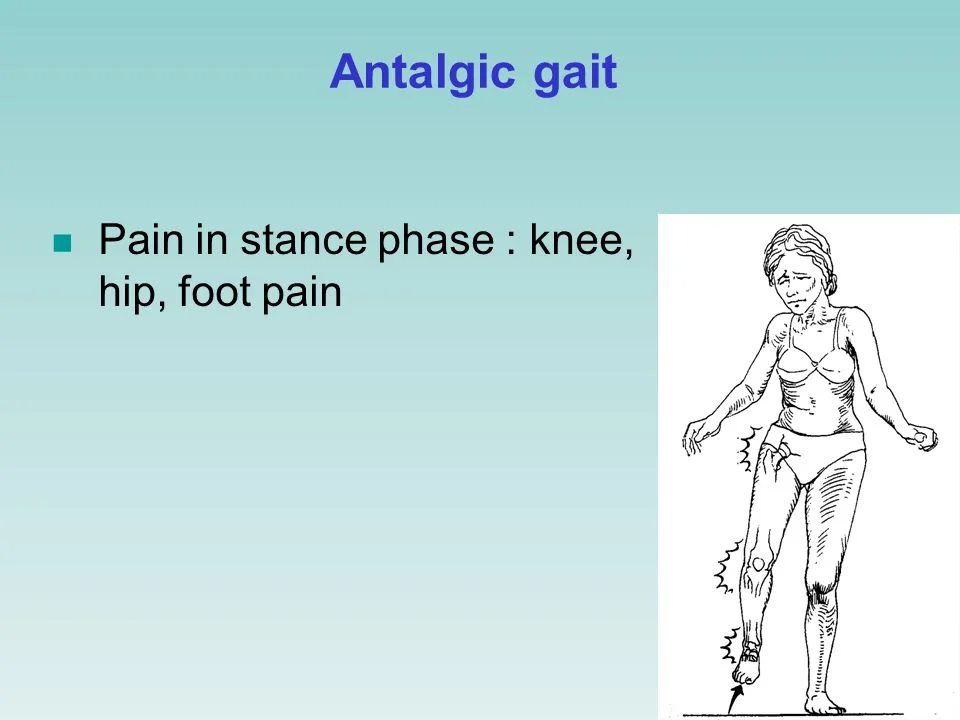
Antalgic Gait
Table of Contents
What is Antalgic gait?
Antalgic gait is a medical term used to describe a limp or altered walking pattern that is caused by pain in the leg or foot. When a person experiences pain in one of their lower limbs, they may try to avoid putting pressure on that limb when walking, which can result in an antalgic gait.
The typical antalgic gait involves a shortened stance phase on the affected side, which means that the foot spends less time on the ground during each step. This is because the person is trying to reduce the amount of weight-bearing on the affected limb, and therefore puts less pressure on it during each step.
Other features of an antalgic gait may include a decreased stride length, a wider base of support, and a slower walking speed. These changes in gait are often accompanied by visible signs of discomfort, such as grimacing or favoring the affected limb.
An antalgic gait can be caused by a variety of conditions, such as a sprained ankle, a stress fracture, or a herniated disc in the spine. Treatment for an antalgic gait will depend on the underlying cause and may include rest, physical therapy, or medication to manage pain and inflammation.
Most people have probably experienced an antalgic gait at some point in their lives as a result of a misstep, or a tumble. The limp is frequently temporary and probably goes unnoticed.
There are more serious disorders that can induce pain and result in an antalgic gait, such as injuries, neoplasms, and arthritis. The majority of the time, these problems can get better with treatment.
Causes of Antalgic Gait
The majority of the time, a lower back or lower extremities disorder is the cause of an antalgic gait. Traumatic, viral, inflammatory, vascular, or neoplastic events are some of its potential causes. This adaptive change in stride targets to reduce the necessity of muscle and joint groups that might be impacted by these processes and prevent applying excessive pressure to uncomfortable locations.
Older people: As the Age increases the probability of developing a gait issue is higher,l. which affects more than 60% of people over the age of 80. Patients frequently complain about it when they go to the emergency room or a primary care doctor’s office.
Pediatrics: Some age-related preferences for pediatric antalgic gait causes remain. While Legg-Calve-Perthes disease (LCP) and transient synovitis are the most frequent causes in younger children, slipped capital femoral epiphysis (SCFE) and osteoid osteoma are common in adolescents and teenagers.
