you will be working out.
Position the band such that you may grip the other end with one or both hands by placing it under the ball of your other foot and up the leg.
While holding the band, extend your foot and pull against it.
Reintroduce the foot gradually.
4. Single leg stance:
If you need to balance yourself, stand behind a chair and rest your hands on the seat.
Lean on your damaged foot while raising one leg off the ground.
Maintain this posture. You should gradually extend the amount of time you can hold it. You can start with ten seconds and work your way up to sixty seconds by adding ten seconds each day after that.
To finish a set of three, carry out the identical exercise two more times.
5. Hamstring curls:
Place your feet hip-width apart as you stand. Place your hands on a chair or your waist for balance. Now your weight should be supported by your left leg.
The heel of Your right knee should be moving toward the butt as you slowly bend it. Maintain parallel thighs.
Lower your foot gradually.
Do 12 to 15 repetitions.
the other leg, and repeat.
6. Bridging (glutes):
With your knees bent, lie on your back. Your abdominal muscles should be tightened. Lift your hips off the ground once your knees and shoulders are in place. Three full breaths should be held. Repeat from your starting position.
7. Ankle instability stretching exercises:
Towel stretch:
Sit on the floor with straight legs.
Keep your back straight and wrap a large bath towel around both of your feet, holding the ends with both hands.
Make sure that your leg is straight as you slowly pull the towel in your direction.
Pull the towel until you can feel your foot’s arch stretching.
For 30 seconds, maintain this posture.
Go back to the beginning place.
Do this stretch two more times.
Standing calf stretch:
Stand in front of a wall with your arms straight out in front of you as your palms are pressed flat against the wall.
With your right knee slightly bent, extend your leg forward.
Make sure your left leg is straight behind you and that your heel is pulled all the way down to the floor.
Hold this for 30 seconds;
Go back to the beginning place.
Do this stretch two more times.
8. Neurodynamics and flexibility exercises:
Ankle Dorsiflexion Neural Glides:
- Sit comfortably with your legs extended.
- Keep your knee of the affected ankle straight.
- Gently point your toes (plantarflex) and then flex them upward (dorsiflex) as much as you can comfortably.
- While maintaining the dorsiflexed position, gently dorsiflex your ankle even further by pulling your toes gently toward you.
- Hold this position for a few seconds, feeling a gentle stretch along the front of your ankle.
- Slowly return to the starting position and repeat for about 10-15 repetitions.
These neural glides can help improve neural mobility and flexibility in the ankle joint.
Phase 2
Cardio-vascular fitness:
- Running: Your lower body strength and cardiovascular fitness will both increase as a result of jogging. You must perform particular workouts that condition and strengthen the joint while applying a safe amount of load to weak ankles.
2. Elliptical: The elliptical machine can be a wonderful low-impact fitness option for a few weeks old, slight ankle injury. Work with your doctor and physical therapist to create a safe exercise regimen if you fractured your ankle last week or sprained it severely a few days ago.

3. Stepper:
Basic stepper exercise:
Stand with both feet on the stepper.
Slowly lift one foot off the stepper, balancing on the other foot.
Hold this position for a few seconds, then lower your foot back onto the stepper.
On each foot, perform 10 to 15 repetitions of this exercise.
As you progress, try increasing the duration you hold each position to challenge your ankle stability further.
Single-Leg Stepper Balance:
Stand on one foot on the stepper with your knee slightly bent.
Aim for 30 to 60 seconds to hold this position as long as you can.
Switch to the other foot and repeat.
4. Rowing machine:
Rowing is a low-impact exercise, which means it puts minimal stress on the ankles. This is crucial for individuals with ankle instability or those recovering from ankle injuries as it reduces the risk of exacerbating the problem.
Rowing promotes gentle ankle movement as you push and pull with your legs, which can help improve ankle mobility without putting undue stress on the joints.
It can assist in managing body weight, reducing the load on the ankles. Rowing requires balance and stability, which can contribute to strengthening the muscles around the ankle joint, potentially enhancing ankle stability over time.
Functional strength:

- Modified lunges
- If you have ankle instability and want to perform lunges safely and effectively, you can modify the traditional lunge exercises to reduce the risk of injury and improve stability.
- Stationary Lunges
- Elevated Heel Lunges
- Supported Lunges
- Squats: bilateral, single leg
- Squats are a fantastic lower body exercise that can be performed both bilaterally (using both legs) and unilaterally (using a single leg).
- Bilateral squats: Stand shoulder-width apart, squat down with both legs, keep knees aligned with feet, then stand back up. Great for leg strength.
- Single-leg squats, also known as pistol squats:
- Place the other leg out in front while standing on one leg. Lower your body into a squat while keeping the elevated leg straight. Maintain balance and form. Stand back up. Perform 2-3 sets of 5-8 reps on each leg.
- Single leg activity: Single-leg activities are exercises that involve standing, balancing, or moving on one leg at a time. These exercises are excellent for improving balance, stability, strength, and flexibility. They are especially beneficial for athletes, individuals recovering from injuries, or anyone looking to enhance their lower body strength and stability.
