Jersey Finger
A flexor tendon rupture, or “jersey finger,” refers to the tendon that causes the fingertip to bend downward. Its term is derived from football players who have grabbed the jersey of an opponent who is attempting to flee. The finger, which is still attempting to bend and grab, unexpectedly straightens as the player struggles to release themselves.
The tendon is tugged in two different directions as a result, creating a tug of war. This may cause the tendon at the tip of the finger to separate from the bone where it was inserted. Sometimes, a fragment of the bone is also pulled off. While this is a classic illustration, a jersey finger can result from different sports and hobbies (like rock climbing). Sometimes, a fragment of the bone is also pulled off. While this is a classic illustration, a jersey finger can result from different sports and hobbies (like rock climbing). The forearm is where most of the tendons that move your fingers start.
The fingertip is bent downward by the flexor digitorum profundus (FDP) muscle. Consequently, FDP avulsion is the medical word for a “jersey finger”. Type I, II, and III are the three categories. The most severe type, Type I, involves complete tendon retraction into the palm. The best type is Type III. There is little to no tendon retraction in this. Each joint has a blood supply for the flexor tendon. As a result, more of the blood supply is cut off as the tendon retracts farther from the tip towards the base of the finger. The speed of your recovery and the outcome of your treatment may be impacted by a loss of blood supply.
Table of Contents
Anatomy:
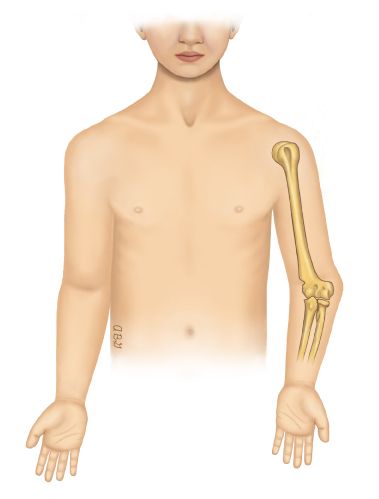
The index finger, middle finger, ring finger, and little finger are the only four non-thumb digits that have three phalanges, which are arranged in a row like box cars on a railway. The proximal phalanx, which is closest to the palm, the intermediate phalanx, and the distal phalanx, which is farthest from the palm, are the names of these bones. The proximal interphalangeal joint (PIP, between the proximal and middle phalanx) and the distal interphalangeal joint (DIP, between the middle and distal phalanx) are the names of the joints that connect these bones.
Long tendons that originate in the forearm travel to the fingers and attach at various locations on these bones. These muscles contract, and their tendons pull on their bone attachments, flexing and stretching these digits. The deepest flexor in the anterior forearm, the flexor digitorum profundus (FDP) muscle releases four tendons that enter the hand through the carpal tunnel and connect to the distal phalanx in each of the four non-thumb digits.
What is a Jersey finger?
Jersey’s finger is a common flexor tendon injury that affects athletes who play contact sports. The forearm muscles are connected to the bones in the fingers by flexor tendons, which are long, fibrous cords. These tendons serve as a pulley that allows your fingers to bend when your muscles contract. Jersey finger, which can be fatal, can occur when the flexor tendon at the finger’s tip is torn or pulled away from the bone in the finger’s distal phalanx.
The Jersey finger, also known as the sweater finger or rugby finger, is a type of injury in which the volar aspect of the distal phalanx base of the flexor digitorum profundus (FDP) is avulsed. Due to the ring finger’s anatomically weaker FDP insertion than the middle finger’s, it often affects the fourth digit. In the grasping position, the ring finger is the most vulnerable to FDP avulsion, which prevents it from flexing at the DIPJ.
A Jersey’s finger occurs when a player grabs another player’s jersey while that player is pulling away, for instance, and a force into DIP hyperextension resists a significant contraction of the FDP tendon. A jersey finger injury that results in a complete rupture of the FDP tendon results in the loss of active DIP joint flexion because the FDP is the only tendon that flexes the DIP joint. A jersey finger injury affects the ring finger the most frequently, accounting for 75% of all instances. In approximately 90% of people, this is thought to be related to the ring digit being 5 millimetres more prominent during grip.
