Steppage Gait
Table of Contents
What is Steppage Gait?
Steppage gait is a type of abnormal gait or walking pattern that is characterized by an exaggerated lifting of the foot and toes during the swing phase of walking. It is also known as drop foot gait or foot drop gait.
During normal walking, the foot is lifted and the toes are pointed upward in order to clear the ground during the swing phase. However, in individuals with steppage gait, there is weakness or paralysis of the muscles responsible for lifting the foot and toes, resulting in a high-stepping gait where the foot is lifted higher than necessary to clear the ground.
In the Steppage gait, there is the difficulty of raising the foot while walking as a result of the muscles that control the ankle joint’s dorsiflexion being weak. like foot drop but, Foot drop is not a condition that occurs frequently. the typical presentation in patients with a rapid onset of weakening of the muscles that stretch the foot when walking is the typical presentation.
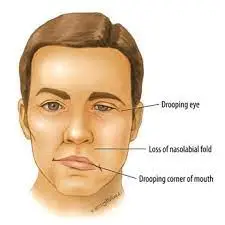
The history typically includes abnormal behavior, surgery, extended bed rest, a fracture-causing event, or a lower extremity in a very tight cast. The other reasons involve a history of vascular disorders of the collagen that cause ischemia in the nerves. An additional symptom of upper motor neuron injuries is foot drop. Unilateral or bilateral foot drops can be caused by peripheral neuropathies, for which diabetes is the most common reason. Hemiplegia and aphasia are also included for the same reason.
What is the Cause of Steppage Gait?
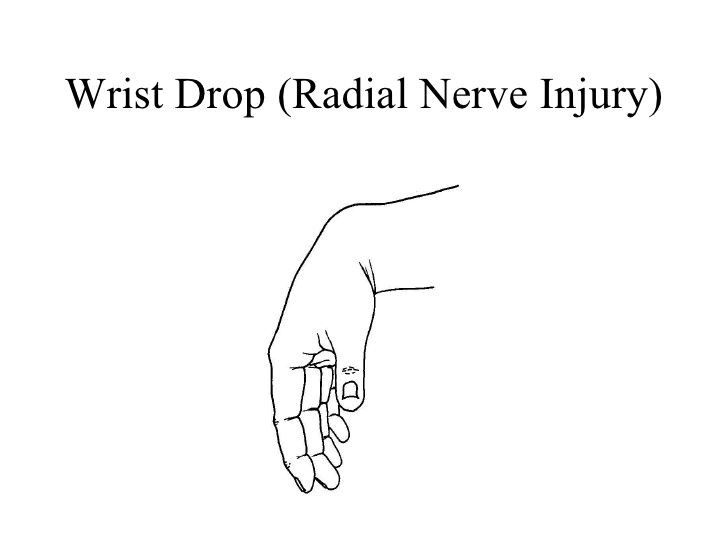
This type of gait is commonly seen in individuals with nerve damage or muscle weakness in the lower limbs, such as those with peripheral neuropathy, spinal cord injuries, muscular dystrophy, or multiple sclerosis. It can also be caused by certain neurological conditions that affect the nerves controlling the muscles of the foot and ankle.
