The Vertebral Column
Table of Contents
Introduction
The vertebral column, also known as the spine or backbone, is a crucial structure that provides support and protection to the spinal cord while allowing for movement and flexibility.
The vertebral section consists of roughly 33 vertebrae that are separated by intervertebral circles. Each of the five distinct regions of the column is distinguished by a distinct vertebral structure.
Composed of individual vertebrae and intervertebral discs, the vertebral column plays a vital role in maintaining posture, balance, and overall body alignment. Dysfunction or injury to the vertebral column can lead to various conditions and disorders, including spinal cord injuries, herniated discs, and scoliosis.
The function, structure, and clinical significance of the vertebral column will be examined in this article.
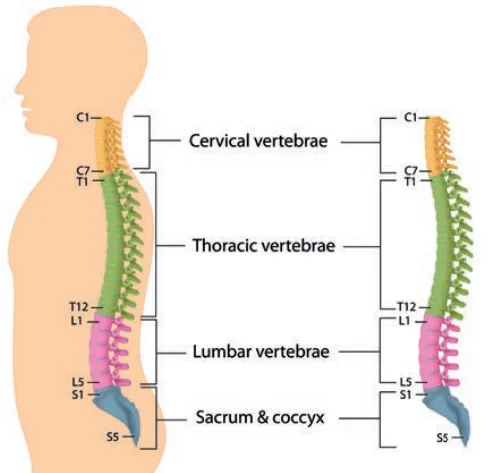
The vertebral section, otherwise called the spinal segment, is the focal pivot of the skeleton in all vertebrates. The vertebral column serves as a location for hemopoiesis, supports the trunk, shields the spinal cord and nerve roots, and provides muscle attachments. The mammalian vertebral segment comprises five morphologically separated gatherings of vertebrae: cervical, thoracic, lumbar, sacral, and coccygeal (caudal) The vertebral column in humans typically consists of 33 vertebrae that are arranged in series and are linked together by ligaments and intervertebral discs. Nevertheless, the number of vertebrae can range anywhere from 32 to 35. The sensory system is parted into 2 frameworks: The central nervous system (CNS) typically consists of seven cervical, twelve thoracics, five lumbar, five sacral, and four caudal (coccygeal) vertebrae. For males, the vertebral column is 71 cm long, while for females, it is 61 cm long.
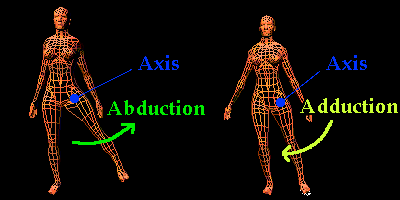
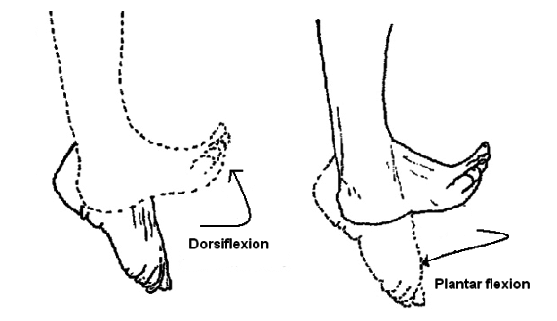
This part audits the hard parts of trunk life structures, including verbalizations and scope of movement (ROM).
Vertebral Column
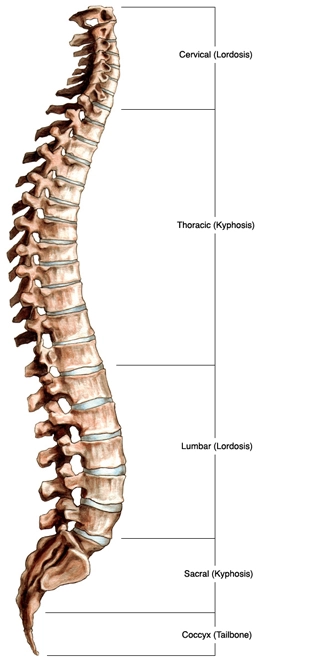
The vertebral segment is comprised of 26 vertebrae, which are named follows:•
- Cervical: 7
- Thoracic: 12
- Lumbar: 5
- Sacral: 5 (merged into the sacrum, a single bone)
- Coccygeal: 4 (the coccyx, which was fused into one or two bones)
Functions of Vertebral Column
The vertebral column has four main functions:
- Protection – encases and safeguards the spinal string inside the spinal waterway.
- Support – carries the body’s weight above the pelvis
- Axis – forms the body’s central axis.
- Movement – plays a role in both movement and posture.
Structure of Vertebral Column
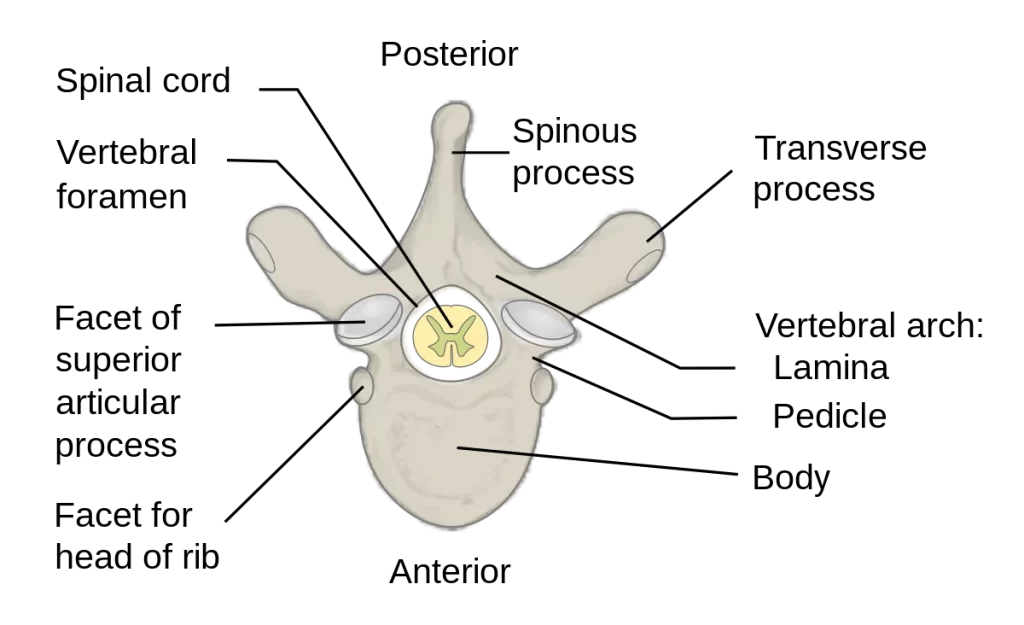
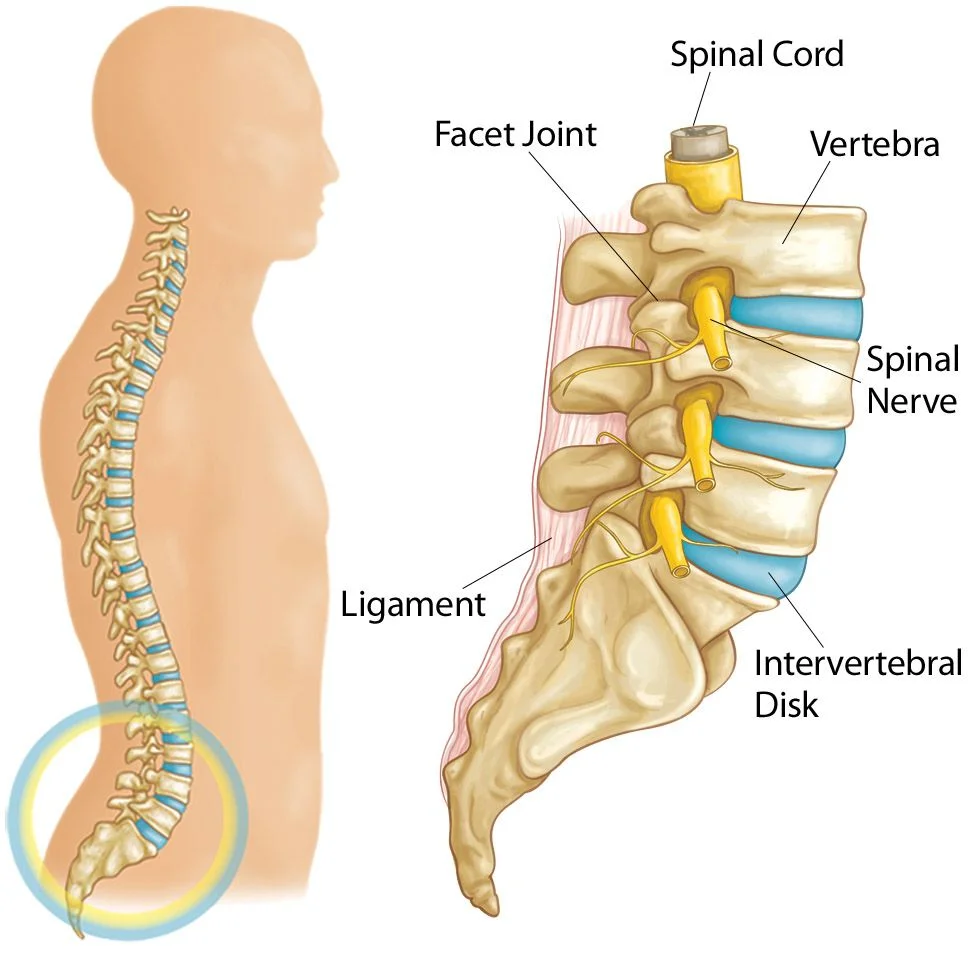
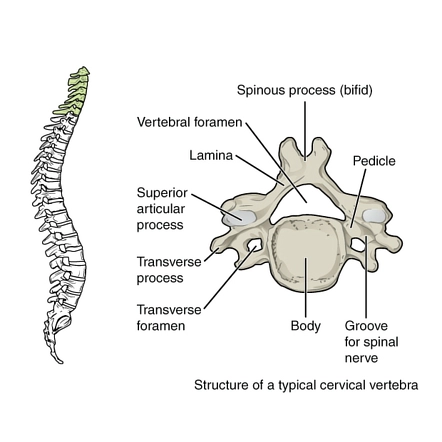
All vertebrae share a fundamental normal construction. An anterior vertebral body and a posterior vertebral arch make up each one.