The most frequent cause of struggling in kids is a minor injury, followed by inflammation and infection.
Injury: Usually not serious and will get well on its own. An underlying bone fracture may be indicated by persistent limping.
Infection: In young children, infections caused by bacteria or viruses in developing bones and joints can result in discomfort and limping.
Inflammation: Joint discomfort, swelling, and the recognizable antalgic limp can all be symptoms of juvenile arthritis.
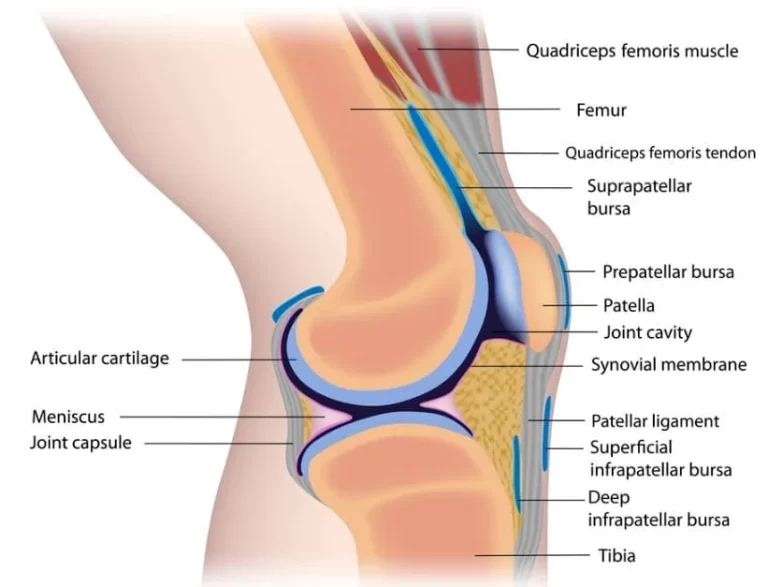
Osteoarthritis: This type of arthritis develops as a result of “wear and tear” on frequently aging joints. Obesity and previous traumas may also be factors. Older persons with two forms of arthritis may experience pain and an antalgic gait
Rheumatoid arthritis causes ligament injury, cartilage destruction, and bone erosion as a result of the development of ruptured tissue. It results in discomfort and could lead to deformed joints.
Antalgic gait can be a result of back problems such as.
The sciatic nerve, which is the longest in the body, runs from the posterior region of the pelvis to downward the buttocks, then down both legs and into the foot. It is causing pain when it is irritated or compressed by some tissue or any other reason.
Spinal osteomyelitis is an infection that develops when bacteria get stuck in a spinal disc between vertebrae and then enter the bloodstream. Older adults are more frequently affected.
Inflammation and irritation of the disc gaps between the tiny bones in the spine, which results in discomfort and limping.
Additionally, the following diseases can also lead to antalgic gait.
Tumors: These can expand into soft tissue and bone, resulting in pain and walking difficulty.
When the pelvic joint motion occurs in different ways, the pelvic girdle becomes less stable and can become painful in pregnant women.
Sign and Symptoms of Antalgic Gait
The primary sign of an antalgic gait is pain. There are some conditions where we can experience pain such as a wound, infection, inflammation, vascular problems, or a tumor.
The changed gait is a natural attempt to decrease the discomfort of the damaged muscles, bones, nerves, or joint deformities that are the source of the pain.
Although there are many different gait disorders, antalgic gait is unique among them. When you walk, there is a difference tween a small “stance phase” and a long “swing phase.”
Foot discomfort: People who experience foot pain only put weight on the forefoot, heel, or lateral border of their foot.
Knee discomfort: people who have knee pain have difficulty fully extending or flexing the knee.
Hip pain: People who are experiencing hip pain may not extend their hips fully.
The following are the common signs and symptoms of antalgic gait:
- Limping: A noticeable limp or hobbling gait is the most common sign of antalgic gait. The person may also favor one leg over the other while walking.
- Shortened stride: The person may take shorter steps with the affected leg to avoid putting too much weight on it.
- Toe walking: In some cases, the person may walk on their toes to avoid putting pressure on the heel or ball of the foot.
- Wincing or grimacing: The person may show signs of pain, such as wincing or grimacing while walking.
- Reduced weight-bearing: The person may avoid putting weight on the affected leg altogether, causing them to limp heavily or use crutches.
- Asymmetrical gait: The person’s gait may be asymmetrical, with one leg swinging differently than the other.
