Cervical Stenosis: Physiotherapy Treatment
Table of Contents
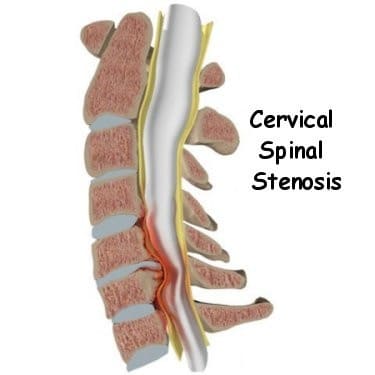
Cervical stenosis Definition
Cervical stenosis is a narrowing of the cervical spinal canal. This narrowing of the spinal canal may result in compression of the spinal cord and/or the nerve roots and affect the function of the spinal cord or the nerve, which may cause symptoms associated with cervical radiculopathy or cervical myelopathy.
Spinal stenosis may occur due to various reason like disc bulging-Herniated disc, spondylosis, trauma around cervical area, tumour or listhesis of cervical spine.

Clinically Relevant Anatomy :
The cervical spinal canal normally provides enough room for neural elements. The sagittal diameter of the spinal canal varies with height and between individuals.
The first cervical vertebral body (C 1) is about 21.8 mm high and the spinal cord makes up about 50% of the spinal canal. On the other hand, C 6 is about 17.8 mm in height and the spinal cord takes up about 75% of the spinal canal.
Average anterior-posterior canal diameter at all levels is 14.1 +/- 1.6 mm.
The canal diameters range from 9.0 to 20.9 mm, with a median diameter of 14.4 mm.
Men have significantly larger cervical spinal canals than women at all of the levels.
Stenosis is usually the secondary consequence of space-occupying lesions
eg. : Progressive disk degeneration, accompanied by
- Disk protrusion
- Ventral spondylophyte formation
- Thickening of the ligamenta flavum
- Hypertrophy of the dorsal facets.
Movement affects the diameter of the spinal canal and cord:
The diameter of the spinal canal in flexion and extension is reduced.
During extension, the ligamentum flavum is folded, which further constricts the spinal canal.
__Changes in length of the spinal canal also affect the length of the spinal cord. eg the shortening of the spinal cord in extension is linked to an increase in diameter and can be additionally damaged by movement. It is pinched between the pincers of the postero-inferior end of one vertebral body and the lamina or ligamentum flavum of the caudal segment. .
Pathophysiology of Cervical stenosis :
__Many theories regarding the pathophysiology of spinal stenosis suggest a number of confluent mechanisms. The spinal cord can be directly compressed by osteophytic bones and ligamentous hypertrophy. Compression of local vascular structures can lead to ischemia of the spinal cord from arterial insufficiency and venous stasis.
__A herniated disk can exert repeated local trauma to the spinal cord or nerve root during repetitive flexion and extension movements, especially in the unstable spine with multiple levels of subluxations.
__In the cervical spine, segments C5-6 and C6-7 are often affected
__Most patients will experience some type of pain associated with the spine but luckily, even without surgery, the majority will have an uneventful recovery. Only 1-3% will have a herniated disc and less than 2% will have compression of a nerve root.
__Spinal stenosis is common with aging but predicting which individual will develop symptoms is not possible. In most cases, the degenerative process can be controlled by changes in lifestyle.
Which are the Cause of Cervical stenosis?
__The backbone (spine) runs from your neck to your lower back. The bones of your spine form a spinal canal, which protects your spinal cord (nerves).
__Some people are born with a small spinal canal. But most spinal stenosis occurs when something happens to narrow the open space within the spine. Causes of spinal stenosis may include:
__Overgrowth of bone: Wear and tear damage from osteoarthritis on your spinal bones can prompt the formation of bone spurs, which can grow into the spinal canal. Paget’s disease, a bone disease that usually affects adults, also can cause bone overgrowth in the spine.
__Herniated disks: The soft cushions that act as shock absorbers between your vertebrae tend to dry out with age. Cracks in a disk’s exterior may allow some of the soft inner material to escape and press on the spinal cord or nerves.
__Thickened ligaments: The tough cords that help hold the bones of your spine together can become stiff and thickened over time. These thickened ligaments can bulge into the spinal canal.
__Tumors:-. Abnormal growths can form inside the spinal cord, within the membranes that cover the spinal cord or in the space between the spinal cord and vertebrae. These are uncommon and identifiable on spine imaging with an MRI or CT.
__Spinal injuries:. Car accidents and other trauma can cause dislocations or fractures of one or more vertebrae. Displaced bone from a spinal fracture may damage the contents of the spinal canal. Swelling of nearby tissue immediately after back surgery also can put pressure on the spinal cord or nerves
Epidemiology :
Cervical spine stenosis appears to be very common and it is estimated that cervical stenosis is present in:
_4.9% of the adult population,
_6.8% of the population fifty years of age or older
_9% of the population seventy years of age or older
__Most patients’ symptoms chronically deteriorate over the years however deterioration can occur rapidly and is then mostly irreversible.