Vertebral Body
Each vertebra’s anterior part is made up of the vertebral body.
It is the part of the column that bears weight, and the vertebrae in the lower part of the column are larger than those in the upper part (to better support the increased weight).
Hyaline cartilage covers both the upper and lower sides of the vertebral body. Neighboring vertebral bodies are isolated by a fibrocartilaginous intervertebral circle.
Vertebral Arch
Each vertebra’s lateral and posterior aspects are formed by the vertebral arch.
The vertebral foramen is an enclosed hole formed by the vertebral arch and the vertebral body. The vertebral canal, which protects the spinal cord, is made up of the foramina of each vertebra.
Numerous bony prominences serve as muscle and ligament attachment points in the vertebral arches:
- Spinous processes – A single spinous process is located posteriorly at the point of the arch in each vertebra.
- Transverse processes –From every vertebral body, two transverse processes expand laterally and posteriorly. The transverse processes articulate with the ribs in the thoracic vertebrae.
- Pedicles – connect the transverse processes to the body of the vertebra.
- Lamina – the transverse and spinous processes are connected.
- Articular processes – Joints are formed between vertebrae and their superior and inferior counterparts. The laminae and pedicles meet at the intersection of the articular processes.
Classifications of Vertebral Column
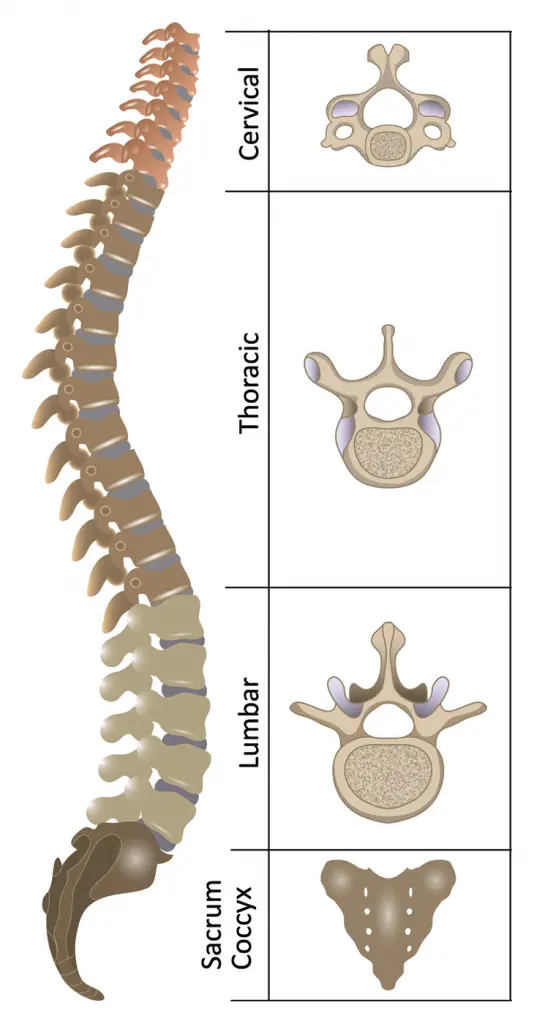
Cervical vertebrae
The human body has seven cervical vertebrae. They are distinguished by three main characteristics:
- Bifid spinous process – The distal end of the spinous process has a bifurcation.
- C1 (no spinous process) and C7 (spinous process that is longer than C2-C6 and may not bifurcate) are the two exceptions to this rule.
- Transverse foramina – an opening in each cross-over process that the vertebral veins use to get to the mind.
- Triangular vertebral foramen -Two distinctive cervical vertebrae C1 and C2, also known as the atlas and axis, are specialized to allow for head movement.
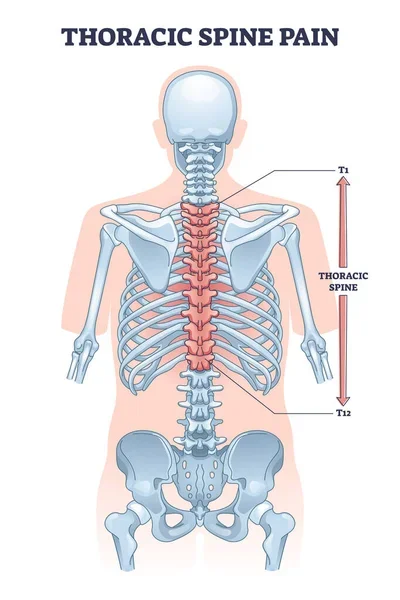
Thoracic Vertebrae
The twelve thoracic vertebrae are medium in size and move from superior to inferior in size. Their unique function is to articulate with the ribs, which results in the formation of the bony thorax.
Each thoracic vertebra has two “demi facets,” which are located on either side of its vertebral body and are placed superiorly and inferiorly. The heads of two distinct ribs connect the demi facets to one another.
A costal facet connects the shaft of a single rib to the transverse processes of the thoracic vertebrae. For instance, the head of Rib 2 explains the second-rate demi feature of thoracic vertebra 1 (T1) and the predominant demi aspect of T2, while the shaft of Rib 2 verbalizes the coastal features of T2.
The thoracic vertebrae’s spinous processes are oriented obliquely inferiorly and posteriorly. The thoracic vertebral foramen is circular, in contrast to the cervical foramen.
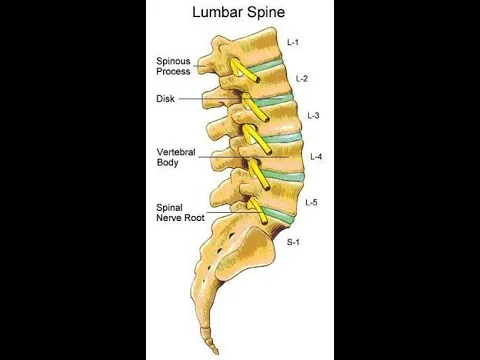
Lumbar Vertebrae
The majority of humans have five lumbar vertebrae, which are the largest in the vertebral column. They are designed structurally to support the torso’s weight.
Lumbar vertebrae have exceptionally huge vertebral bodies, which are kidney-molded. They lack transverse foramina, costal facets, and bifid spinous processes, which are characteristic of vertebrae.
However, like the cervical vertebrae, their vertebral foramen is triangular. The spinous cycles of these vertebrae are less extensive than those of thoracic vertebrae, but they still expand well below the level of the vertebral body.
Their size and direction make it conceivable to embed a needle into the spinal channel and the spinal rope something that would be inconceivable between thoracic vertebrae. Examples include lumbar puncture and epidural anesthesia administration.
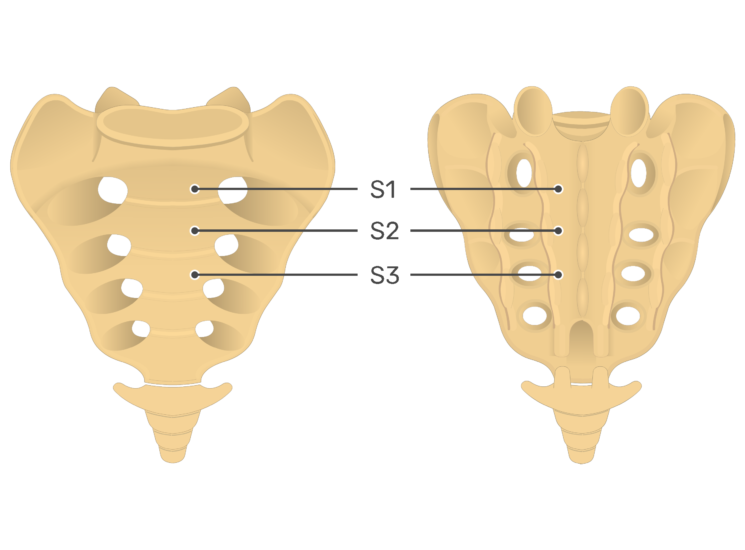
Sacrum and Coccyx Vertebrae
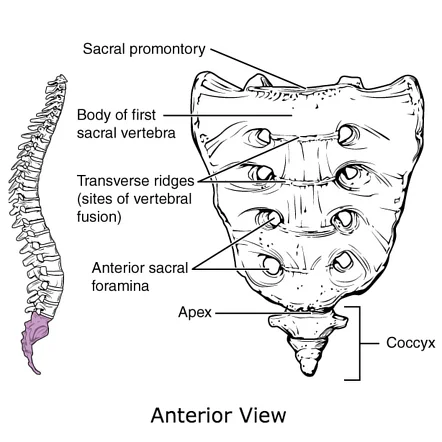
A collection of five fused vertebrae is the sacrum. It is referred to as an inverted triangle with an inferior apex. For articulation with the pelvis at the sacroiliac joints, the sacrum’s lateral walls are faceted.
The apex of the sacrum is articulated with the coccyx, a small bone. It is perceived by its absence of vertebral curves. Because of the absence of vertebral curves, there is no vertebral waterway.
The separation of S1 from the sacrum is termed “summarization”, while the fusion of L5 to the sacrum is termed “sacralization”. These conditions are congenital abnormalities.