If it is not surgically repaired, it can cause the end of the finger to lose its ability to flex. When a player grips a teammate’s jersey with one or more fingers while the other is pulling or fleeing, they frequently suffer an injury. It is the most prevalent injury to the closed flexor tendon and affects the ring finger in 75% of cases.
Causes of Jersey Finger:
A traumatic rupture of the flexor digitorum profundus (FDP) tendon at its attachment to the distal phalanx is termed as a Jersey’s finger. When one player grabs another player’s jersey with the tips of one or more fingers while that player is pulling or running away, this injury frequently occurs in American football. While the proximal portion of the finger is flexed, the force of this action causes the tip of the finger to hyperextend at the DIP joint.
The FDP tendon at or near its attachment point on the distal phalanx can be partially or completely ruptured by this action. When the force is strong enough, a piece of the phalangeal bone to which the tendon can be attached can be pulled off or avulsed. This injury is common in football, but it can also happen in other sports or activities.
The torn FDP ligament may either withdraw somewhat and stay in the finger close to the PIP joint after the injury, or it might withdraw all the more completely into the centre of the hand. A jersey finger injury in which the FDP tendon has been destroyed completely prevents an individual from independently flexing the affected digit at the DIP joint.
Stages and classification of injury:
The degree of tendon retraction and the presence or absence of a fracture determines the classification of a jersey finger injury. Leddy and Packer first described Types I-III in 1977, and two more have since been added, Types IV and V.
- Type I: At the lumbrical origin, the FDP tendon retracts to the palm.
- Type II: At the proximal interphalangeal (PIP) joint, the FDP tendon retracts to the A3 pulley.
- Type III: A large bony fragment’s avulsion. Because the bone fragment prevents further retraction, the FDP tendon and fracture fragment retract to the A4 pulley.
- Type IV: Avulsion of a substantial chunk of bone and subsequent rupture of the FDP tendon attached to the bony fragment. The avulsed FDP retracts into the pelvis because it is not attached to the bone fragment.
- Type V: A large bony fragment avulsion is accompanied by another significant distal phalanx fracture.
Signs and Symptoms of Jersey Finger:
Athletes with jersey fingers can’t straighten the injured finger. Other common symptoms include:
- Pain in the fingertip
- Unable to bend the distal interphalangeal joint
- Tenderness
- Swelling
- Bruising felt after 2 days
- occasionally, a lump in the finger’s palm
- Although the finger can still be bent with force, it is unable to bend normally.
- It’s possible that you experienced a “snap” at the time of the injury.
- It very well might be feasible to feel the ligament as a clustered up delicate mass on the palm side of the hand.
Diagnosis:
History and physical examination are frequently used to make the diagnosis. Jersey’s fingers are frequently missed by patients and other physicians who do not specialize in hand surgery. They won’t notice that the fingertip isn’t moving, but they will notice that the first two finger joints are bending.
Sometimes people notice that their fingertip isn’t moving, but they think it’s because of pain or swelling. Your hand surgeon may try to isolate your movement during the diagnosis by testing your ability to move the fingertip while holding your knuckle joint straight to prevent it from bending. You most likely ruptured the tendon if it does not move. In order to determine whether the disrupted tendon has chipped off a piece of bone, your doctor may order X-rays.
Physical examination, as well as X-rays and ultrasound, are important to rule out fractures in athletes with finger pain and to link these injuries to sport-related trauma. MRI can assist in a thorough evaluation of the injury and may help identify the extent of tendon retraction, but it is rarely used.
Additionally, a physical examination will reveal that the injured finger continues to extend in relation to the other digits. Additionally, the avulsion can be palpated proximally to the retracted tendon; The DIP joint does not flex, and grip and flexion against resistance are very painful. The x-ray’s anterior-posterior and lateral views may show a bone fragment. In most cases, ultrasound is necessary to evaluate tendon retraction and direct subsequent treatment. Although MRI is rarely used, it can be used to accurately measure the increased distance between the bone and the tendon.