__75% of patients experience phases of neurological deterioration. 5% of all patients with asymptomatic spinal cord compression become symptomatic each year
Risk factors in Cervical stenosis :
_Genetic influence as demonstrated in the study of twins
_Cumulative trauma can lead to the progression of the disease
_Osteoporosis can be a contributing factor
_Cigarette smoking in several epidemiological studies has been shown to lead to back pain and degenerative spinal diseases.
Which are the common Symptoms of Cervical Stenosis?
__Cervical stenosis does not necessarily cause symptoms, but if symptoms are present they will mainly be caused by associated cervical radiculopathy or cervical myelopathy.
__Cervical spondylotic myelopathy can be seen in patients with greater than 30% spinal narrowing, leading to gait disturbance, lower extremity weakness, and ataxia.
__Cervical spinal stenosis can lead to radicular symptoms due to nerve root compression and myelopathy due to spinal cord compression, radicular symptoms are dependent on the level affected eg a C5-6 disk herniation leads to C6 radiculopathy.
–C4-5 disk herniation can lead to deltoid weakness and shoulder paresthesia. Patients also can experience pain and paresthesia in the head, neck, and shoulder.
–C6-7 disk herniation is the most common, leading to a wrist drop and paresthesia in the 2 and three fingers.
–C5-6 disk herniation is the next common, resulting in weakness in forearm flexion and paresthesia in the thumb and radial forearm.
–C7-T1 disk herniation can lead to weakness in the hand intrinsic muscles and numbness in the 4 and five digits.
Potential symptoms include:
- Pain in the neck or arms
- Arm and leg dysfunction
- Numbness or tingling, stiffness or clumsiness in the hands and arm
- Arm and hand weakness
- Diminished proprioception
- Balance and coordination problems, such as shuffling or tripping while walking. Cervical spinal stenosis can be crippling if the spinal cord is damaged.
- Loss of bowel or bladder control (incontinence)
Differential diagnosis :
–Diabetes
–Inflammatory spondyloarthropathy (e.g., ankylosing spondylitis)
–Paget’s disease of the bone
–Peripheral neuropathy (paralysis)
–Peripheral vascular disease
–Spinal cord tumor
–Vascular insufficiency (atherosclerosis of the aorta )
–Vertebral disc disease
Physical Examination :
Start your examination with:
_Therapist takes carefully reviews medical history, which may include family history. Some spinal disorders may be inherited, or the risk is increased if a parent has a history of neck or back pain.
In general, existing medical problems (eg, diabetes, cardiovascular disease), current medications taken (over-the-counter, prescription), previous spine treatments and surgeries, and lifestyle (eg, tobacco and alcohol use, exercise) are vital.
a physiotherapist will ask questions about your symptoms and how your problem is affecting your daily activities. This will include questions about pain, feelings of numbness or weakness, changes in bowel or bladder function, and whether you’ve noticed any changes in the way you walk.
Pain history:- physiotherapist may ask about your symptoms including:
-Describe your symptoms (eg, pain, numbness, tingling sensations)
-When did your symptoms begin?
-Where is your pain? Does it radiate into another part of your body?
-What is the frequency of your symptoms?
-On a scale from 1 to 10 with 10 being the worse pain imaginable, how do you rate your pain now?
-What improves your symptoms? What makes your symptoms worse?
-Does leaning forward or sitting relieve your pain?
Observation (standing) Examination:
__ physiotherapist then does a physical examination to see which neck movements cause pain or other symptoms. Your skin sensation, muscle strength, and reflexes are tested. therapist also watch walk of the patient to see if there are any subtle changes in the walking pattern.
__During the physical examination, inspects patient’s spine for abnormalities (such as kyphosis, scoliosis, abnormal curvature of the spine) and areas of swelling, tenderness, and pain. He/she observes posture, and how patient walk and stand. flexibility and spinal range of motion is assessed as patient bend forward and backward and from side-to-side.
__Assessment of sensation with pinprick and touch in the upper extremity, thorax, and abdomen in the dermatomal regions mentioned above to check for radiculopathy and also in the lower extremity to check for myelopathy.
Posture:
__Observe the patient’s posture in standing and sitting. As a part of the examination, postural deviations can be corrected to determine the effect on the patient’s signs and symptoms.
__common postural deviation:
-Protracted cervical spine or forward head posture
-Protracted shoulder girdle and rounded shoulders
Upper Thoracic Spine
-Kyphotic or Flexed
-Lordotic or Extended
-Normal
Middle Thoracic Spine
-Kyphotic or Flexed
-Lordotic or Extended
-Normal
Movement Tests:
__Functional Movement
__ask the patient to demonstrate the functional movement that most easily replicates their symptoms. The movement that the patient demonstrates can give many clues to the main cause of the problem as well as a good performance-based outcome measure.
__Cervical AROM, PROM, and Over-pressure
__Prior to movement testing the examiner asks the patient about baseline symptom location and intensity. The examiner notes any change in location or intensity during the testing and where in the motion they occur.
__The examiner should assess for the presence of symptom centralisation and peripheralisation during testing. Repeated motions may be utilised as part of this assessment.
__All cervical AROM tests (Neck flexion, extension, rotation, and side-bending) performed with the patient in seated in an upright posture
Passive overpressure may be applied at the end of the active motion to assess for pain response and end-feel.
-Combined motions:-
_Upper cervical flexion and lower cervical extension is assessed with cervical retraction.