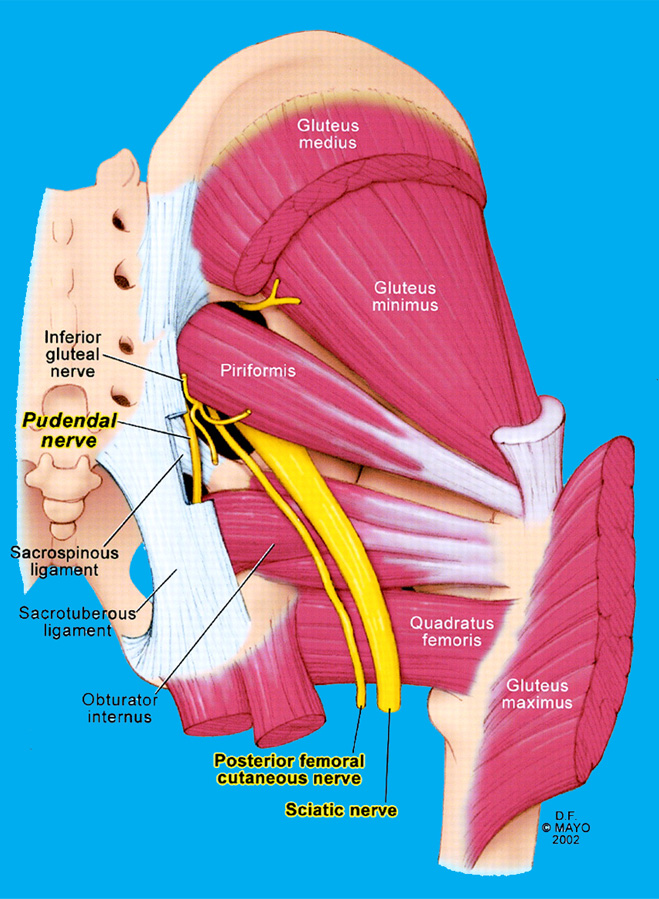
Traumatic injuries, pelvic fractures, tibia or fibular head fractures, fibular head fractures, tight casts, prolonged lithotomy positioning during surgical procedures, compression by a space-occupying lesion, vascular impairments as in diseases like lupus, or Waldenstrom macroglobulinemia which can result in vasculitis causing nerve ischemia, are some of the common causes.
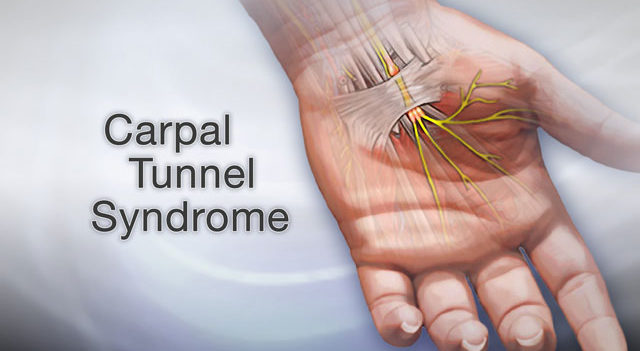
Peripheral neuropathies are neuropathies that affect the peripheral nervous system’s nerves. They may be mostly demyelinating, mostly axonal, or a combination of both. Congenital or acquired primary demyelinating neuropathies are also possible.
With exposure to toxins, viral or bacterial infections, and chemotherapeutic drugs like vincristine or vinblastin, primarily axonal neuropathies are observed.
Mixed peripheral polyneuropathies may result from conditions like diabetes, alcoholism, and renal failure.
Cerebral vascular accident (CVA) and amyotrophic lateral sclerosis are the main causes of foot drop. CVA manifests as hemiplegia or hemiparesis that is accompanied by aphasia, dysarthria, and dysphagia.
The upper motor neuron type is characterized by foot drop and high steppage stride, or “cock-walk gait”.
Statistics
Males are more likely to have peroneal neuropathy than females (2.8 to 1). 90% of peroneal lesions are unilateral and have no predilection for one side over the other.
After total knee arthroplasty (TKA), the frequency of occurrence ranges from 0.3 to 4%.
After proximal tibial osteotomy, foot drop may occur in 3 to 13% of cases.
Foot drop
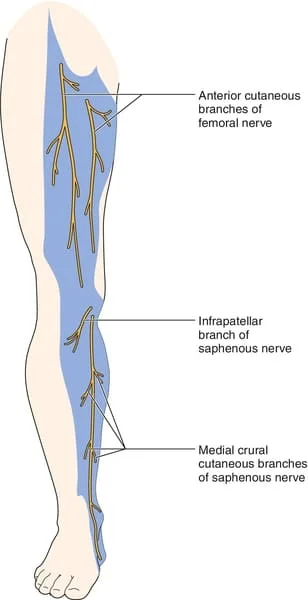
The anterior tibialis muscle, which is located in front of your shin bone, weakens or becomes paralyzed, which results in foot drop.
To assist in flexing your foot and ankle while walking the anterior tibialis muscle contracts. This makes sure that your foot clears the floor and that you would not step on your toes.
A high steppage gait may be present if the anterior tibialis is weak. This shows that as you stride forward, your hip and knee are bent excessively. To prevent stumbling and clear your foot over the ground, you lift your leg sharply off the floor.