Balance training
- Aeroplane, Star Excursion Balance Test
- Bosu ball, Balance pad, Wobble board:
- Place one or both feet on a wobble board or balance disc.
- The uneven ground tests your balance and engages the muscles that stabilise your ankles.
- Circling or shifting your weight from side to side are two exercises to try.
Shoe assessment
Phase 3
Cardio-vascular
- Sport-specific exercises and techniques
- Endurance
- Terrain
Balance/ function/ agility
- Jumping, skipping, landing
- Jumping, skipping, and landing exercises are effective for improving ankle stability and proprioception. These exercises challenge your ankles to control movements while jumping and landing, which can help reduce the risk of ankle injuries and enhance overall stability.
- Multiple hops
- Multiple hops exercises are often used to improve ankle stability and strength. These exercises help to strengthen the muscles around the ankle joint and improve proprioception (awareness of your body’s position in space), which is crucial for preventing ankle injuries and improving stability.
- Basic Single-Leg Hops:
- Stand on foot with your knee little bent.
- Hop forward, landing on the same foot.
- Maintain balance and control.
- Perform 2-3 sets of 10-15 hops on each leg.
- Vertical jumps
- Vertical jumps, also known as vertical leap or vertical jump training, are exercises and drills aimed at improving your ability to jump vertically. This type of training is essential in various sports like basketball, volleyball, and track and field, where the ability to jump high can provide a competitive advantage.
Including activities particular to a specific sport without reducing movement quality.
Monitoring of pain
Aerobic Exercise for Chronic Ankle Instability Exercise:
An injured ankle can benefit from aerobic activity, which can also aid with ankle instability. However, you should always see a medical expert first to make sure the exact workout is suitable for your situation.
A podiatrist, physical therapist, or physician would typically recommend low-impact exercises for rehabilitation, such as swimming or using a stationary bike.
Surgical Management:
Depending on the degree of ligament weakening, surgery may be a possibility if non-surgical therapy for ankle instability is ineffective. The two most common procedures for ankle instability are:
Brostrum’s method:
It is possible to reattach the fractured ligaments to the bone by tightening them. This kind of operation, also known as the Brostrum’s treatment, is quite effective and suitable for persons who lead busy lifestyles.
Tenodesis surgery:
A tenodesis technique may be performed if all other possibilities have been exhausted and have proven unsuccessful or unsuitable. To recreate new ligaments, a strip of hamstring must be taken. Only in extreme cases of instability and when the ankle is expected to be put under a lot of strain should this method be considered. Although a highly long-lasting remedy for ankle instability, this kind of surgery typically results in ankle stiffness.
Tips to prevent ankle instability:
Always carry out the recommended rehabilitation activities for ankle sprains:
If you’ve ever injured your ankle and had it correctly treated, you likely received a variety of strengthening exercises, balance exercises, and stretches to perform to help your ankle heal. Many people believe that once their ankle feels better again, they no longer need to perform the exercises, but this couldn’t be further from the truth. To guarantee that the ankle has a full range of motion and won’t experience more issues in the future, such as ankle instability, you must complete the exercises prescribed by your doctor or physiotherapist.
Don’t ignore ankle discomfort:
In this situation, it is particularly true that you shouldn’t overlook ankle pain that has developed quickly as a result of an injury. You should never dismiss any ankle discomfort. If an acute ankle sprain is overlooked or improperly managed, the ligament may become even more torn. Treatment and rehabilitation become more difficult as a result. Additionally, it makes you more vulnerable to getting ankle instability. Therefore, it’s crucial to seek medical attention or a podiatrist right away if you suffer an ankle injury.
When playing sports, brace your ankles:
Ankle braces can be used as a prophylactic measure in addition to treating ankle injuries. There is a greater danger of ankle sprains in high-contact, stop-and-start sports like hockey, soccer, and basketball. Before engaging in sports, you can prevent this by securing your ankle with a strap so that it is supported and won’t twist awkwardly and risk getting hurt. A brace will also teach the body not to move the ankle in any way that could harm it. You can strap your ankle with tape or wear an ankle brace to support it.
Always warm up before working out.
You should prevent an ankle sprain and other ankle injuries in the first place if you want to prevent developing ankle instability. Make sure to warm up before exercising to help your muscles become more flexible by increasing their temperature. As a result, you can avoid sprains and tension on the ligaments, tendons, and joints. You should perform a light to moderate endurance exercise for 5 to 10 minutes to warm up. A jog, star jumps, or some walking lunges could be used for this.
When should You consult a doctor for an ankle injury?
Podiatrists are excellent in identifying and treating ankle instability because they focus on diseases that affect the feet and lower limbs. To validate our diagnosis, a doctor might perform a physical examination. They will figure out the best course of action for your situation if they determine that you have ankle instability. Typically, a functional rehabilitation program will combine physical therapy and racing to achieve this.
A podiatrist can assess the degree of your ankle instability. Further testing can be performed, and they can address any queries you may have if they believe surgery may be necessary.
FAQs:
Chronic ankle instability is a condition characterized by recurring ankle sprains, persistent feelings of instability, and a weakened sense of balance in the ankle joint.