_Upper cervical extension with lower cervical extension is assessed with cervical protraction.
_The cervical quadrant involves combined cervical extension with ipsilateral rotation and sidebending.
Palpation:
–Supine
-Palpate bilateral sternoclavicular joints for mobility assessment or tenderness.
-Palpate acromioclavicular joint for mobility assessment or tenderness.
-Palpate suboccipital muscles, upper trapezius, levator scapula, and pectoralis minor to assess shortness or tenderness.
–Prone
-Central and peripheral Cervical and Thoracic Spine
-Palpate ribs 1 – 7 of the upper and mid-thoracic region
-Ribs 1 – 7 posterior to anterior accessory motion
–Seated
-Palpate for tissue texture changes down the medial groove of the cervical and thoracic spine
-Palpate for tissue texture changes on either side of the spinous processes of the cervical and thoracic spine
-Palpate for any scoliotic deviations
Neurologic Assessment:
A neurological examination should be performed if the patient reports numbness or tingling in the back, shoulder, or more distal upper extremities, or if the patient has focal weakness that would indicate nerve involvement.
_Reflexes:
C5 – C6 – biceps
C5 – C6 – brachioradialis
C7 – triceps
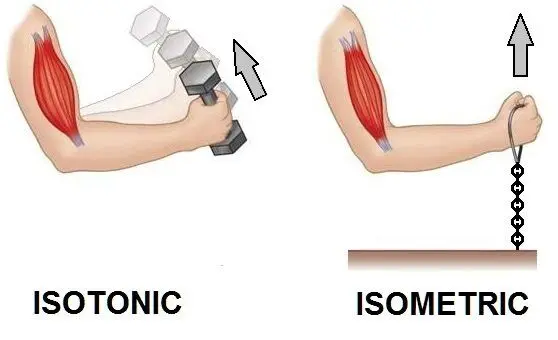
__Manual muscle testing:
*Elbow
-Flexion (C5,C6)
-Extension (C7)
*Shoulder
-Flexion (C5)
-Extension (C6, C7, C8)
-Abduction (C5)
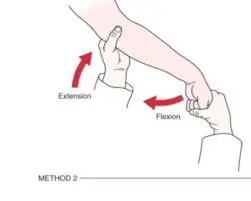
*Wrist
-Flexion (C6 – 7)
-Extension (C6 – 7)
*Finger
-Flexion (C7 – C8)
-Extension (C7 – C8
-Abduction (T1)
*Sensory examination:-
C3 – Occiput
C4 – Supraclavicular space
C5 – Anterior shoulder
C6 – Lateral shoulder
C7 – Posterior arm
C8 – Phalanxes 4 – 5
T1 – Medial arm and axilla
*Spinal Accessory Nerve:
__ Have the patient shrug both shoulders upward against resistance. An inability to shrug bilateral shoulders upward against resistance may indicate a lesion to the spinal accessory nerve.
special test:
Upper Limb Tension Test (ULTT)
__The patient is positioned in supine. During the ULTT that places a bias towards testing the patient’s response to tension placed on the median nerve, the examiner sequentially introduces the following movements to the symptomatic upper extremity.
-Scapular depression
-Shoulder abduction to approximately 90 degrees with the elbow flexed
-Forearm supination, wrist and finger extension
-Shoulder lateral rotation
-Elbow extension
-Contralateral then ipsilateral cervical side-bending
Spurling’s Test
__The Spurling’s test (also known as Maximal Cervical Compression Test and Foraminal Compression Test) is used during a musculoskeletal assessment of the cervical spine when looking for cervical nerve root compression causing Cervical Radiculopathy.
__The patient is seated and asked to sidebend and slightly rotate head to the painful side.
__The clinician places a compressive force of approximately 7 kg through the top of the head in an effort to further narrow the intervertebral foramen.
__The test is considered positive when it reproduces the patient’s symptoms. The test is not indicated if the patient does not have upper extremity or scapular region symptoms.
__Distraction Test (used to identify cervical radiculopathy)
__The patient is positioned in supine.
__The examiner grasps under the chin and occiput, flexes the patient’s neck to a position of comfort, and gradually applies a distraction force of up to approximately 14 kg.
__A positive test occurs with the reduction or elimination of the patient’s upper extremity or scapular symptoms. The test is not indicated if the patient has no upper extremity or scapular region symptoms.
__Valsalva Test
__The patient is seated and instructed to take a deep breath and hold it while attempting to exhale for 2 – 3 seconds. A positive response occurs with the reproduction of symptoms.
Evaluation:
__X-rays:- These can show how the shape of your vertebrae has changed. radiograph is of limited value although dynamic views in flexion and extension modes can demonstrate dynamic instability or spondylolisthesis.
__Magnetic resonance imaging (MRI):-By using radio waves, an MRI creates a 3-D image of your spine. It can show tumors, growths, and even damage to discs and ligaments.MRI is the gold standard; it is able to show intrinsic cord abnormalities, the degree of spinal stenosis, and differentiate other conditions such as tumors, hematoma, or infection
__Computerized tomography (CT scan):- A CT scan uses X-rays to create a 3-D image. With the help of a dye injected into your body, it can show damage to soft tissue as well as issues with your bones. CT can help differentiate calcified disks or bone osteophytes from “soft disks,” differentiate ossification of the posterior longitudinal ligament from a thickened posterior longitudinal ligament and detect bone fractures or lytic lesions.