Joints and Ligaments
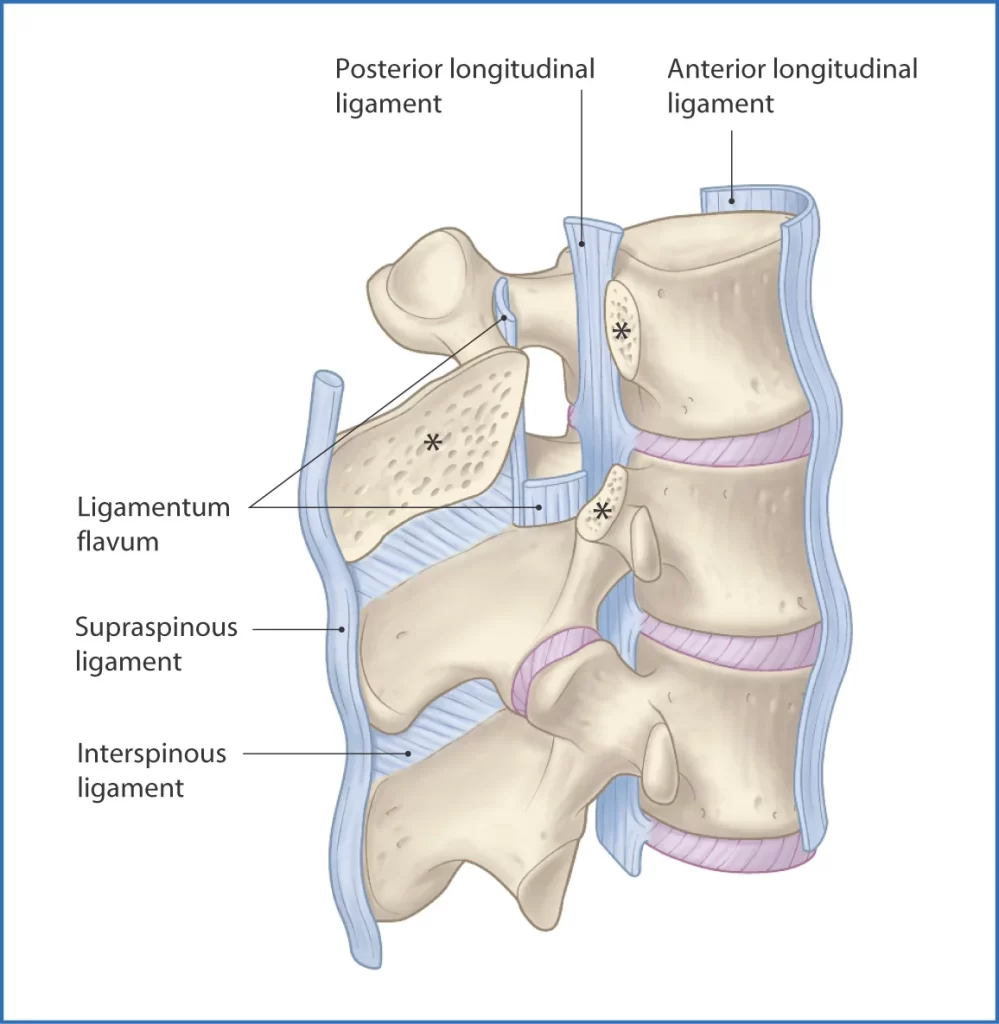
Through articular facets and joints between their bodies, the mobile vertebrae communicate with one another:
- The vertebrae above articulate with the left and right superior articular facets.
- The inferior articular facets on the left and right articulate with the vertebrae below.
- Vertebral bodies by implication articulate with one another through the intervertebral circles.
The vertebral body joints are cartilaginous joints, intended for weight-bearing. Hyaline cartilage covers the articular surfaces and connects them with the intervertebral disc.
The vertebral body joints are supported by two ligaments: the longitudinal ligaments that run the full length of the vertebral column, both anterior and posterior. The thick anterior longitudinal ligament prevents vertebral column hyperextension. Hyperflexion can’t happen because of the weaker posterior longitudinal ligament.
Glide motions between the vertebrae are made possible by the facet joints that connect the articular facets. Several ligaments give them strength:
- Ligamentum flavum –extends between adjacent vertebrae’s lamina.
- Interspinous and supraspinous – join the adjacent vertebrae’s spinous processes. The interspinous tendons append among processes, and the supraspinous tendons join to the tips.
- Intertransverse ligaments – extend between transverse processes.
Blood Supply and Lymphatics
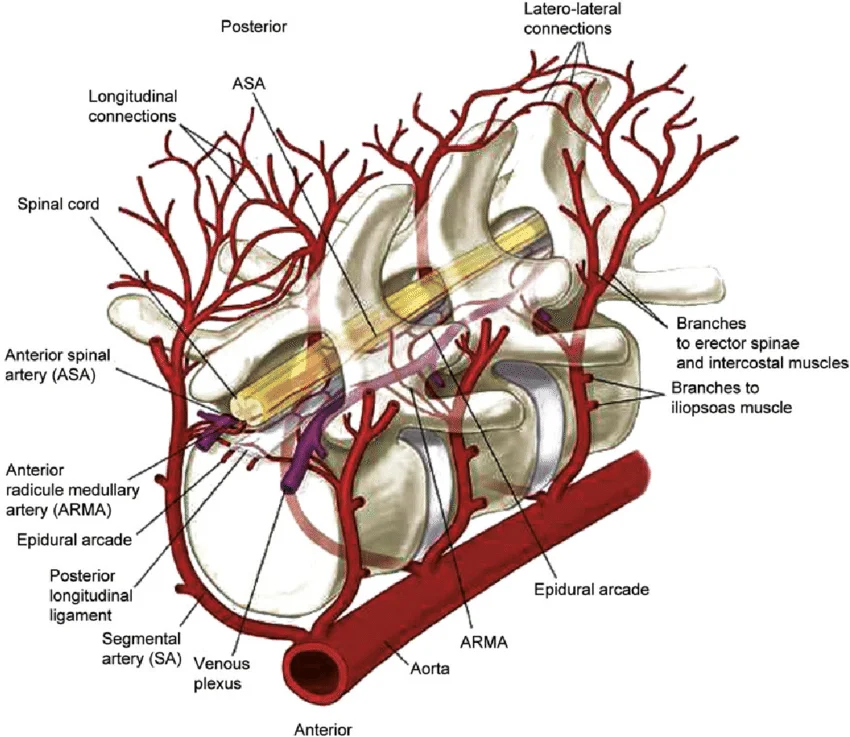
The branches of larger arteries that supply the internal organs give rise to the spinal arteries. The subclavian arteries of the neck split off into the vertebral and ascending cervical arteries of the spine. The lumbar arteries of the spine originate from the abdominal aorta, whereas the posterior intercostal arteries of the spine originate from the thoracic aorta. From the pelvic internal iliac arteries, the lateral sacral arteries branch. Every one of these corridors provides the spine parts into foremost and back branches. The front branch supplies blood to the vertebral body, and the back branch supplies blood to the vertebral curve. The middle of the vertebral column and the interior of the vertebral canal are supplied by radicular arteries.
The smaller veins of the spinal cord and the internal and external vertebral veins are drained by radicular veins. They discharge into intervertebral and segmental veins. Depending on where you are, blood flows into one of three large vessels. The cervical spine is drained by the superior vena cava. The inferior vena cava drains the lower regions of the lumbar and sacral spine, while the azygous and hemizygous veins drain the thoracic area.
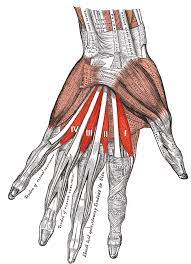
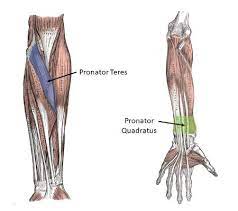
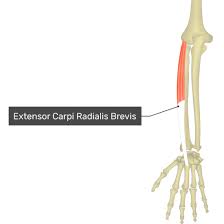
Muscles attachment
The spine, as the central bony structure supporting weight, experiences a lot of force. The muscles that append to the spine assist with keeping up with the pose and disperse the lopsided power of the body’s weight. They are separated into extraneous and natural back muscle gatherings.
The extrinsic muscles are further broken down into two groups: the superficial group, which includes the trapezius, latissimus dorsi, and levator scapulae, and the major and minor rhomboids, and the intermediate group, which includes the superior and inferior serratus posterior muscles. The scapula and humerus, as well as other upper-limb muscles, are moved by the superficial extrinsic muscles. To help with breathing, the intermediate extrinsic muscles move the ribs.
There are three layers that make up the intrinsic back muscles: deep, intermediate, and superficial These muscles help in the development of the spine and keep up with stances. The splenius capitis and splenius cervicis comprise the superficial layer. Neck flexion, rotation, and extension are all influenced by these. The paraspinal or erector spinae muscles, the iliocostalis, longissimus, and spinal muscles make up the majority of the intermediate layer. The central curvature of the spine is extended and maintained by the erector spinae, as their name suggests.
The muscles that are located between the transverse and spinous processes of the vertebrae are part of the deep layer of intrinsic back muscles. They are made up of three different muscle groups and are sometimes referred to as the paravertebral muscles. The most superficial is the semispinalis; It is noticeable in the cervical and thoracic regions. The multifidus is profound to semispinalis and most conspicuous in the lumbar locale. Lastly, the thoracic region is where the rotator cuff muscles are deepest and most prominent.
Deep in the back of the neck are the muscles of the suboccipital region. They are a part of the head’s movement and attach to the skull. These incorporate the muscles that make up the suboccipital triangle: the superior obliquus capitis, inferior obliquus capitis, and rectus capitis posterior major. The vertebral artery’s loop from the transverse foramen of the atlas enters the foramen magnum of the skull, where it supplies the brainstem, making this triangle significant.