It often results from incomplete healing or inadequate rehabilitation after an initial ankle sprain. Repeated ankle injuries can also contribute to chronic instability.
Common symptoms include a sensation of the ankle “giving way,” recurrent ankle sprains, pain, swelling, and difficulty walking on uneven surfaces.
Diagnosis typically involves a physical examination, medical history review, and sometimes imaging tests like X-rays or MRI to assess the extent of damage.
Yes, many cases can be treated without surgery. Physical therapy, bracing, taping, and strengthening exercises can help improve stability and reduce symptoms.
Surgery may be considered when conservative treatments fail to provide relief, or in cases of severe ligament damage. Surgical options include ligament repair or reconstruction.
Preventive measures include proper rehabilitation after an initial sprain, wearing appropriate footwear, using ankle braces during physical activities, and participating in balance training
With proper treatment and rehabilitation, many individuals can manage chronic ankle instability effectively and reduce the frequency of ankle sprains.
While chronic ankle instability primarily affects the ankle joint, repeated ankle injuries can lead to issues like osteoarthritis in the long term.
Chronic ankle instability is relatively common, especially among individuals who have experienced one or more ankle sprains in the past.
In some cases, chronic ankle instability may improve on its own, but this is not guaranteed. It’s generally advisable to seek treatment to prevent further complications.
Untreated chronic ankle instability can lead to ongoing pain, increased risk of future ankle sprains, and long-term joint damage, including osteoarthritis.
Yes, physical therapists often recommend exercises to strengthen the ankle and improve balance. These exercises can include calf raises, proprioception drills, and resistance band exercises.
Yes, chronic ankle instability can limit athletic performance and increase the risk of sports-related injuries. Many athletes seek treatment to maintain their competitive edge.
Yes, functional instability refers to a perceived sense of instability, while mechanical instability involves objective signs of laxity or looseness in the ligaments.
Participation in sports or physical activities is possible with chronic ankle instability, but it’s essential to take precautions, such as using ankle support, and consulting a healthcare professional for guidance.
Yes, chronic ankle instability can impact daily activities and mobility, potentially causing discomfort or pain during routine tasks.
While maintaining a healthy diet can support overall healing and recovery, there are no specific dietary recommendations solely for managing chronic ankle instability.
Yes, it is possible for chronic ankle instability to affect both ankles, especially if an individual has a history of ankle injuries on both sides.
Reference:
Ankle and Foot Mobilisations. (n.d.). Physiopedia. https://www.physio-pedia.com/Ankle_and_Foot_Mobilisations
Best ankle instability exercises & stretches. (2023, July 5). The Feet People. https://www.thefeetpeople.com.au/learning-hub/best-ankle-instability-exercises-and-stretches/
Williams, M. (2023, February 2). Does Cycling Strengthen Ankles? 11 Key Facts & Bull; Bicycle 2 Work. Bicycle 2 Work. https://bicycle2work.com/does-cycling-strengthen-ankles/
Effective Hydrotherapy Exercises for Treating Lateral Ankle Sprains. (n.d.). SwimEx. https://www.swimex.com/resources/effective-hydrotherapy-exercises-ankle-sprains/
How to Tape an Ankle with Medical Tape or Kinesio Tape. (n.d.). How to Tape an Ankle With Medical Tape or Kinesio Tape. https://www.healthline.com/health/how-to-tape-an-ankle
WOBBLE BOARD: SINGLE-LEG BALANCE – Exercises routines. (n.d.). WOBBLE BOARD: SINGLE-LEG BALANCE – Exercises Routines. https://www.workoutsprograms.com/exercises/wobble-board-single-leg-balance
Management of Chronic Ankle Instability. (n.d.). Physiopedia. https://www.physio-pedia.com/Management_of_Chronic_Ankle_Instability
Chronic Ankle Instability. (n.d.). Physiopedia. https://www.physio-pedia.com/Chronic_Ankle_Instability
Chronic Ankle Instability Risk Identification. (n.d.). Physiopedia. https://www.physio-pedia.com/Chronic_Ankle_Instability_Risk_Identification
Squats-holistic physio fitness exercise. (n.d.). Holistic Physio Fitness. https://holisticphysiofitness.com.au/exerciselibrary/single-leg-stance-theraband-kickouts/Instructions:
Chronic Ankle Instability Treatment – London Foot and Ankle Centre. (2022, January 28). London Foot and Ankle Centre. https://www.londonfootandanklecentre.co.uk/condition/chronic-ankle-instability/
Sports Medicine Chronic Ankle Instability. (n.d.). https://www.nationwidechildrens.org/conditions/sports-medicine-chronic-ankle-instability

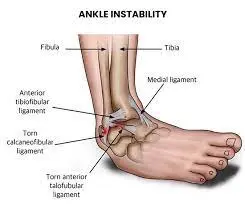
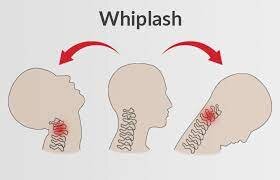

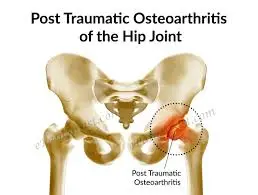
3 Comments