__ If a patient has a pacemaker and cannot obtain an MRI, a CT myelogram can be performed to identify the level and degree of stenosis
__ electrical tests of the nerves that go to your arm and hand. Electromyography (EMG) test is used to check if the motor pathway in a nerve is working correctly. Doctors may also order a somatosensory evoked potential (SSEP) test to locate more precisely where the spinal cord is getting squeezed. The SSEP is used to measure whether a nerve is able to get and send sensory information such as pain, temperature, and touch. The function of a nerve may be recorded with an electrode placed over the skin or with a needle that is inserted into the nerve or sensory center of the brain.
MEDICAL TREATMENT :
Your doctor may start off with nonsurgical treatments. These might include:
__Medication:- Common pain remedies such as aspirin, acetaminophen (Tylenol), ibuprofen (Advil, Motrin), and naproxen can offer short-term relief. All are available in low doses without a prescription. Other medications, including muscle relaxants and anti-seizure medications, treat aspects of spinal stenosis, such as muscle spasms and damaged nerves.
__Corticosteroid injections:- Your doctor will inject a steroid such as prednisone into your back or neck. Steroids make inflammation go down. However, because of side effects, they are used sparingly.
Some patients are given an epidural steroid injection (ESI). The injection is given in a part of the spinal canal called the epidural space. This is the area between the dura (the material that covers the spinal cord) and the spinal column. It is thought that injecting steroid medication into this space fights inflammation around the nerves and discs. This can reduce the swelling and give the spinal cord more room
__Anesthetics:- Used with precision, an injection of a “nerve block” can stop pain for a time.
__surgical treatment:
__Surgery is for only those who fail repeated nonoperative treatments (aimed at improving symptoms and function rather than preventing neurologic complications) and only considered after attempting nonsurgical modalities, or if a patient’s symptoms result in disability.
-If a patient presents with rapidly progressive neurological deficits or if there is the presence of bladder dysfunction, urgent surgery is necessary
Surgical Treatment of Cervical Spinal Stenosis:-
__The goal of surgery is to take pressure off the spinal cord and/or nerves—this is called decompression. There are different types of decompression procedures to treat spinal stenosis affecting the spinal canal (spinal cord; central spinal stenosis) and/or neural foramen (nerves; lateral spinal stenosis). Sometimes instrumentation and fusion are performed after spinal decompression to stabilize the cervical spine. Alternatively, certain patients may be candidates for motion preserving spinal implants, so-called cervical arthroplasty.
Typical surgical procedures performed to treat spinal stenosis affecting the neck include:-
-Anterior cervical discectomy and fusion (ACDF)
-Laminectomy or laminotomy
-Foraminotomy
-Cervical arthroplasty (ie, artificial disc)
-Corpectomy and strut graft
Laminectomy
__The lamina is the covering layer of the bony ring of the spinal canal. It forms a roof-like structure over the back of the spinal cord. When bone spurs or disc contents have pushed into the spinal canal, a laminectomy is done to take off the lamina bone in order to release pressure on the spinal cord.
__Some surgeons completely remove the entire lamina bone, called a total laminectomy. Others prefer to keep the lamina in place by forming a hinge on one edge of the bone. This hinge is formed by cutting partially through the lamina on one side. A second cut is made all the way through the lamina on the other side. This edge is then lifted away from the spinal cord, and the other edge acts like a hinge. The hinged side eventually forms a bone union, which holds the opposite side open and keeps pressure off the spinal cord.
_Anterior Cervical Discectomy and Fusion
__A fusion surgery joins two or more bones into one solid bone. Fusion of the neck bones is most often done through the front of the neck. The surgeon takes out the intervertebral disc (discectomy) between two vertebrae. A layer of bone is shaved off the flat surfaces of the two vertebrae to be fused. This causes the surfaces to bleed and stimulates the bone to heal. (This is similar to the way two sides of a fractured bone begin to heal.)
__ A section of bone is grafted from the top part of the pelvis bone and inserted into the space where the disc was taken out. This separates the two vertebra bones, taking pressure off the spinal cord. As the bone graft heals in place, the vertebral bones fuse together into one solid bone.
_Corpectomy and Strut Graft
__A corpectomy relieves pressure over a large part of the spinal cord. In this procedure, the surgeon takes off the front part of the spinal column and removes several vertebral bodies. The spaces are then filled with bone graft material. Metal plates and screws are generally used to hold the spine in place while it heals. A corpectomy is used in cases of severe spinal stenosis.
PHYSIOTHERAPY TREATMENT:
__Nonoperative treatments, such as physical therapy management, are aimed at reducing pain and increasing the patient’s function. Nonoperative treatments do not change the narrowing of the spinal canal, but can provide the patient of a long-lasting pain control and improved function without surgery. A rehabilitation program may require 3 or more months of supervised treatment.
A physiotherapy program may include:
Controlling your pain and symptoms:
1)Rest: – Resting the painful joints and muscles helps calm soreness, giving your neck time to heal. If you are having pain with an activity or movement, it should be a signal that there is still irritation going on. You should try to avoid all movements and activities that increase your pain. In the early stages of your problem, your doctor or therapist may want you to use a soft or hard neck collar to limit neck movement nearly completely.