Foot drops can be caused by illnesses that have an impact on the body’s muscles and nerves. They consist of the following:
Neuralgia of the periphery. The most frequent reason for peripheral neuropathy is diabetes. One often occurring hereditary peripheral neuropathy is Charcot-Marie-Tooth disease.
Muscle weakness and tissue loss are symptoms of muscular dystrophy.
A virus is which causes polio, which can result in paralysis and weakened muscles.
Examination
In order to rule out fracture or dislocation in the event of trauma, the diagnostic examination should include plain X-rays of the pelvis and tibia or fibula. MRI results for suspected plexopathies may be suggestive.
In cases of collagen vascular, Rheumatoid factor, which is an antinuclear antibody (ANA), and other pertinent laboratories should be examined Consideration should be given to complete blood count, differential count, and SMA 18 to rule out sepsis.
Studies on nerve conduction velocity (NCV) and electromyography (EMG) will reveal denervation potentials and motor units. Tibialis posterior weakness is caused by L5 radiculopathy, lumbar plexopathy, and a lumbosacral trunk lesion however it is not present in peroneal neuropathy. The weakening of the short head of the biceps in the former helps to distinguish the lateral trunk of the sciatic nerve participation from peroneal neuropathy. EMG can be used to examine these two muscles.
Treatment of Steppage Gait
Treatment for steppage gait usually involves addressing the underlying cause of the condition and may include physical therapy, bracing, or surgery.
Physical therapy referrals for pain management, strengthening exercises for the weak muscles, and range of motion (ROM) exercises for the ankle to prevent stiffness are advantageous in mild cases.
An ankle-foot orthosis (AFO) is recommended if the EMG reveals total loss of continuity and signs of neurotmesis or axonotmesis. The brace’s principal function is to keep the foot in the neutral position during the toe-off stage of the gait cycle. Since pressure sores can form where the brace touches the anesthetic foot, you can use routine skin inspections. You must wear footwear that has enough space and enough to support the brace.
Physiotherapy treatment for Steppage gait
Physical treatment with focused attention on the anterior tibialis muscle is used to treat a high steppage. anterior tibialis can be strengthened with certain ankle workouts. Calf stretches can keep your ankle’s range of motion intact.
Ankle exercises
Non-weight-bearing movement
Dorsiflexion
Ankle dorsiflexion, or the action of bending your ankle up towards your shin, is a straightforward exercise for strengthening your ankles. You can regain your ability to walk correctly with the help of this action.
- Firstly adjust your knee.
- Point your foot down towards your nose while simply moving your ankle. Continue doing this until you experience pain or reach your
- Maintain this posture for 15 seconds.
- Now back to normal position.
Plantar flexion
When you plantar flex, you move your ankle outward and downward. Your range of motion (ROM) may be improved.
- First Adjust your knee.
- Point your foot forward by merely moving your ankle. Continue doing this until you either experience discomfort or reach your limit.
- Maintain this posture for 15 seconds.
- Normalize your stand once again
Inversion
Inversion is performed When you point your ankle inside towards your midsection of the body. Turn your foot inside by slowly moving your ankle and maintaining your toes pointed upward. Your opposite leg should be facing the bottom of your foot. Continue until you experience pain or lose the ability to turn your foot inward.
For 15 seconds, maintain this posture.
Go back to being normal position.

Eversion
it is the movement of the ankle. which includes the outside movement of the leg. You can increase your ankle’s range of motion by performing this workout.
Turn your foot away from your other leg by slowly turning your ankle while maintaining your toes pointed upward. Keep doing this exercise until you either experience pain or lose the ability to turn your foot outward.
For 15 seconds, maintain this posture.
Now come back to normal position.
Partial weight-bearing exercise
Seated calf raising
You can put additional weight on the damaged ankle by performing these partial weight-bearing exercises. They are also used to strengthen the ankles. A person should perform this ten times at one set of exercises. you should place the hurt foot on the floor and sit on a chair.
When you hold your toes planted on the ground, then try to raise your heel as high as you can.
Put your heel back on the ground.
Weight shifting in standing
You might need to restrict how much weight you bear on the injured leg at first. This can shield your ankle while it heals.
Following that, you can gradually add more weight to your wounded ankle. Weight shifts are the ideal workout for this because they strengthen the ankles.
Holding on to something solid will help you stand straight.