- Slow walking speed: The person may walk more slowly than usual due to pain or discomfort.
- Stiffness: The affected leg may feel stiff or rigid, making it difficult to move smoothly.
- Muscle weakness: The muscles in the affected leg may feel weak or fatigued due to compensatory movements.
If you experience any of these signs or symptoms, it is important to seek medical attention to determine the underlying cause and receive appropriate treatment.
Complications of Antalgic Gait
The possibility of undiagnosed pathologies, such as septic arthritis, osteosarcoma (x-ray picture), or severe vascular disease, which can endanger life or limb, is the most dangerous complication of an antalgic gait.
an antalgic gait is not always connected to a small injury. So that It is critical to completely assess these disorders and not to make any assumption
An entire history and physical examination, together with proper doubt for significant causes in kids with an antalgic gait, will help kids have better outcomes.
Antalgic gait can also lead to a variety of complications, including:
- Muscle imbalances: The altered gait pattern associated with antalgic gait can lead to muscle imbalances, which can further exacerbate pain and limit mobility.
- Joint stiffness and instability: Antalgic gait can cause joint stiffness and instability, particularly in the affected limb or joint.
- Reduced range of motion: The altered gait pattern can result in a reduced range of motion in the affected limb or joint, which can further limit mobility and increase pain.
- Chronic pain: Antalgic gait can lead to chronic pain, which can significantly impact a person’s quality of life and mental health.
- Secondary injuries: Antalgic gait can increase the risk of secondary injuries, particularly in the opposite limb or joint, as well as in other parts of the body due to compensatory movements.
How do you feel?
To get a sense of the antalgic stride, Imagine walking with a sharp stone in your shoe. An unsteady step arises from attempting to avoid the pain.
you will probably try to avoid doing so If it hurts when you walk and put pressure on your foot, knee, or hip. The result is frequently limping.
Antalgic gaits are frequently characterized by the ankle remaining stuck in place while the foot is raised and lowered.
Identification of Antalgic Gait
As there are several types of gait problems the diagnosis of antalgic gait at first relies upon the observation of identifiable, visual signs of the disease The doctor will probably observe your walk so they can notice the typical gait.
The symptoms of many disorders can be similar, so your physician will also search for aspects of your gait that cannot be incorporated in order to rule out related conditions. You might be asked to describe your discomfort.
The next step in the diagnosing process is to determine what is really causing your antalgic gait. There are many potential causes, which make this difficult. The doctor will often take any medical conditions and perform a physical examination before making a diagnosis.
Specifically in the legs or hips, they will be looking for soreness, edema, or bruising during the physical examination. Additionally, they will be on the lookout for back pain, stiffness, or curvature. Inadequate development or functional impairment will be on their radar.
To determine the proper reason for your antalgic gait, some tests could be required. Among these checks this trusted Source:
X-rays. These imaging studies are necessary to identify the structures causing your pain. An X-ray can not show every structure, but it can give you a solid idea of what is there. For comparison, the technician will likely take X-rays of both sides of your body.
Magnetic resonance imaging, or MRI. Your doctor might recommend an MRI scan to take a closer look. It will aid in the early detection of internal infections, tumors, bone fractures, and soft tissue injuries.
CT scan for computed tomography. In rare circumstances, this may be required to further deviation in skeletal.
Ultrasound. High-frequency sound waves are used in an ultrasound test to produce images within your body. Antalgic gait is frequently used to find out joint fluid that can be the reason for pain.
tests in the lab. To assist in the diagnosis of bacterial or viral illnesses, lab tests using blood or urine samples may be performed. Lab testing is also used to diagnose juvenile rheumatoid arthritis in children.
Difference between Antalgic Lean and Gait
Age, attitude, and personality can all have an impact on your gait, which is called your walking pattern. A typical gait consists of two phases: the stance phase, during which your feet are on the ground, and the swing phase, during which your foot is in the air. By the age of 3, you begin to learn this regular cycle and rhythm, and by the time you are 8 to 10 years old, you have fully developed it.
Some people walk differently for a variety of reasons. One is a limp brought on lower-limb pain, which is known as an antalgic gait. If walking causes pain in your knee, ankle, or foot, you will adjust it by cutting down on the length of your stance phase. As a result, you would not support your entire weight and will walk with a limp.
Antalgic lean frequently coexists with an antalgic gait. When you change the way you sit and lean towards one side for relieving back or leg pain, the antalgic lean takes place. Thus, the painful area is relieved of pressure.