2)Specific Rest:- Specific rest encourages safe movement of the joints and muscles on either side of a painful area, while protecting the sore spot during the initial healing phase. Select exercises can be given to encourage safe movement of the shoulders and upper back. If you’ve been prescribed a collar, you will likely be instructed to take it off a few times a day so you can do some gentle and controlled exercises.
Soft Neck Collar:- At first, we may suggest immobilizing the neck. Keeping your neck still for a short time can calm inflammation and pain. We instruct patients to restrict their daily activities by avoiding heavy and repeated motions of the neck, arms, and upper body.
__Our therapist may also prescribe a soft neck collar. The collar is a padded ring that wraps around the neck and is held in place by a Velcro strap. Patients wear the collar during waking hours, usually for up to three months. Then they slowly begin to taper the amount of time they wear it each day. After wearing a neck brace for up to three months, most patients slowly resume their routine activities.
3)Positioning: The results of the evaluation will give your therapist a clear picture of ways you can position your neck for the greatest comfort. A special pillow, called a contour pillow, may be suggested to help get your neck in the most comfortable position while sleeping or resting. A commercial neck roll, or even a rolled towel, can be slid inside your pillow case so that when you lie back, the roll fills in and supports the curve in your neck. Other special ways to rest your head and neck may be given by your therapist to help take away arm pain that is coming from your neck.
4)Ice: Ice makes the blood vessels in the sore area become narrower, called vasoconstriction. This helps to control inflammation that is causing pain. Some ways to put ice on include cold packs, ice bags, or ice massage. Cold packs or ice bags are generally put on the sore area for 10 to 15 minutes.
__ Ice massage is done by rubbing an ice cube or ice cup on a sore spot or tender point. It’s as easy as freezing a small paper cup full of water. Once the water freezes, simply tear off the top inch of the cup and rub the exposed ice on the sore spot for three to five minutes, or until it feels numb.
5)Heat: – Heat makes blood vessels get larger, called vasodilation. This action helps to flush away chemicals that are making your neck hurt. It also helps to bring in nutrients and oxygen which help the area heal.
__True heat in the form of a moist hot pack, a heating pad, or warm shower or bath is more beneficial than creams that merely give the feeling of heat. Hot packs are usually placed on the sore area for 15 to 20 minutes. Special care must be taken to make sure your skin doesn’t overheat and burn. It’s also not a good idea to sleep with an electric hot pad at night.
6)Ultrasound:- An ultrasound machine produces high frequency sound waves that are directed toward the sore area. Passing through the body’s tissues, these waves vibrate molecules. This causes friction and warmth as the sound passes through the tissue. The rest of the sound changes to heat in the deeper tissues of the body.
_This heating effect helps flush the sore area and brings in a new supply of nutrient and oxygen-rich blood. Ultrasound treatments are a way for your therapist to reach tissues that are over two inches below the surface of your skin.
7)Phoresis:- This means to “carry or transmit.” There are two methods that therapists can use to transmit substances across the skin. Phonophoresis uses the high-frequency sound waves of ultrasound to “push” a steroid medication (cortisone) through the skin.
__ Iontophoresis uses a small machine that produces a mild electrical charge, which is used to carry medicine, usually a steroid, through the skin. The steroid is a very strong anti-inflammatory medication that actually stops the pain-causing chemical reaction within the cells of the sore tissue in your body. Either type of phoresis may be used in place of a cortisone injection.
8)Electrical Stimulation:- This treatment stimulates nerves by sending an electrical current gently through your skin. Some people say it feels sort of like a massage on their skin. Electrical stimulation can ease pain by sending impulses that are felt instead of pain.
__Two respected scientists discovered a theory, called the Gait Theory. This theory says that when you feel a sensation other than pain, like rubbing, massage, or even a mild electrical impulse, your spinal column will actually “close the gate” and not let pain impulses pass to the brain. In the case of electrical stimulation, the electrical impulses speed their way across the skin and onto the central nervous system much faster than pain.
__By getting there first, the electrical information “closes the gate” to pain, blocking its passage to the brain. Once the pain eases, muscles that are in spasm begin to relax, letting you move and exercise with less discomfort. Other settings on the machine can be used to help your body release endorphins. These are natural chemicals formed within your body that behave like a strong drug in reducing the perception of pain for up to eight hours at a time.
9)Soft tissue mobilization/massage:- Physical therapists are trained in many different forms of massage and mobilization when treating the neck. Massage has been shown to calm pain and spasm by helping muscles relax, by bringing in a fresh supply of oxygen and nutrient-rich blood, and by flushing the area of chemical irritants that come from inflammation.
__Soft tissue treatments can help tight muscles relax, getting them back to a normal length. This will help you begin to move with less pain and greater ease. Physical therapists have special training in a variety of different ways to mobilize or massage.
__These can include gentle strokes, called effleurage. Myofascial release techniques help restore better movement by getting the thick layer of fascia below the skin and around muscles to “give”. Strain-counter-strain is a type of therapy that is especially helpful when tender points are causing muscles to restrict movement.