Complications:
Quadriga is possible with tendon advancements of more than 1 cm. The inability to flex the digits next to the injured digit due to increased stress over the healed tendon is known as quadriga.
Additional surgical side effects are:
- Infection
- Skin necrosis
- Tendon repair rupture
- Nail matrix injury
- Adhesions
Treatment of Jersey Finger:
Non-Surgical Treatment:
If, as is uncommon, the flexor tendon was only partially torn, surgery may not be necessary.
A splint might be suggested to the patient to help stabilize the finger and allow the injured tendon to heal on its own.
Non-steroidal anti-inflammatory drugs (NSAIDs) are used to reduce any discomfort or pain caused by the tendon injury.
After 1-3 weeks of immobilization and rest, physical therapy and the use of a splint will help the affected finger regain strength and movement.
Surgical Treatment:
Jersey’s finger is typically treated surgically; conservative measures are only taken when complications make surgery unfeasible. To regain the affected digit’s pain-free active range of motion, surgery is required.
Surgery is definitive treatment and should be performed as soon as possible, typically within three weeks of the injury. DIP joint arthrodesis, tenodesis, and staged tendon reconstructions are surgical salvage options for patients who present late.
Typically performed as an outpatient procedure, the surgery involves locating the flexor tendon, reattaching it to the distal phalanx, and removing the incision from the finger. Screws can be used to reattach an avulsion fragment—a piece of bone that has been pulled off by the tendon—to the bone. It could also be removed if it is small enough.
The FDP is treated with a variety of surgical methods for avulsion injuries, including the following:
- The Bunnell pull-out suture method
- Repairing the tendon with the volar plate as part of the procedure
- The latter is the most recent of the techniques that have been described, and clinical outcome studies are still in the process of being developed.
- The pull-out suture method has always been the most common one. With good postoperative rehabilitation, patients should be able to return to sports and normal activities within 8 to 12 weeks.
If your tendon has been completely torn, you’ll need surgery to reattach it to the bone. Your tendon must be reattached as soon as possible, preferably within ten days. Put your finger down. Inflammation and pain can be reduced by using ice or cold therapy. Seek medical attention immediately if you cannot move your finger and it is stuck in an extended position. In order to confirm the diagnosis and determine whether you have an avulsion fracture, X-rays or ultrasound scans may be required.
Typically, surgery is required to repair injuries to Jersey’s finger. The distal phalange of your tendon must be reattached as soon as possible. The condition’s rehabilitation is crucial because improper treatment can cause flexor tendons to become extremely stiff. It’s important to move quickly after surgery to avoid stiffness.
The most common treatment for injuries to the jersey finger is surgery. For blood supply and function to be restored, prompt treatment is essential. The mesotendon’s blood vessels—the long and short vincula—provide flexor tendons with nourishment. In cases of high-risk surgical patients, there have been few reports of conservative treatment.
A rapid increase in activities may hinder a successful recovery. On the other side, stiffness could happen if there isn’t enough mobility quickly enough. If your range of motion is restricted, a subsequent procedure known as a tenolysis may be required.
Surgical Management:
- Acute: within three weeks of injury.
Without a break: tendon reinsertion (mini-suture anchor) or direct tendon repair
Part of a fracture: calls for internal fixation and open reduction (wires, mini-screws). Bony avulsions are currently being treated with suture anchors as well.
Acute injuries can be treated in a variety of ways that have been demonstrated and described. It doesn’t seem like any of these are significantly better than the others. - Chronic: over three months since the injury.
The two-stage ligament joining (in the event that the full scope of movement is available).
DIP joint arthrodesis (if there is persistent stiffness) Each patient must be carefully discussed prior to joint arthrodesis. Tendon reconstruction may become a viable alternative because some patients may require the distal interphalangeal joint motion for their occupations or hobbies. Unfortunately, for a successful long-term rehabilitation outcome, tendon reconstruction necessitates a significant amount of patient time.