Physiotherapy treatment for Antalgic Gait
Physiotherapy treatment for antalgic gait aims to reduce pain, improve mobility, and restore normal gait patterns. The following are some common physiotherapy interventions for antalgic gait:
Pain management:
The first step in treating antalgic gait is to manage pain. Pain management can be achieved through various modalities such as heat or ice therapy, electrical stimulation, ultrasound, or manual therapy techniques. These modalities can help reduce pain and inflammation in the affected area. The physiotherapist may also prescribe pain-relieving medications or refer the individual to a pain management specialist for further treatment.
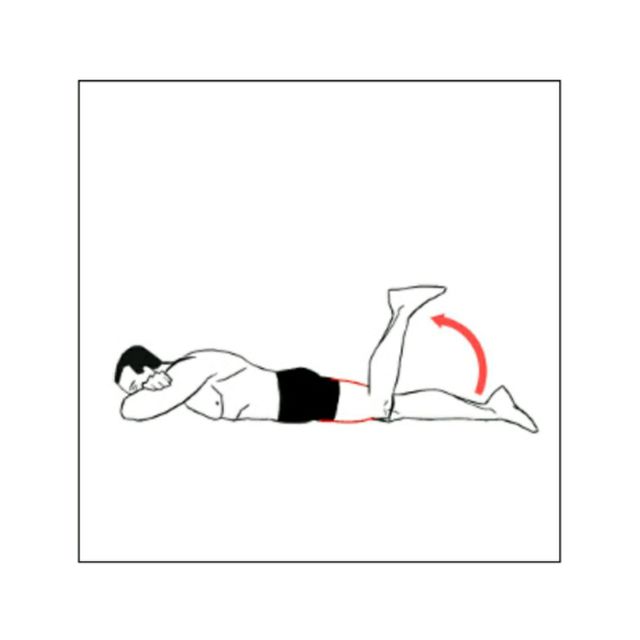
Strengthening exercises
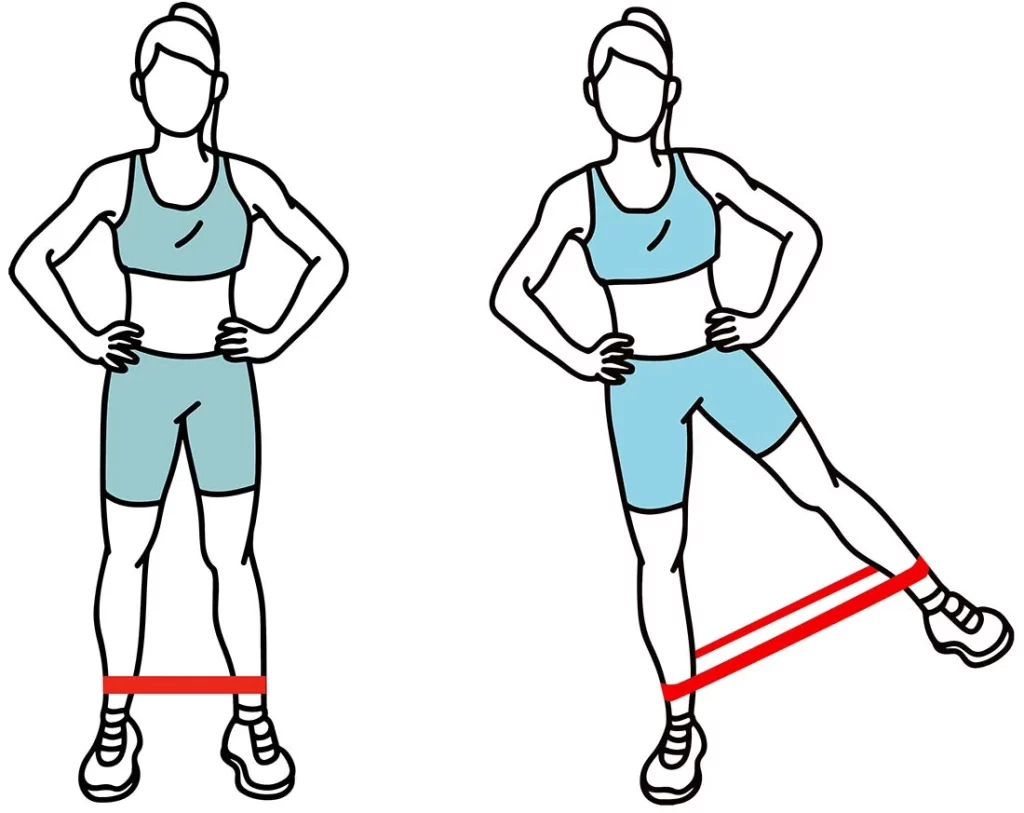
Weakness in the muscles of the lower extremities can contribute to antalgic gait. Therefore, strengthening exercises that particularly target the affected muscles can help improve gait mechanics and reduce pain. Strengthening exercises may include exercises for the glutes, quadriceps, hamstrings, and calf muscles. The physiotherapist will design a specific exercise program for the individual based on their strength and fitness level. Weak muscles can also contribute to antalgic gait, so strengthening exercises can help to build up these muscles and improve stability. A physiotherapist may recommend exercises such as squats, lunges, or calf raises
Range of motion exercises
Tightness or stiffness in the joints of the lower extremities can also contribute to antalgic gait. Mobility exercise can help improve flexibility and reduce pain. These exercises may include stretching for the hip, knee, and ankle joints. The physiotherapist will guide the individual through these exercises and ensure that they are performed correctly.