10)Joint mobilization:- These are graded pressures and movements that are done by skilled physical therapists. Gentle graded pressures help lubricate joint surfaces, easing stiffness and helping you begin moving with less pain. Pain that is left unchecked can quickly uncomfortable “cycle of pain and muscle guarding.” In other words, the pain can make your muscles go into spasm, in which your muscles try to guard the sore joints, keeping you from wanting to move your neck at all.
__ When movement stops, your brain gets an uninterrupted flow of pain sensation. Ouch! This leads to a cycle of even more muscle spasms and pain because your muscles try to “protect” you from painful movement.
__By applying gentle pressures, or mobilizations, your therapist will begin to halt the flow of pain information, which helps muscles relax. Once your muscles begin to relax, you will begin to feel other sensations than pain. As your pain eases, more vigorous grades of mobilization may be used to lengthen tissues around the joint helping restore better movement in your neck.
11)Traction:- Sore joints and muscles in the neck often feel better when a traction “pull” is used. Your therapist will test at first to see if you can get relief with this type of treatment. Traction can be done in a variety of ways.
__ There are traction machines that allow you to relax comfortably with either a halter or cushion behind your neck. The machine is set to pull on this halter or cushion for a certain amount of time and pressure.
__ Manual traction is another way for your therapist to put a graded pull on your neck. There are also traction devices that can be issued for you to use at home. The amount of pull that is used will depend on your condition. A gentle on/off pressure may be better early on to help control pain or if there is pain from arthritis. More vigorous traction can help take away pain if a joint is mildly sore or tight.
Exercises:
1)Strengthening your neck
__Exercise is important during all stages of recovery from neck pain. Different types of exercises will be used by your physical therapist as you get better. In the early stages, when your neck is still quite painful, specific exercises may be suggested to help reduce your pain. Supporting your neck in certain positions as suggested by your therapist can take pressure off sore or injured areas. These positions are sometimes easier to get into by using a pillow, rolled towel, or commercial neck roll. You may need to relax back on a recliner or mattress for best results.
__ In cases of significant pain, you may be given a set of breathing exercises. Deep, diaphragmatic breathing helps air to reach even the lower lobes of your lungs. Combining deep breathing to a slow relaxing count can help muscles relax, while bringing much-needed oxygen to sore tissues. Neck pain can be physically and emotionally draining. Relaxation exercises may not correct your problem, but they can help control pain and its accompanying stress.
__Movement is also important, even when your neck is still painful. Careful movements suggested by your therapist can safely ease pain by providing nutrition and lubrication to injured and sore areas. The movement of joints and muscles also signals the nervous system to block incoming pain.
__Common movement exercises include active range of motion, in which you are encouraged to move your neck toward directions that don’t hurt. Your therapist will evaluate which movements will be safest and best for you. In some cases, pain will ease with the addition of pressure into one or another direction. Again, your therapist will need to determine which movements are best for your condition. Avoid movements that hurt or seem to irritate the soreness in your neck.
__As your neck becomes less painful, the exercises will be changed to focus on improving the overall health of your neck. These changes will focus on exercises for:
1)Flexibility
2)Strength
3)Coordination
4)Aerobic conditioning
__Exercises that increase flexibility help to reduce pain and make it easier to keep your neck and spine in a healthy position. Tight muscles cause imbalances in spinal movements. This can make injury of these structures more likely. Flexibility exercises for the neck, chest, and upper shoulders can be helpful in establishing safe movement. A slow progression of stretching exercises can increase flexibility in these areas, ease pain, and reduce the chance of reinjury.
__The next stage of exercise focuses on the strength of the muscles that support the neck. These muscles help bring the spine into a safe position–and keep it there! Trained muscles can keep your neck healthy by getting it into better posture. A series of strengthening exercises, called stabilization training, is a way to get better balance in the muscles around your neck, chest, and upper back.
__ These stabilization exercises are helpful in supporting your neck in safe positions while you are working or when you are doing other daily activities. Strengthening and stabilization exercises are simple to do at home and don’t have to require any expensive equipment. By practicing these exercises often, you will become comfortable keeping your neck in healthy positions and postures with all your activities.
__Strong muscles need to be coordinated. As the strength of the spinal muscles increases, it becomes important to train those muscles to work together. Learning any physical activity takes practice. Muscles must be trained so that physical activity is under control. Muscles that are trained to control the safe movement of the spine help reduce the chance of injury. You will be taught exercises to help train your neck, chest, and upper back muscles to work together in protecting your spine.
__Finally, attention will be directed to increasing your overall fitness. The word aerobic means “with oxygen”. By using oxygen as they work, muscles are better able to move continuously, rather than in spurts. Fitness training allows the muscles to become more efficient at obtaining nutrients and oxygen from the blood. As the muscles use up the nutrients and oxygen, chemical waste products are created that can cause pain. Training also increases the ability of muscles to get rid of these waste products.
__Exercise has other benefits as well. Vigorous exercise can cause chemicals called endorphins to be released into the blood. These chemical hormones act as natural pain relievers in reducing your pain. It will be important that you pick an aerobic activity you can enjoy and stick with it.
__Once your pain is controlled, your range of motion is improved, and your strength is returning, you will be progressed to a final home program. Your therapist will give you some ideas to help take care of any more soreness at home. You’ll be given some ways to keep working on the range of motion and strength too. Before you are done with physical therapy, more measurements will be taken to see how well you’re doing now compared to when you first started in therapy.