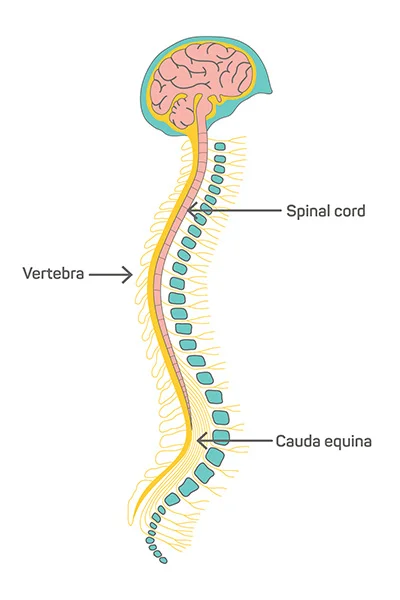
Nerves
The sensory system is parted into 2 frameworks: the brain and spinal cord make up the central nervous system (CNS), and the cranial nerves, spinal nerves, and ganglia make up the peripheral nervous system. The spinal line is held inside the vertebral segment. It ends at the conus medullaris and filum terminale at the base of the spine, where it runs from the base of the brain. The spinal cord’s tapering, cone-shaped end is the conus medullaris. In adults, it typically ends at L1-L2, but as an anatomical variant, it may extend further. The conus medullaris can be as low as L3-L4 in newborns. In order to lessen the likelihood of cord trauma during procedures like the lumbar puncture, the ending location is important. A delicate extension of the spinal cord from the conus medullaris that attaches to the coccyx’s dorsum is known as the filum terminale. The conus medullaris below extends into the cauda equina, or “horse’s tail.”
Thirty-one pairs of spinal nerves leave the spinal cord and enter the periphery via the intervertebral foramen. The vertebrae are innervated by meningeal spinal nerve branches.
Embryology
Shortly after conception, the human skeleton begins to develop. Around day 17, the notochordal process begins to form. After the roof of the yolk sac (of the underlying endoderm) fuses with the floor of the notochordal processes, the notochordal plate is formed. The notochord is made by folding the notochordal plate inward. The notochord is where the vertebral column develops and helps to maintain the embryo’s structure. The nucleus pulposus is created by adult notochord components. Likewise, the notochord invigorates the overlying ectoderm to shape a neuroectoderm, making the brain plate. The adult brain develops from the rostral portion of the neural plate, the spinal cord from the caudal end, and the neural tube from the neural plate.
At the point when the incipient organism starts gastrulation something like 3 weeks, the scleroderma of somites, explicitly the mesodermal part, develops around the brain cylinder and notochord to frame vertebral bodies and curves as well as the ribs. Segmentation is the process by which two adjacent sclerotomes (the caudal and cranial halves) fuse to form each vertebral body.
Endochondral ossification is the process by which the vertebrae grow. Around week 6, cartilage forms first, and bone replaces it from week 7 to week 8. Around the age of 26, complete endochondral ossification occurs. Degeneration and regeneration of the bones take place over time.
Clinical importance
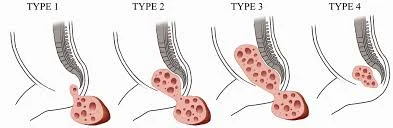
Intervertebral Disc Herniation
A fibrocartilaginous cylinder that connects the vertebrae is called the intervertebral disc. They absorb shock and allow the spine to be more flexible. They are wedge-shaped and support the spine’s curvature in the lumbar and thoracic regions.
The two parts of a vertebral disc are the annulus fibrosus and the pulpous nucleus. The solid and collagenous annulus fibrosus surrounds the jelly-like nucleus pulposus.
When the nucleus pulposus breaks through the annulus fibrosus, an intervertebral disc herniates. After the nucleus pulposis can irritate nearby spinal nerves, causing a variety of neurological and muscular symptoms, the rupture typically occurs posterior-laterally.
Abnormal Morphology of the Spine
The following clinical syndromes are brought on by an abnormal spine curvature:
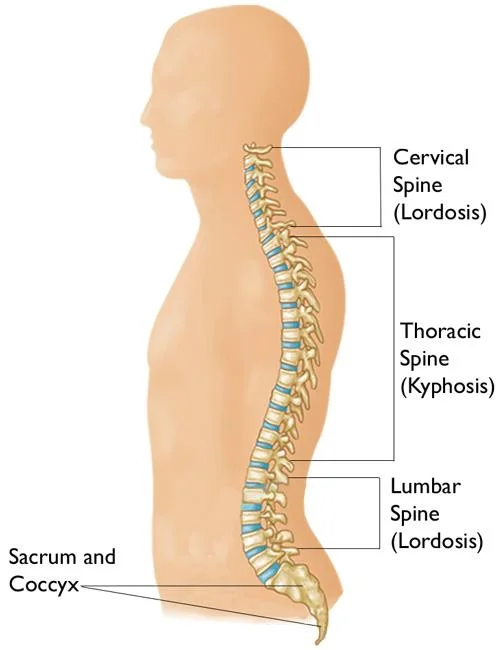
- Kyphosis – over the top thoracic curve, causing a hunchback distortion.
- Lordosis –swayback deformity as a result of excessive lumbar curvature.
- Scoliosis – horizontal bend of the spine, typically of obscure reason.
- Cervical spondylosis – a decrease in the size of the intervertebral foramina, usually due to degeneration of the joints of the spine. The more modest size of the intervertebral foramina comes down on the leaving nerves, causing torment.
The Cervical Spine
Between the cranium and the thoracic vertebrae is the superior portion of the vertebral column known as the cervical spine.
It has seven distinct vertebrae, two of which have their own distinctive names:
- Atlas refers to the first cervical vertebra (C1) in the neck.
- The second cervical vertebra, or C2, serves as the axis.
The characteristics, articulations, and clinical significance of the cervical vertebrae will be examined in this article.
Structure
The three primary characteristics of the cervical vertebrae set them apart from other vertebrae:
- Triangular vertebral foreman.
- Bifid spinous process – The spinous process divides into two distally at this point.
- Transverse foramina – holes in the transverse processes. The vertebral artery, vein, and sympathetic nerves are able to pass through them.
Atlas and Axis
Additional characteristics set the atlas and axis apart from the other cervical vertebrae.
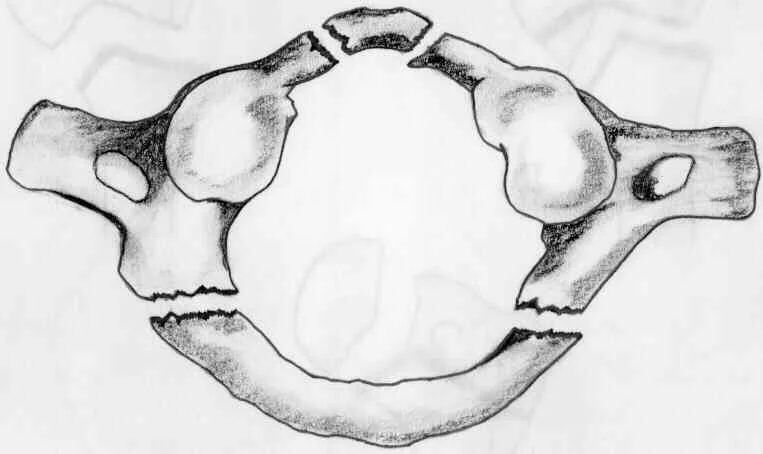
Atlas
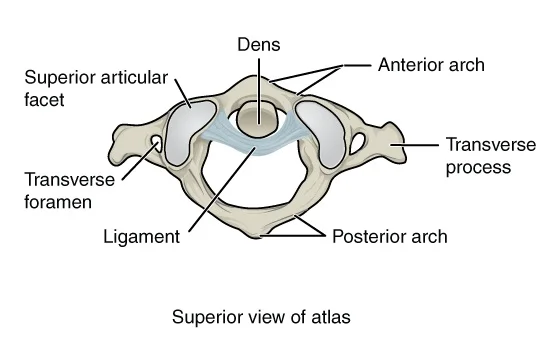
The map book is the main cervical vertebra and expresses the occiput of the head and the pivot (C2).
It differs from the other cervical vertebrae in that it lacks a spinous process and a vertebral body. The atlas, on the other hand, consists of lateral masses connected by an anterior and posterior arch. Every parallel mass has a predominant particular feature for explanation with occipital condyles and a sub-par articular feature for enunciation with C2.
The front curve contains a feature for explanation with the caves of the hub. This is gotten by the cross-over tendon of the map book – which joins to the parallel masses. A groove accommodates the vertebral artery and C1 spinal nerve in the posterior arch.
Axis
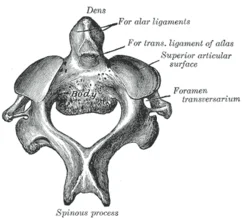
The dens (odontoid process) of the axis (C2), which extends superiorly from the anterior portion of the vertebra, make it simple to identify.
The medial atlantoaxial joint is formed when the dens articulate with the atlas’s anterior arch. Because of this, the head can rotate independently of the torso.
The two lateral atlantoaxial joints are formed by the superior articular facets of the axis and the inferior articular facets of the atlas articulating together.
Joints
There are two sorts of cervical spine joints: those that are found all through the vertebral section and those that are just tracked down in the cervical spine.
Present throughout Vertebral Column
The vertebral column is comprised of two distinct joints:
- Between vertebral bodies – nearby vertebral bodies are joined by intervertebral plates, made of fibrocartilage. A symphysis is a type of cartilaginous joint like this one.
- Between vertebral arches –formed by the articulation of adjacent vertebrae’s superior and inferior articular processes. It is a synovial sort joint.
Unique to the Cervical Spine
The atlantoaxial (x3) and atlantooccipital (x2) joints are unique to the cervical spine.