Physiotherapy Management:
Following surgical treatment, athletes can anticipate a loss of play for eight to twelve weeks.
- Dorsal Blocking Splint (DBS)
- Passive range of motion (ROM) exercises in the early postoperative phase
- Active or assisted ROM exercises
- Place and hold exercises
- Strengthening/power grasping exercises
- Scar massage
- Tendon gliding exercises
A sport-specific hand rehabilitation protocol is considered for athletes following surgery in light of their position during play and level of competition.
Putty exercises and hand therapy balls, for example, may be suggested as strengthening exercises. Exercises for strengthening the wrist:
Putty Exercises (Variable): You can use putty to strengthen the hand and wrist’s small muscles. This is helpful after injuries like a wrist, thumb, or finger sprain or a fracture of any of the small bones in the hand. Pull apart with both hands to strengthen your wrist deviation. You can hold it in one hand and twist it with the other to strengthen your wrist extension. You can squeeze the putty to strengthen your grip.
How is the Jersey Finger Cared For?
At the point when there is a full separation of the FDP ligament, careful fix or re-connection is required frequently with securing the ligament back deep down. A hand therapist is needed for flexor tendon care after surgery. Due to the numerous rehabilitation protocols for flexor tendon injuries, it is necessary to maintain close communication with the referring physician.
The physician and therapist’s preference, the quality of the repair, the patient’s adherence, and the availability of resources all influence the protocol selection. When the tendon is only partially torn, doctors may also ask that a conservative flexor tendon program be followed. A hand therapist often needs to make an orthosis after a flexor tendon injury. For flexor tendon injuries, orthoses should support the hand in a way that protects the tendon and promotes the best possible soft tissue healing.
The orthosis should not irritate or redden the skin. Oval-8 Finger Splints, which come in NEW Oval-8 CLEAR and Classic Beige, are a great option because they can be made with a heat gun. When making thermoplastic splints or custom-fitting them, a heat gun is a “must-have.”
Prognosis:
Early diagnosis results in accelerated therapy with fantastic functional results. Excellent patient-reported outcomes are correlated with surgery performed within 10 days of the accident. Within 8 to 12 weeks, patients who have fully recovered their range of motion and are pain-free can resume their athletic activities.
Dexterity loss and reduction of pinch strength are two functional effects of reduced DIP joint motion. Accurate reduction, high-quality repairs, and a suitable rehabilitation regimen all contribute to postoperative functional and aesthetic outcomes. To maintain finger function, scar contracture prevention is essential.
Patient Education:
Patients should be informed that delaying treatment for jersey finger injuries can lead to chronic pain and a loss of grip strength. It is advised to stop smoking for fracture recovery even if bony-avulsion-type jersey finger injuries have a low nonunion rate.
FAQS:
What is the special test for the jersey finger?
Hold the middle phalanx of the injured finger to isolate the DIP, and urge the patient to aggressively straighten the DIP as part of a special test. If the patient is unable to, the test indicates that the extensor digitorum has been injured. Additionally, you can passively extend the tip and observe whether the patient can maintain it there or if it flexes back into place.
What is the initial treatment for a jersey finger?
A finger splint, ice, and painkillers are frequently used as the first treatments. In order to restore the damaged ligament to its original location, a procedure is needed for Jersey’s fingers. The amount that the tendon moves back determines when to perform the procedure.
Does the jersey finger need surgery?
A diagnosis of acute jersey finger necessitates surgical intervention and typically results in an 8–12 week absence from most contact sports.
What are the complications of jersey finger surgery?
Adhesions, joint contracture, re-rupture, loss of fixation, infection, and quadriga—the inability to flex the digit next to the repair due to increasing stress over the repaired tendon—are complications connected with jersey finger repairs.
What happens if jersey finger is left untreated?
The entire hand’s functionality will be affected if the Jersey Finger is not treated. It may impact one’s ability to handle objects and grip strength. In the beginning, rest and ice are advised to help reduce inflammation and pain, but a visit to the doctor should happen soon after the injury.