Put part of your weight on the foot that is hurt.
For 15 seconds, maintain the position.
After that, unwind and reposition your weight to your healthy foot.

Full weight-bearing exercise
One leg standing
More weight will be placed on the hurt foot thanks to these workouts for strengthening the ankle. Before you place your entire weight on your ankle, make sure it can withstand the pressure. Lift the normal foot off the ground and stand on the affected foot.
For 15 seconds, maintain the position.
Remain calm and shift your weight back to your healthy foot.
Ten consecutive times, carry out each.

Calf raising in standing
Try calf raises once you are able to bear your entire body weight.
Lift the healthy foot off the ground and stand on the affected foot.
Lift your heel off the ground while standing only on the afflicted foot’s ball as you stand up.
For 15 seconds, maintain the position.
Remain calm and shift your weight back to your healthy foot.
Sidestepping
Stepping from side to side is used in this workout for strengthening the ankles. To the side of your wounded foot, place a rolled towel or other short object on the ground.
With the damaged foot, step over the towel while standing on that foot.
After that, step your unharmed foot over the item and stand upright.
Remain on the foot that isn’t hurt as you step back over the towel.
Then, re-cross the hurt foot over the towel and stand upright with both feet.
As your healing develops, you can speed up this workout.
Gait training exercise
To Improve range of motion
After a lower extremity injury, you might need to put in some effort to regain and maintain your joints’ normal range of motion (ROM). Swelling can frequently restrict joint ROM following surgery.
Additionally, after a time of immobilization due to an accident or surgery, tight muscles or other structures may restrict the range of motion. Your gait training exercise program may include working to recover that motion.
exercising to strengthen the lower extremity ROM could contain:
ankle boots
Towel calf stretches
Improve knee ROM with heel slips
stretching the hamstrings
stretching the hips
Maintaining a full range of motion (ROM) when you retrain your joints to walk will help them move freely as you step and transfer weight to each leg.

Obstacle Gait Training
Emphasizing your legs’ movements while you walk is one approach to improving your gait. Stepping exercises over barriers or minor hurdles is one technique to achieve that repeatedly. This makes it necessary for you to walk with your knees bent behind you while your hips are flexed up high.
How to practice obstacle gait training is as follows:
15 inches apart, place five or six little obstacles in a row. Rolls of toilet paper, athletic hurdles, or compact book stacks are all examples of obstacles.
Step over each barrier with one foot while facing it.
Put the second foot adjacent to the first one.
Repeatedly use one foot to navigate the obstacles. After that, turn around and advance with your other foot first over any impediments.
Step all the way over the first obstacle in the row when it becomes simple to do so, then repeat for the other obstacles. When taking steps, make sure to pull your knee up high and your foot and ankle up towards your buttocks.
Repeat navigating the obstacles ten times.
Stepping on a target
You might want to incorporate target stepping into your gait training exercise program to enhance lower extremity coordination. Performing target stepping
Set up a semicircle of four or five targets on the ground. About one foot should separate the objectives. Paper plates or little pieces of paper can be used as targets.
Place yourself on one side of the floor’s goals.
Step slowly to tap a target with your foot.
After putting that foot back in its original place, tap another target with your foot while reaching out again.
Tap each target repeatedly with one foot, then the other. Attempt to land each tap gently and lightly.
This exercise encourages single-leg standing while also assisting in the improvement of your ability to place your foot precisely where you want it while walking.