The articulation between the atlas and the axis creates the atlantoaxial joints:
- Lateral atlantoaxial joints (x2) – are framed by the verbalization between the mediocre aspects of the parallel masses of C1 and the unrivaled features of C2. These are plane-type synovial joints.
- Medial atlantoaxial joint – framed by articulating the nooks of C2 with the articular feature of C1.This is a pivot-type synovial joint.
The atlantooccipital joints comprise an enunciation between the spine and the head. They occur between the occipital condyles at the base of the cranium and the superior facets of the lateral masses of the atlas. These synovial joints, which are of the condyloid variety, permit head flexion, also known as nodding.
Ligaments
In the cervical spine, there are six significant ligaments to consider. Most of these tendons are available all through the whole vertebral segment.
Present throughout Vertebral Column
- Anterior and posterior longitudinal ligaments –long ligaments that cover the vertebral bodies and intervertebral discs and run the vertebral column length.
- Ligamentum flavum –interfaces the laminae of neighboring vertebrae.
- Interspinous ligament – connects the adjacent vertebrae’s spinous processes.
Unique to the Cervical Spine
- Nuchal ligament – a part of the supraspinous ligament that continues. It provides the rhomboids and trapezius with a proximal attachment and attaches to the tips of the spinous processes from C1 to C7.
- Transverse ligament of the atlas –anchors the dens in place by linking the atlas’s lateral masses together.
Anatomical Relationships
Numerous neurovascular structures in the neck are intertwined with the cervical spine in a close relationship.
The vertebral conduit, vein, and thoughtful nerves can pass through the cervical vertebrae’s cross-over foramina. This is only true in C7, where the vertebral artery circumvents the vertebrae rather than passing through the transverse foramen.
The cervical vertebrae and the spinal nerves are inextricably linked. Through the intervertebral foramen created by the joints at the articular processes, they reach above their respective vertebrae. Again, C7 is an exception because it has spinal nerves that extend from above the vertebra (C7) and below the vertebra (C8). Subsequently, there are eight spinal nerves related to seven cervical vertebrae.
Clinical importance
Jefferson Fracture of the Atlas
The lateral masses of the atlas between the occipital condyles and the axis can be compressed by a vertical fall onto an extended neck, such as when diving into water that is too shallow. This makes them be divided, breaking one or both front/back curves.
Assuming that the fall happens with sufficient power, the cross-over tendon of the map book may likewise be cracked.
The large vertebral foramen make it unlikely that the spinal cord will be damaged at the C1 level. However, further down the vertebral column, there may be damage.
Hyperextension (Whiplash) Injury
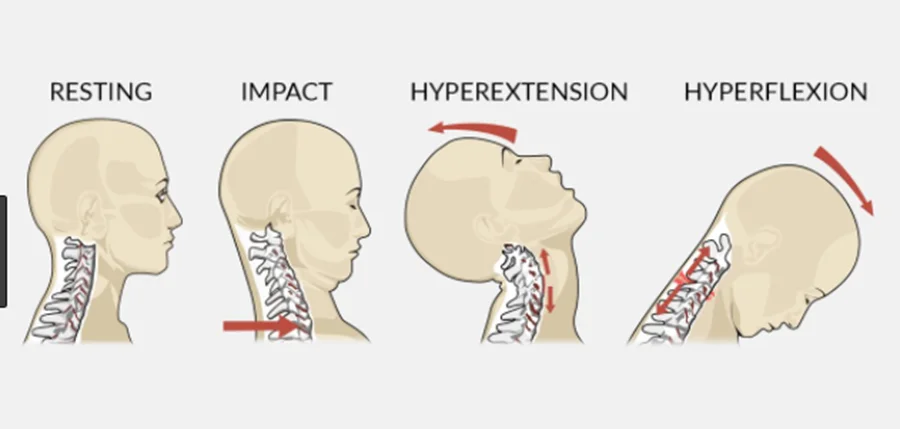
Whiplash can be brought on by a backside car accident or by a poor rugby tackle that causes the head to be whipped back on the shoulders. The anterior longitudinal ligament of the spine can be damaged in minor cases, resulting in acute pain for the patient.
In additional serious cases, cracks can happen to any of the cervical vertebrae as they are out of nowhere packed by quick deceleration. Again, the large vertebral foramen makes spinal cord involvement less likely.
The most dire outcome imaginable for these wounds is that disengagement or subluxation of the cervical vertebrae happens. This frequently occurs at the C2 level, where the collection of C2 moves anteriorly concerning C3. A spinal cord injury of this nature could result in quadriplegia or even death. At the C6/C7 level, subluxation occurs more frequently (50 percent of cases).
Fractures of the Dens
Breaks of the odontoid cycle address ~40% of C2 cracks.
Frequently these cracks are unsound and are at high gamble of connective corruption – because of the detachment of the distal section from any blood supply. There is a possibility of injury to the spinal cord, as with any fracture of the vertebral column.
The Thoracic Spine
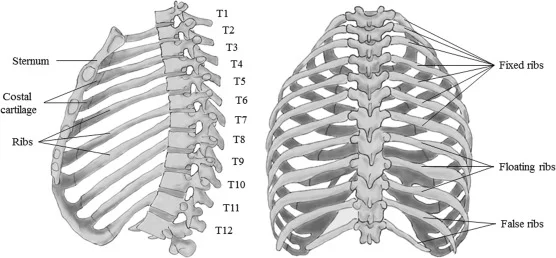
Between the cervical and lumbar vertebrae, the thoracic spine is the second segment of the vertebral column. There are twelve of them, and intervertebral discs separate them.
The thoracic spine is a part of the thoracic cage, along with the sternum and ribs. The internal viscera, such as the heart, lungs, and esophagus, are safeguarded by this bony structure.
The characteristics, joints, and clinical correlations of the thoracic vertebrae will be examined in this article’s osteology section.
Structure
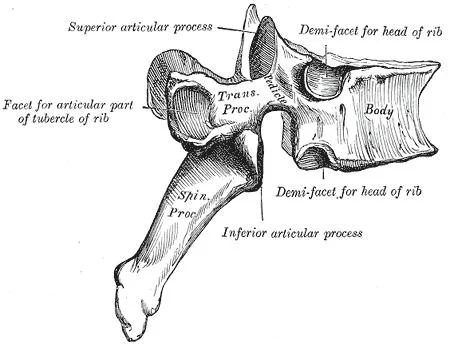
There are four characteristics that set the thoracic vertebrae apart from other vertebrae:
- The vertebral body is heart-shaped.
- Each vertebral body has demi-facets on the sides. – these move by means of the rib heads.
- Costal facets are present in the transverse processes. – these move in conjunction with the ribs’ tubercles. They only exist on T1-T10.
- The spinous processes are long and slant inferiorly. Preventing an object like a knife from entering the spinal canal, provides increased protection for the spinal cord.
Superior and Inferior Costal Facets
They are rib-head-articulating depressions lined with cartilage. The second rate feature explains with the top of the rib beneath, while the unrivaled aspect expresses with the top of the rib nearby it.
The majority of vertebrae (T2-T9) have these facets in the form of demi-facets. Some unusual vertebrae have complete facets.
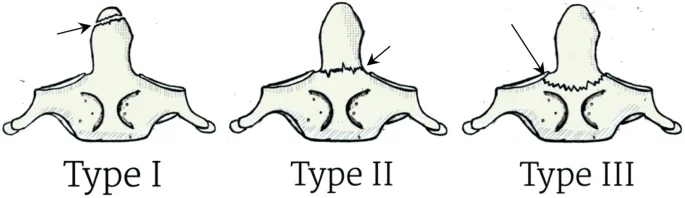
Atypical Vertebrae
The predominant and mediocre coastal aspects of the abnormal thoracic vertebrae fluctuate in size, area, and number.
- T1 –Because this is the only vertebra that can articulate with the first rib, it is not a demi facet.
- T10 – There is a single pair of complete facets that articulate with the 10th rib. Both the pedicle and the body of the vertebrae contain these facets.
- T11 and T12 – On the pedicles, each has a single pair of complete coastal facets.
Joints
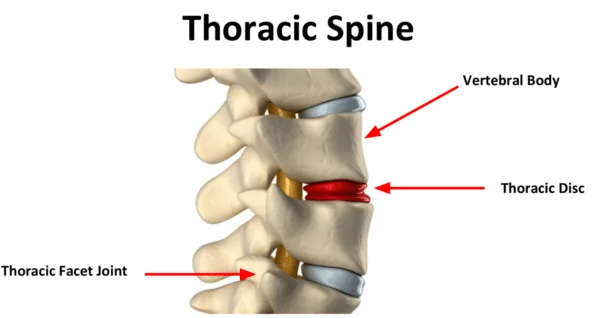
There are two kinds of joints in the thoracic spine: those that are exclusive to the thoracic spine and those that can be found throughout the vertebral column.
Present throughout Vertebral Column
The vertebral column is home to two distinct types of joints:
- Between vertebral bodies – Fibrocartilage intervertebral discs connect adjacent vertebral bodies. A symphysis is a kind of joint made of cartilage.
- Between vertebral arches –framed by the explanation of prevalent and sub-par articular cycles from adjoining vertebrae. It is a synovial kind of joint.
Unique to Thoracic Spine
The verbalizations between the vertebrae and the ribs are extraordinary to the thoracic spine. There are two distinct articulations costotransverse and costovertebral for each rib.
The head of the rib articulates with one of the following in each costovertebral joint:
- The adjacent vertebra’s superior costal facet
- The mediocre coastal feature of the prevalent vertebra
- Intervertebral circle isolating the two vertebrae
The intra-articular tendon of the rib head associates the rib head with the intervertebral plate inside this joint. Due to the close articulation of their components, these joints can only perform slight gliding movements.
The articulation of a thoracic vertebra’s transverse processes and the adjacent rib’s tubercle create the costotransverse joints. They are available in all vertebrae aside from T11 and T12.