Prevention and long-term self-care for the neck:
1)Posture: – Using a healthy posture is like holding a defense shield against future neck problems. Pain and injury CAN be prevented. When your joints are positioned in their safe—or neutral posture—the body works like an elegant machine. It works safely and even more productively. When unbalanced postures are used, problems are more likely to happen.
__ Prevention of neck pain and injury has a lot to do with keeping a balanced position of the spine and extremities. When standing, this balance follows a plumb line from ear to ankle. In a seated position, this line descends from the ear to the hip. A rule of thumb for the extremities is to keep them in their relaxed positions.
__There are three natural curves in the spine. From a side view, the neck (cervical spine) curves slightly inward. The mid-back (thoracic spine) curves slightly outward. The low back (lumbar spine) curves slightly inward. Keeping this relationship while standing, sitting, or moving is the basis for healthy posture. When moving, bend at the hips to avoid rounding or straightening the spine. This keeps the spine safe during activities like lifting and walking.
__For better sitting posture, sit with a good upright alignment of the spine by using a comfortable chair designed to support correct posture. Avoid slouching by keeping your low back against the back of the chair. Bending the head forward strains the neck and affects the nerves and arteries leading to the arms. Your shoulders should be relaxed, and the elbows, hips, and knees should be bent at right angles (ninety degrees). Avoid pressure to the back of the knees. Your feet should be kept flat on the floor or supported by a foot-rest.
__Awkward posture places stress on the body that can lead to neck pain. Slouching with the spine or leaning the head forward puts the body out of alignment, causing the limbs to be stretched and bent. Too much bending (flexion) or straightening (extension) in the spine increases the risk of injury. Symptoms of pain, tingling, or numbness in the arm or hand may also come from poor neck posture. The slight inward curve of the neck balances the head on the spine. Avoid extreme postures, like gazing up at the stars, or bending your head down for long periods when reading a book. Keeping a balanced posture is a measure you can use to prevent further injury and pain in your neck.
2)Ergonomics:- Ergonomics is a look at the way people do work. What does ergonomics have to do with the ache in your neck? It could have a lot to do with it. It’s possible that even minor changes in the way you do your work or hobby activities could ease the pain you feel now while preventing further neck injury or pain.
__In some cases, it is best to have someone trained in ergonomics, like a physical or occupational therapist, check your work station and the way you do your work.
__ The first step will be for them to ask you some questions about your work, which makes good sense. Since you’re the one doing the job, you will have an expert opinion about what seems to be working, what could be done differently, and what tasks seem to be causing the most problems for you. Once these questions are covered, the evaluator will want to watch you do the work tasks.
__Areas that will be noted include the postures you use, repetitions to complete the task, rest time between tasks, and the amounts of weight you are dealing with. For office workers, the examiner will look at alignment of the computer monitors, chairs, desk heights, etc. Other areas that may be evaluated include work heights, tools of the trade, lighting, and temperature.
__It’s also helpful to look at your work postures and work tasks to see if what you are doing can be done with less stress and strain on your body.
__When the work site evaluation is over, you or your supervisor will probably be given some recommendations—some of these may even be ones you came up with! Ergonomics doesn’t always have to involve expensive changes. Even minor adjustments can make a huge difference in easing your pain and preventing further problems.
3)Work Place Strategies:- These strategies are ideas of how to work with greater safety and even better productivity. Have you ever felt stress or tension at work? Chances are good that you wouldn’t have a pain or worry if you didn’t. The reality is that people are often called on to do even more with less resources.
_They are faced with more responsibility and more deadlines to get their tasks done. The health of your neck may be at risk with these mounting pressures. But scientists have helped us learn that there is a defense in the face of these mounting pressures. They have shown the importance of using the “Three R’s” to help ease tension and reduce neck pain at work:
4)Rest: – This includes taking frequent breaks during the work hour. It also means choosing alternate activities to get your mind ready for a new job task. Activities include deep breathing, walking, napping, or exercising.
5)Relaxation:- Take a load off. Lie back. Turn down the lights, and listen to your favorite tape or CD. Attempt to breath slowly and deeply, allowing your abdomen to rise and fall rhythmically. Using visual imagery can also aid in relaxation. Try to visualize each muscle relaxing one after another.
6)Recovery: – Our bodies need a chance to heal. Repeated and prolonged activities can take their toll if the body doesn’t get a chance to recover. Recovery helps repair these sore and achy tissues along the way, keeping them healthy.
*Whether at work or at home, you can use these ideas to help prevent neck pain and injury. Here are some additional tips to use at work to avoid tension and keep your neck healthy:
__Be Relaxed. Try to work with your muscles relaxed. To stay relaxed, look relaxed.
__Pace Yourself. Keep an even keel. Avoid sudden changes in your workload. Try to avoid last minute “panics” to meet deadlines.
__Take a Break. Take a thirty second “microbreak” every twenty to thirty minutes to do some deep breathing and a few exercises. Take a few minutes each hour to do some exercises, get a drink, or go bug a coworker. Use your lunch break to take a nap or a walk.