Neuromuscular electrical stimulation
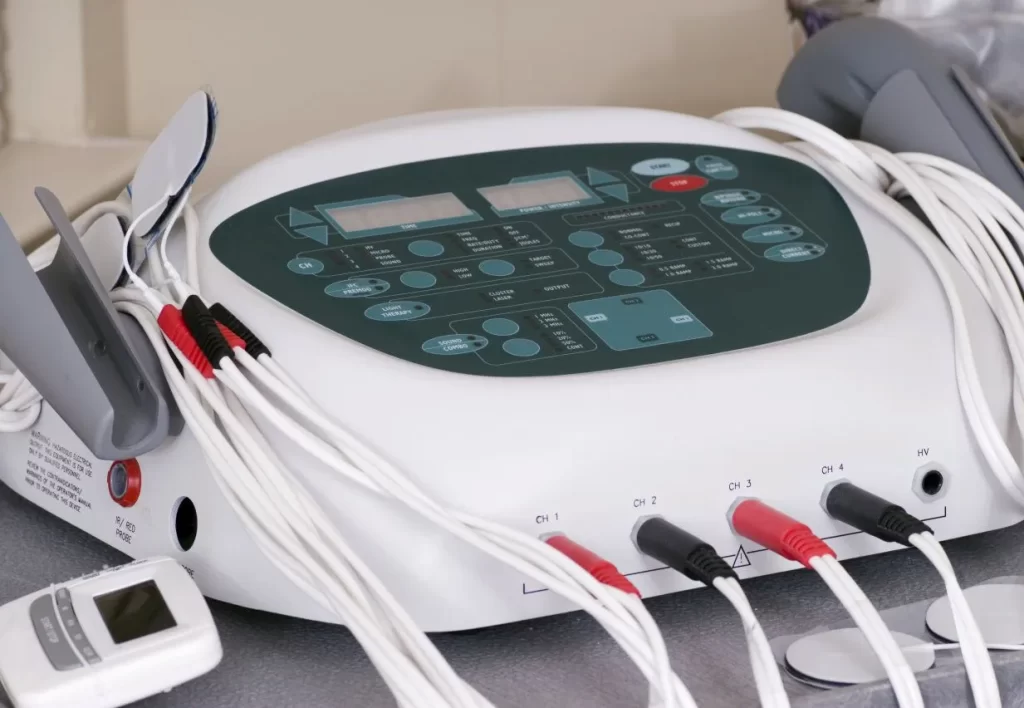
Neuromuscular electrical stimulation (NMES) is one type of electrical stimulation that is frequently used to treat foot drops. It is a form of electric stimulation that aids in artificially contracting your muscle to assist it learn to work properly once more.
Your Therapist will likely refer to a few fundamental procedures when using NMES. Here is the fundamental procedure.
In the front of your shin, let your anterior tibialis muscle show.
The front of your shin will be covered with tiny adhesive electrodes by your PT.
An electrical stimulation device will subsequently be linked to the electrodes.
The equipment will then be turned on by your PT, who will also increase the level of stimulation.
Most likely, the front of your shin will start to tingle.
The intensity should be increased until you can see your anterior tibialis muscle contracting. Unintentionally, your ankle will flex upward.
Work with the NMES unit as it flexes your ankle and make an effort to lift your toes and ankle even higher.
Use of assistive devices :

Your physical therapist could advise you to use an aid to help you walk correctly. This could be a quad cane, which has a base with four little feet, or a wheeled walker. Your physical therapist can make sure you’re utilizing your aid correctly.
Your anterior tibialis muscle might occasionally paralyze you permanently. If so, you can benefit from an ankle-foot orthosis (AFO), a type of specialized brace.
This brace assists in raising your foot and toes off the ground, lowering the possibility that you will stumble your toes. Wearing your AFO should make your high steppage stride disappear.
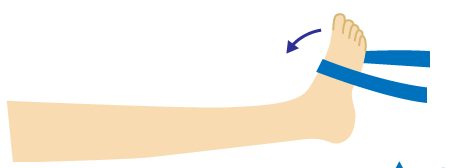
Use an elastic band to elevate your foot when walking as a temporary fix for anterior tibialis weakness.
Place the band around the ball of your foot and tie it around your leg slightly below the knee. The elastic band helps to keep your foot up as you swing your leg forward. To lift your toes off the ground, you are no longer required to take a high step.
Of course, it might not be practical to have an elastic band around your leg the entire day. However, utilizing it as a short-term fix can enable you to continue moving safely.
FAQ
Walking with a slapping gait occurs when the foot descends to the ground. He occasionally displayed a steppage gait, which is the result of attempting to raise the thigh to clear the toes while walking.
Steppage gait can be brought on by muscle atrophy or peroneal nerve damage (from spinal stenosis or a herniated disc, for example). Waddling gait: When you walk with a waddling gait, your upper body moves more dramatically than it normally would, giving you a waddling or duck-like appearance.
Steppage gait requires a higher-than-usual flexion of the knees to elevate the feet off the ground. Typically, muscle atrophy and weakness affect the muscles of the foot and leg, particularly the intrinsic foot and peroneal muscles.