Ligaments
Numerous ligaments contribute to the strength of the thoracic spine.
Present Throughout Vertebral Column
- Anterior and posterior longitudinal ligaments: Long tendons that run the length of the vertebral segment, cover the vertebral bodies and intervertebral circles.
- Ligamentum flavum: connects adjacent vertebra’s laminae.
(Note: In the cervical spine, the interspinous and supraspinous tendons thicken and join to frame the nuchal tendon).
Several small ligaments also support the costovertebral joints:
- Radiate ligament of the head of the rib – stretches out from the rib’s head to the two vertebrae’s bodies and intervertebral plate.
- Costotransverse ligament –connects the transverse process to the rib’s neck.
- Lateral costotransverse ligament – extends to the rib’s tubercle from the transverse process.
- Superior costotransverse ligament – reaches the transverse process of the vertebra that is above it from the upper border of the rib’s neck.
Clinical Importance
Thoracic Kyphosis
Kyphosis is an unnecessary curve of the thoracic spine, making the back show up “slouched”. It can happen early on for a number of different reasons. These incorporate unfortunate stances, unusually wedge-formed molded vertebrae (Scheuermann’s kyphosis), and intertwining of vertebrae during improvement.
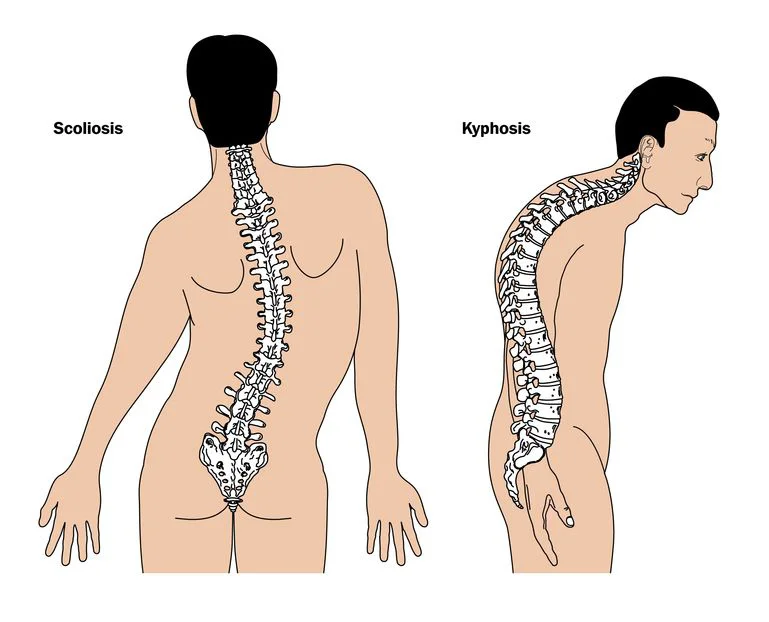
Adult kyphosis can also be caused by a number of illnesses. Osteoporosis, a condition in which bone mass is lost (mostly in older people), is the most common cause. As a result, the spine is less able to support the body’s weight, which causes kyphosis.
The Lumbar Spine
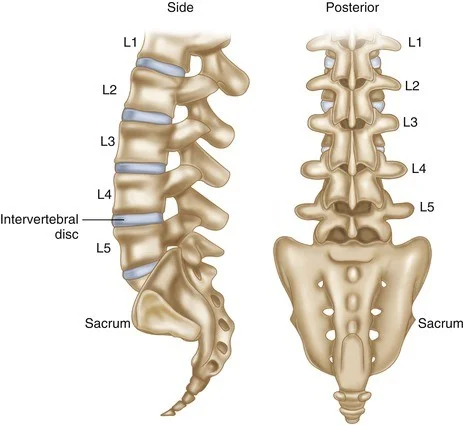
Between the thoracic and sacral vertebrae, in the lower back, is the lumbar spine, the third region of the vertebral column.
It is comprised of five distinct vertebrae, the largest of the vertebral column’s components. As a structure that bears weight, the lumbar spine is supported by this.
This article will take a gander at the osteology of the lumbar vertebrae, inspecting their trademark elements, joints, and their clinical connections.
Structure
Albeit the lumbar vertebrae come up short on of the more unmistakable highlights of different vertebrae, a few qualities help to recognize them.
The vertebral bodies are kidney-shaped and large. The lumbosacral angle is the angle between the long axis of the lumbar region and that of the sacrum because they are deeper anteriorly than posteriorly. The foramen of the vertebrae is triangular.
Other features of a typical lumbar vertebrae:
- Transverse processes are long and slender.
- Articular processes have nearly vertical facets.
- Spinous processes are short and broad.
- Accessory processes can be tracked down on the back part of the foundation of each cross-over process. They serve as anchor points for the deep back muscles.
- Mammillary processes can be found on each superior articular process’s posterior surface. They serve as anchor points for the deep back muscles.
The fifth lumbar vertebrae, L5, has a few unmistakable qualities of its own. Because it carries the weight of the entire upper body, it has transverse processes and a large vertebral body.
Joints
The lumbar spine has two types of joints. Both of these articulations are found throughout the vertebral column and are not exclusive to the lumbar vertebrae.
- Between vertebral bodies – Fibrocartilage intervertebral discs connect adjacent vertebral bodies. A symphysis is a type of cartilaginous joint like this one.
- Between vertebral arches –framed by the explanation of prevalent and sub-par articular cycles from adjoining vertebrae. It is a synovial kind of joint.
Ligaments
A number of ligaments provide support for the lumbar vertebrae’s joints. They fall into two categories: those that are specific to the lumbar spine and those that are found throughout the vertebral column.
Present throughout Vertebral Column
- Anterior and posterior longitudinal ligaments: Long tendons that run the length of the vertebral segment, cover the vertebral bodies and intervertebral circles.
- Ligamentum flavum: adjacent vertebra’s laminae are connected through this ligament.
- Supraspinous ligament: joins the adjacent spinous processes’ tips.
- The interspinous ligament: joins neighboring vertebrae’s spinous processes.
(Note: In the cervical spine, the interspinous and supraspinous tendons thicken and join to frame the nuchal tendon).
Unique to Lumbar Spine
The iliolumbar ligaments help to strengthen the lumbosacral joint, which is located between the L5 and S1 vertebrae. From the L5 vertebra’s transverse processes to the pelvic ilia, these are fan-shaped ligaments.
Anatomical Relationships
The vertebral canal, which is made up of the foramina of all vertebrae, is where the spinal cord travels throughout the vertebral column. The spinal cord comes to an end around L1, and the cauda equina starts. The coccygeal, sacral, and lumbar nerve roots are all in this bundle.
Through the intervertebral foramina, spinal nerves leave the vertebral canal.
Clinical importance
Lumbar Spinal Stenosis
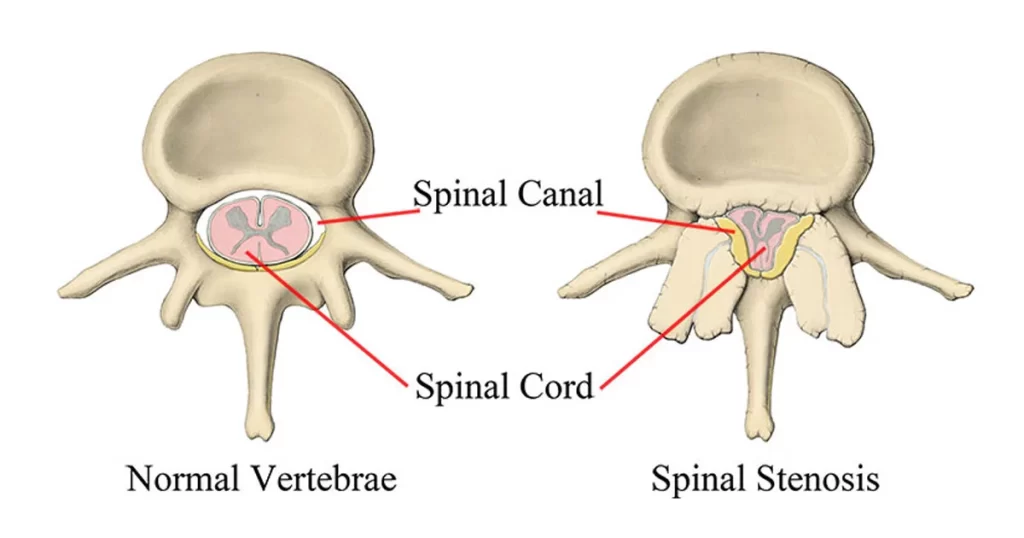
Lumbar spinal stenosis causes a stenotic (narrow) vertebral foramen in one or more lumbar vertebrae, which is thought to be hereditary. The spinal cord and nerves that exit the body may be compressed as a result.
Age-related degenerative changes like intervertebral disc bulging can exacerbate this condition.
A decompressive laminectomy can sometimes be used to treat lumbar spinal stenosis.
Excessive Lumbar Lordosis
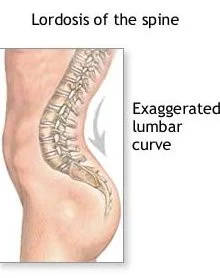
The pelvis is anteriorly tilted as a result of this abnormal anterior curvature of the lumbar vertebral column.
Late in pregnancy, women experience temporary excessive lumbar lordosis, but this goes away after giving birth. Due to the increased weight of the abdomen, obesity can similarly result in lordosis in either sex. Both of these scenarios can result in back pain and are caused by an altered line of gravity.
The Sacrum Spine
The sacrum is a substantial bone that forms the pelvis’s posterior aspect at the end of the vertebral canal. Because it is so thick, it helps support and distribute the body’s weight.
The gross structure of the sacrum, its muscular and ligamentous attachments, the surrounding neuro vasculature, and some pertinent clinical notes will all be examined in this article.