__Change Positions. Avoid holding your neck, trunk, or limbs still for a long time. Plan ways to get the job done using different positions. Sit for a bit—then stand for a bit. Or simply readjust your approach to the task.
_-Rotate Duties. Rotating or sharing your tasks can be fun by offering a new work setting, while giving your body a chance to recover.
__Avoid Caffeine and Tobacco. These can heighten stress, reduce blood flow, and elevate the awareness of neck pain.
Taking Care of Your Neck
__If you’ve had neck pain once, there’s a fair chance you’ll have it in one form or another in the future. When pain comes back again and again, it is called recurrent pain. Even though you may have been treated for neck pain or problems in the past, it’s not a guarantee you won’t have pain again. The question, then, is whether you can take care of your neck if soreness does return.
–Your therapist will probably give you a thorough home program when you get done with your treatments. Some of the exercises will be helpful to keep up with as a way to keep your neck healthy over time. You may also be given ways to help control pain or symptoms if they don’t go completely away, or if they return in the future. Although there are many good “home remedies”, you will want to visit your family doctor if these symptoms appear:
Pain with no apparent injury that doesn’t go away within a week to 10 days
Pain that doesn’t ease or change with the movement
Pain that actually wakes you up at night
Pain that shoots from your neck down into your arm when you cough or sneeze
“Visceral” symptoms of nausea, diarrhea, dizziness, blurred vision, ringing in the ears, etc.
Numbness, tingling, or weakness in your arms or legs
If you feel achiness or pain that is not associated with the red flags listed above, here are some home treatment ideas you may be given to ease your symptoms:
1)Rest:- When neck pain strikes, don’t do activities that make your pain worse. Remember the benefits of rest (see above).
2)Ice:- For the first two to three days, you may get help by applying a homemade cold pack. Simply place two parts crushed ice in a plastic bag with one part rubbing alcohol. This lets you reuse the bag without having it freeze solid between uses. When you’re ready to use the cold pack, wrap it in a wet washcloth. Then place it on the sore area for up to fifteen minutes a few times a day.
3)Contrast:- On day three, you may find more relief by using a “contrast” of ice and heat. This is where you begin by placing a cold pack on the sore area for 10 minutes. Then place a heating pad on for another 10 minutes. You can repeat the process a couple times, finishing with the heat.
4)Heat:- Once the acute symptoms are controlled (two to three days), you may get good relief using a heating pad. Remember to turn off the pad before going to sleep. Check your skin regularly to make sure you are not getting too much heat.
5)Traction:- In some cases, your therapist may have found out that you get good relief with neck traction. That can be good news. There are a number of traction units that can be used at home. Some of these work by giving a traction pull as water is added to a bag.
__Others work by pumping air pressure into a neck cushion. A simple way to do traction at home is to place two tennis balls in a sock. Lay down with the sock sideways just below the back of your head. The two tennis balls will give gentle traction, and the pressure of the balls can help relieve headaches, neck pain, and upper back discomfort.
6)TENS:- This stands for transcutaneous electrical nerve stimulation. If you’ve been treated in the clinic with electrical stimulation, your therapist will have a good idea if this kind of treatment helps you. If so, there are small, pocket-sized electrical stimulation units that can be used up to 24 hours a day if needed to keep pain at bay. Your therapist may choose to issue one of these, but only if you can’t get good pain relief in other ways. Also, a prescription from your doctor is required for you to use one on your own.
7)Exercise:- Some exercises are designed to help take the pain away. After you have completed your physical therapy visits, your therapist will have gotten a good idea of what types of exercise help you control your pain. Your therapist will go over the exercises that will give you the best relief if you get sore again. Remember to only do the exercises in the way your therapist has instructed. Overdoing them could make your pain worsen.
Long-term strategies:
__The best way to treat neck pain is to avoid it altogether. A good exercise regimen can help. Also, remember the benefits of good posture, ergonomics, and work habits—and use them. If you are trying to take care of your neck but you’re not getting adequate relief, you may need to revisit your physical therapist for additional help.
Home program:
__Once your pain is controlled, your range of motion is improved, and your strength is returning, you will be progressed to a final home program. Your therapist will review some of the ideas listed above to help take care of any more soreness at home. You’ll be given some ways to keep working on the range of motion and strength too. Before you are done with therapy, more measurements will be taken to see how well you’re doing now compared to when you first started in therapy.
Post-surgical Rehabilitation :
__Some patients leave the hospital shortly after surgery. Other surgeries require patients to stay in the hospital for a few days. Physiotherapists routinely see patients for treatment in their hospital room after surgery. Therapy sessions are designed to help patients learn to move and to begin doing routine activities without putting extra strain on the neck.
__During recovery from surgery, you may have to be placed in a halo vest or rigid neck brace. These braces are used to restrict motion in the neck to allow the fusion to heal. Patients generally need to be extremely cautious about overdoing activities in the first few weeks and months after surgery.
__Most patients spend some time rehabilitating at home. Bone fusion may take several months. When the health care providers are absolutely certain that the bones have fused together, patients are able to discontinue using the neck brace or halo vest.
___As our physiotherapy sessions come to an end, we may help you with decisions about getting back to work. Ideally, patients are able to go back to their previous activities. However, some patients may need to modify their activities to avoid future problems.




One Comment