Gait training

Gait training involves practicing walking patterns to improve gait mechanics and reduce pain. This may include using assistive devices such as crutches or walkers. Gait training can help individuals learn how to walk with proper alignment and reduce stress on the affected area. The physiotherapist will monitor the individual’s progress and adjust the treatment plan accordingly.
Education and self-management
Education on proper body mechanics, posture, and self-management strategies can help prevent future episodes of antalgic gait and help improve overall function. Physiotherapists can provide education on proper ergonomics, lifting techniques, and exercises to maintain strength and flexibility. The physiotherapist may also recommend lifestyle modifications such as weight loss or changes in footwear to reduce the risk of future episodes of antalgic gait.
Modalities:

Modalities such as heat, ice, or electrical stimulation may be used to reduce pain and inflammation in the affected area.
Manual therapy:
Manual therapy involves hands-on techniques such as massage, joint mobilization, or manipulation to relieve pain and improve mobility. A physiotherapist may use manual therapy in combination with other treatments.
Stretching exercises
Tight muscles can contribute to antalgic gait, so stretching exercises can help to loosen up these muscles and improve flexibility. A physiotherapist may recommend specific stretches for the affected leg or foot.
It is essential to note that the treatment plan for antalgic gait may vary depending on the underlying cause of the condition. For instance, if the antalgic gait is caused by arthritis, the physiotherapist may focus more on pain management and range of motion exercises. On the other hand, if the antalgic gait is caused by a herniated disc, the physiotherapist may focus more on strengthening exercises and gait training.
Summary
In conclusion, antalgic gait is a type of abnormal gait that results from pain in the lower extremities. Physiotherapy treatment for antalgic gait aims to reduce pain, improve mobility, and restore normal gait patterns.
The treatment plan is individualized based on the underlying cause and severity of symptoms. With proper treatment, individuals with antalgic gait can improve their mobility, reduce pain, and restore normal gait patterns. It is crucial to seek medical attention if you experience an antalgic gait to identify the underlying cause and receive appropriate treatment.
FAQ
The majority of older individuals with antalgic gait get better with the right underlying cause treatment. Minor wounds will naturally cure themselves with the right treatment and rest.
A limp that results from pain, frequently in the foot, knee, or hip, is known as an antalgic gait. The most typical kind of limp that people can have is this one. Antalgic gait can be brought on by anything from tiny wounds that heal on their own to excruciating infections and tumors in the bone or soft tissue that require medical attention.
Antibiotics for infections can be used as another antalgic gait treatment, depending on the etiology.
Loss of weight.
physical treatment.
For injuries, apply rest, ice, and elevation.
drugs that reduce pain.
Anti-inflammatories.
Broken bone splints or casts.
canes, crutches, or walkers.
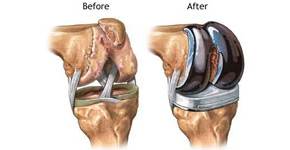
Treatment for antalgic gait depends on the underlying cause. It may include rest, physical therapy, medication, or surgery in severe cases.
Antalgic gait can be prevented by maintaining good posture, wearing supportive footwear, and avoiding activities that put excessive stress on the legs or feet.



One Comment