Structure
The sacrum is made up of the five sacral vertebrae that join together. It has a concave, inverted triangular shape. There is a base, an apex, and four surfaces in the bone:
- Base – verbalizes superiorly with the fifth lumbar vertebra and its related intervertebral plate.
- Apex – adjoins the coccyx poorly.
- Auricular surfaces – formed like the outer ear, hence the name, and located laterally on the sacrum. Each explains the ilium’s auricular surface.
- Anterior and posterior surfaces – provide connections to the muscles and ligaments of the pelvis.
Inside, the focal waterway of the vertebral segment proceeds with the center of the sacrum and closures at the fourth sacral foramina, as the sacral break.
Surfaces of the Sacrum
The sacrum has two surfaces: one that is coarse on the dorsal side and relatively smooth on the pelvic side. The patient’s pelvic surface appears anteriorly inferior when standing, while the dorsal surface is in posterosuperior bearing..
Dorsal Surface
The sacrum has a rough and coarse dorsal surface. This can be ascribed to the combination of the sacral vertebrae, which bring about three hard edges (or peaks).
The median sacral crest is a central bone ridge located in the middle of the dorsal surface. The first three sacral vertebrae’s spinous processes fuse to form this structure. Attachment to the supraspinous ligament is provided by it.
The fusion of the sacral articular processes results in the formation of intermediate sacral crests. The back sacroiliac tendons are appended along this peak. It ought to be noticed that the predominant articulating cycle of S1 and the mediocre articulating interaction of S5 isn’t intertwined. Accordingly, the previous explains the sub-par articulating cycle of L5, while the last option – otherwise called the sacral cornu – verbalizes with the coccygeal cornu (the prevalent articulating interaction of the coccyx).
At last, the cross-over cycles of the five sacral bones circuit to frame the horizontal sacral peaks, which offer a place of connection to the back sacroiliac tendons as well as the sacrotuberous tendon. The combination of these cycles is unfinished, permitting the sacral nerve filaments to enter and leave the focal trench via the four sets of back sacral foramina.
Pelvic Surface
The sacrum’s dorsal surface is more impressive than its pelvic surface. Four transverse lines, which are the remains of the fused sacral intervertebral discs (fusion of the sacral vertebrae begins at age 20), mark the adult surface.
The sacral promontory is a bone projection on the superior side that extends anteriorly. It is serially continuous with the ala of the sacrum, the arcuate line of the ilium, the pectin pubis, and the pubic crest of the pubic bone because it forms the pelvic inlet’s posterior margin.
Muscular Attachments
Several muscles in the back and lower limbs originate or attach to the sacrum’s anterior and posterior surfaces. There are those that are connected to the anterior surface and those that are connected to the posterior surface.
Anterior Surface
- Piriformis – Begins from the S2 – S4 level of the pelvic surface. It is able to stabilize the hip joint and externally rotate, abduct, extend, and attach at the trochanter of the femur.
- Coccygeus – muscle embedded on the lower sacrum. Due to its attachment to the coccyx, it is able to flex the bone and supports the contents of the pelvic cavity.
- Iliacus – Although most of its fibers come from the iliac fossa, there are also fibers that come from the ala of the sacrum. Its distal connection to the lesser trochanter of the femur permits it to flex the thigh at the hips and balance out the hip joint.
Posterior Surface
- Multifidus lumborum – the sacrum’s deepest arising muscle. The two upper sacral foramina are partially covered by some of its fibers. This muscle can help stabilize the spine because it attaches to the transverse processes of the superior vertebrae.
- Erector spinae – partially originates from the sacrospinous ligament and the posterior sacrum. It is necessary to achieve head and vertebral column extension and lateral bending.
Neurovascular Relations
The sacrum is close to a number of important structures because it is a part of the vertebral column and pelvic girdle.
Spinal Cord
The focal channel of the sacrum is home to the sacral strands of the cauda equina (a heap of spinal nerves that emerge from the end of the spinal rope). The dural sac, which comes to an end approximately at the level of S2, contains the proximal portions of these fibers.
The arachnoid and dura mater join the filum terminale, a continuation of the pia mater from the conus medullaris of the spinal cord, at the level of S2, where it becomes the coccygeal ligament and attaches to the coccyx.
Autonomic
The average length of the sacral piece of the two trunks extends from the sacral foramina to the pelvic surface of the sacrum. Around here, every trunk has four ganglia.
Vasculature
The middle and horizontal sacral corridors share a nearby physical relationship with the sacrum:
- The median sacral artery – relates to the sacrum in the middle. A continuation of the stomach aorta emerges posteriorly before its bifurcation. The corridor runs along the midline to the coccyx while providing the back rectum, glomus coccygeus (coccygeal organ), and anastomosing with the horizontal sacral conduits and providing meninges and sacrum en route.
- Lateral sacral arteries – a couple of respective vessels that run along the average line of the sacral foramina. They give rise to superior and inferior branches from the internal iliac artery’s posterior division. They also supply the meninges, sacrum, and muscles surrounding it, like the median artery.
Clinical importance
Sexual Dimorphism of the Pelvis
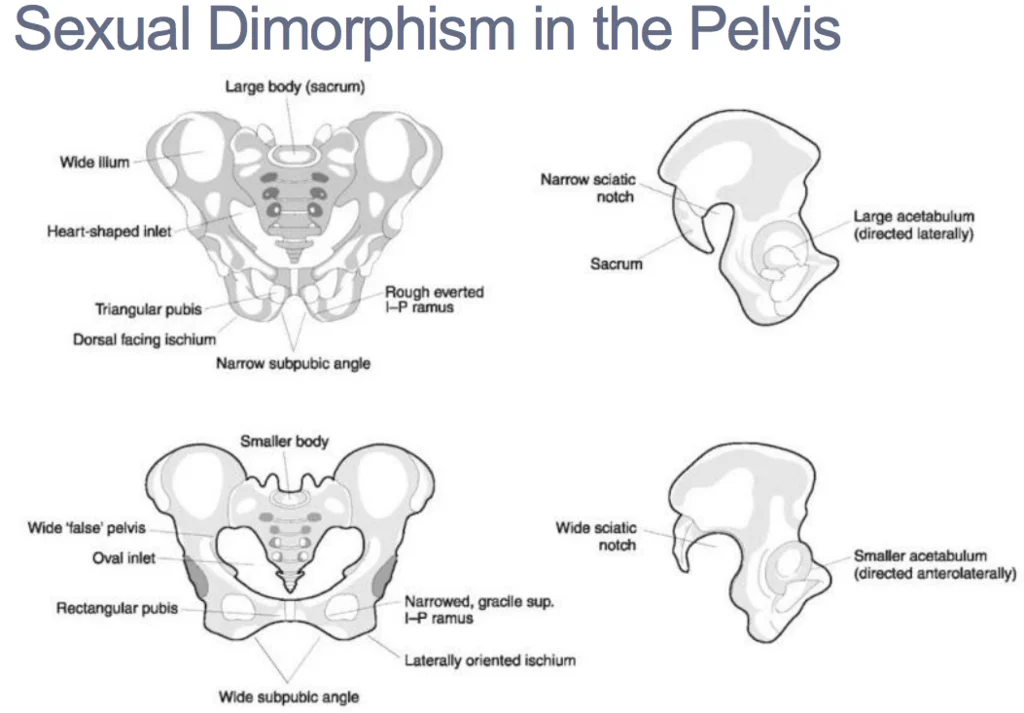
The pelvis exhibits sexual dimorphism because of the sacrum. First, females have less of the sacral promontory than males do. As a result, females’ pelvic inlets are oval-shaped, while males’ are heart-shaped.
In addition, measurements of true conjugate (from the top of the symphysis pubis to the promontory) and diagonal conjugate (from subpubic angle to promontory) are wider with a smaller promontory. A child can move through the wider space during delivery.
The Coccyx Spine
The coccyx, also known as the tailbone, is the vertebral column’s terminal segment. It is contained four vertebrae, which break to create a three-sided shape.
The coccyx’s anatomy, including its structure, bony landmarks, ligaments, and clinical significance, will be the subject of this article.
Structure
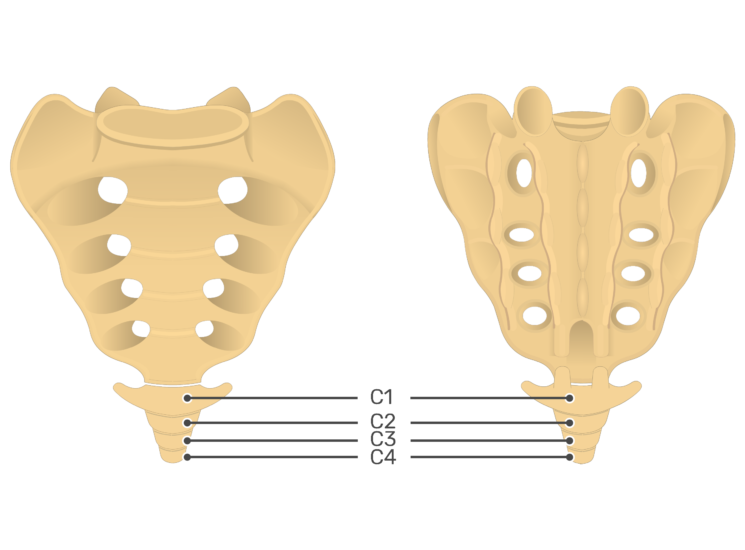
The skeletal remnant of the caudal eminence, which is present from weeks 4 to 8 of pregnancy, serves as the embryological starting point for the coccyx. After that, this eminence falls, but the coccyx stays. The four coccygeal vertebrae are initially distinct, but over time, they fuse to form a single, continuous bone.
There is significant variety in structure between people. The failure of the first coccygeal vertebra (Co1) to fuse and remain separate throughout adulthood is one common variant. There might be pretty much coccygeal vertebrae in certain individuals, giving them a coccyx with 5 or 3 vertebrae, separately.
Bony Landmarks
An apex, base, anterior surface, posterior surface, and two lateral surfaces make up the coccyx. A facet for articulation with the sacrum is contained in the base, which is situated most superiorly. The apex is at the end of the vertebral column, inferiorly. The sidelong surfaces of the coccyx are set apart by a little cross-over process, which projects from Co1.
The coccygeal cornua of Co1 are the greatest of the little articular patterns of the coccygeal vertebrae. They project upwards to express the sacral cornua.
Joints
The sacrococcygeal symphysis is a fibrocartilaginous joint at which the coccyx and sacrum articulate.
This area only allows for passive flexion and extension, such as during labor and defecation.
Ligaments
There are five ligaments that support the sacrococcygeal symphysis:
- Anterior sacrococcygeal ligament – a continuation of the spine’s front longitudinal tendon that interfaces the vertebral bodies’ foremost surfaces.
- Superficial posterior sacrococcygeal ligament – connects the coccyx’s dorsal surface to the median sacral crest.
- Deep posterior sacrococcygeal ligament – connects the posterior side of the fifth sacral body to the dorsal surface of the coccyx.
- Lateral sacrococcygeal ligaments – run from the horizontal part of the sacrum to the cross-over cycles of the coccyx.
- Interarticular ligaments – the span between the cornua of the coccyx and the cornua of the sacrum.
Attachments
One of the vital elements of the coccyx is as a connection point for different designs. The levator ani muscle, which is an important part of the pelvic floor, and the gluteus maximus muscle both attach to the coccyx. The anus is supported by the anococcygeal raphe, a thin, fibrous ligament that extends from the coccyx.
Clinical importance
Fractured Coccyx
The coccygeal vertebrae can be fractured in an abrupt fall onto the buttocks, such as when falling off a chair. Although severe fractures may necessitate hospitalization, this condition typically responds well to conservative treatment.
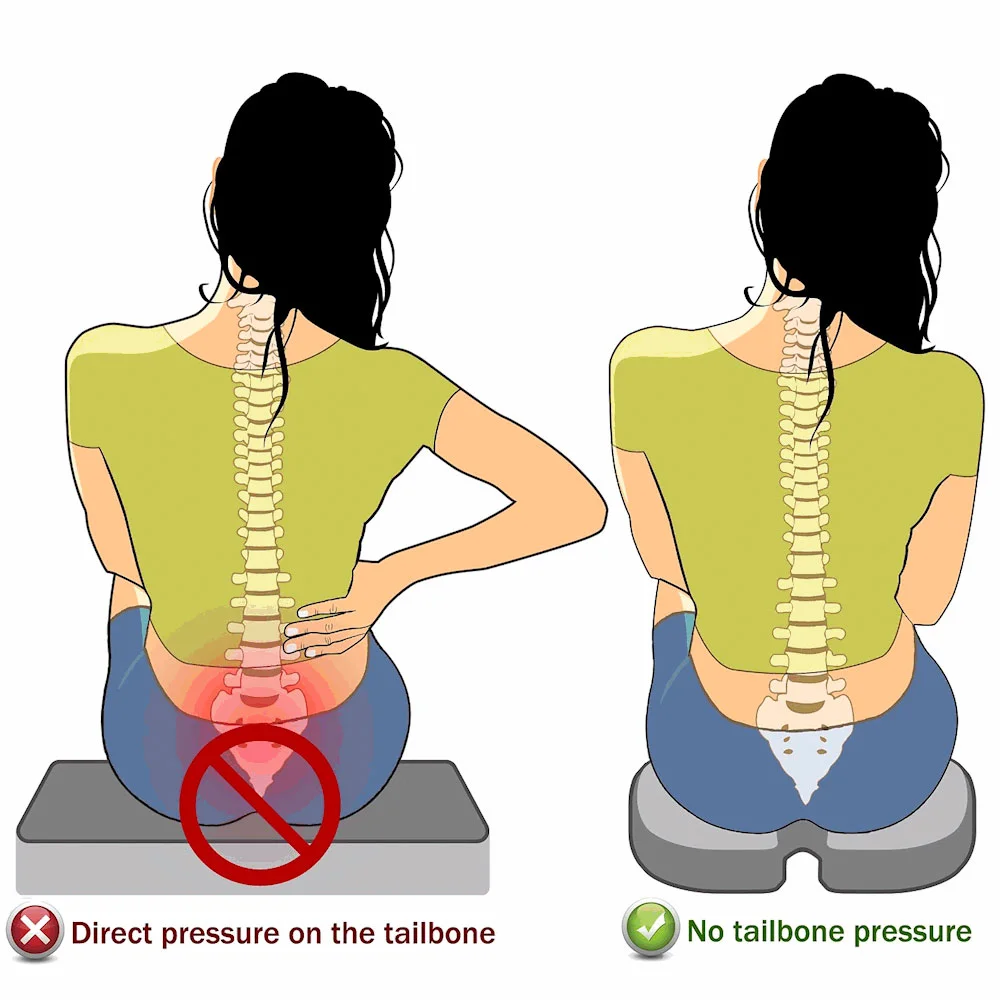
Coccydynia
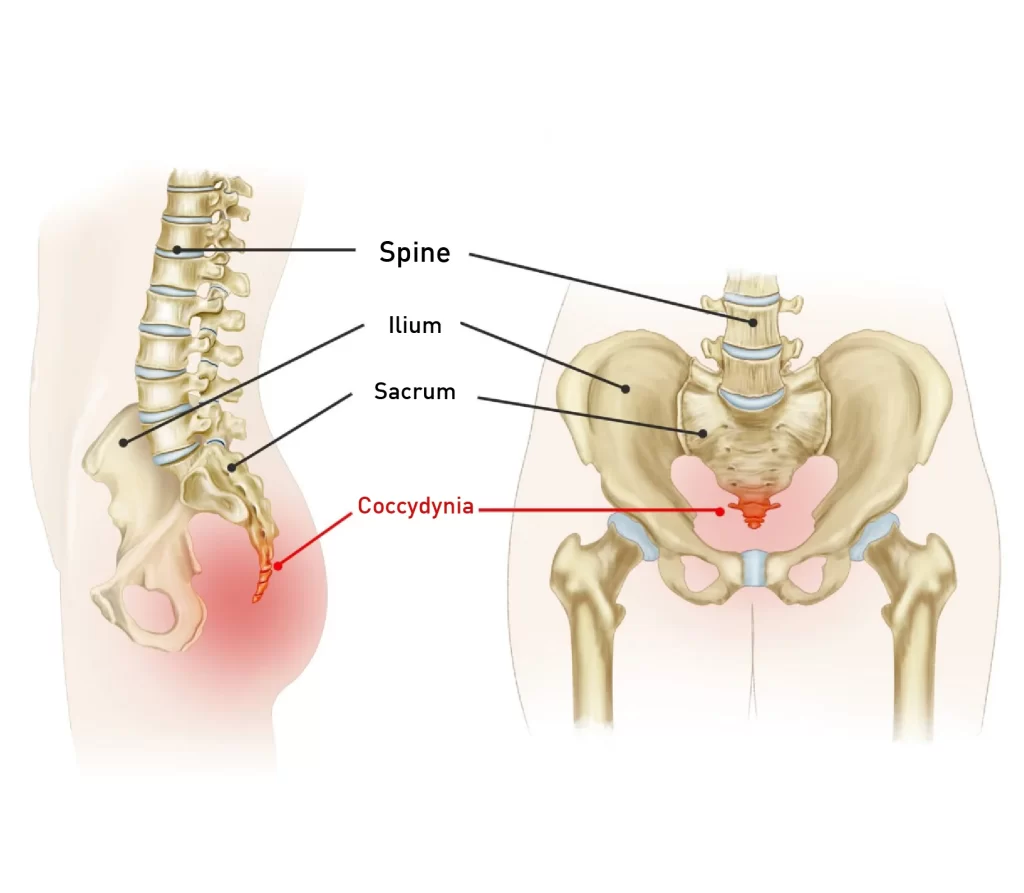
The term “coccydynia” refers to a general feeling of discomfort around the coccyx and has numerous causes. Due to the stretching of the pelvic floor muscles during labor, which puts pressure on their connection to the coccyx and causes pain, childbirth may be the cause. Poor posture while rowing or cycling can also contribute to bone irritation, as can blunt trauma.
Coccydynia is typically an acute condition; however, if the pain persists for longer than three months, it is considered chronic and requires more specialized care.
Sacrococcygeal Teratoma
A tumor of the coccyx known as a sacrococcygeal teratoma is thought to originate from the embryological primitive streak. Although 12% of the time they are malignant and life-threatening, the majority of the time they are benign. They are the most common tumor that appears in newborns and occur in 1/35,000 live births.
FAQs
The vertebral segment, otherwise called the spinal column, is the central axis of the skeleton in all vertebrates. The vertebral column serves as a location for hemopoiesis, supports the trunk, shields the spinal cord and nerve roots, and provides muscle attachments.
Cervical Spine
This district comprises seven vertebrae, which are contracted C1 through C7 (start to finish). These vertebrae support the skull, provide protection for the brain stem and spinal cord, and enable a wide range of head movement.
33 vertices
The vertebrae are the 33 separate bones that connect to form the spinal column. The regions of the vertebrae are designated by numbers: cervical, thoracic, lumbar, sacrum, and coccyx
These conditions may include:
Tumors.
Spinal stenosis.
Herniated discs.
Abscess.
Hematoma.
Vertebral fractures.
Degenerative disc disease.
Of all the vertebrae, L5 has the largest body and transverse processes. The height of the body is greater in the anterior region than in the posterior region. The lumbosacral angle between the sacrum and the lumbar region of the vertebrae is created as a result of this.

5 Comments