Arthritis mutilans
Table of Contents
What is Arthritis mutilans?
Arthritis mutilans is also known as pencil-in-cup disfigurement, arthritis mutilans is the most severe form of psoriatic arthritis. Arthritis mutilans takes place in five percent of cases with psoriatic arthritis & affects fingers & toes.
Arthritis mutilans is a rare disease including serious inflammation hurting the joints of the hands & foot, & leads to joint distortion with difficulties in moving the affected limbs; it can same way affect the spine. As an uncommon arthropathy, arthritis mutilans was first explained as affecting the hands, bases, fingers, & toes, but can relate in general to severe derangement of any usual damage by arthropathy. First noticed in ultramodern medical literature by Marie & Leri in 1913, in the hands, habitual absorptive arthritis. occasionally there’s foot involvement in which toes abbreviate & on which painful calluses occur in a condition known as opera glass foot or pied en lorgnette.
The condition damages & destroys joints and bones. typically, bone cells break down & rebuild. But when patients have arthritis mutilans, the bones don’t rebuild. rather, the soft tissues of the bones collapse.
Still, fingers, & toes will come shorter because of bone degeneration, If the patient has this condition. You might also develop ankylosis, which means the bones will fuse together.
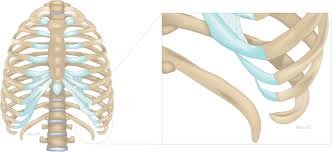
Arthritis mutilans can impact the fritters, hands, wrists, & feet. The condition is occasionally called “ opera glass hand ” or “ telescoping finger. ” Since the joints & bones are so damaged, when pulling on the affected fingers, it looks like the room of opera glasses. Telescoping fingers relate to when the bones dissolve & the soft tissues can’t hold the fingers up. So the fritters end up appearing like a telescope.
What are the symptoms of Arthritis mutilans?
When a patient develops arthritis mutilans, they experience severe inflammation. That leads to the deterioration of joints & bone tissues in the feet & hands. It’s hard to bend, move, or straighten the affected joints. The affected joints will shorten over time, which also causes the development of loose skin in the affected parts. “Fingers are very thin by the nail & then thick and fat toward the hand”. The second joint of the affected finger has been totally demolished.
Another outcome of arthritis mutilans is that bones will fuse together, which is known as ankyloses. That causes immobility & stiffness of the joint.
Other symptoms of arthritis mutilans involve stretched, shiny, & wrinkled finger skin. the patient might have stiffness and won’t be able to completely make a fist or move their fingers well.
- Severe joint pain & swelling in hands and feet
- Bones in your hands & feet fuse and disappear
- Skin lesions, which generally appear before arthritis develops
- Nail changes, like thickening & lifting from the nail bed (subungual hyperkeratosis) & discoloration (oil drop sign)
- Over time, the patient might get an “opera glass hand,” which means your fingers can be pulled in & out like opera glasses because of unstable joints and bones
If a patient develops psoriatic arthritis mutilans, the bone in the affected joints will begin to disappear. This can result in symptoms that might include:
- inability to straighten or bend the involved joint
- shortened limb- joints
- loose skin in affected joints
- Over time, as the affected joints shorten, loose skin might develop in the affected areas. The loose skin can retract & becomes loose and mobile.
Arthritis mutilans can hinder daily activities like dressing & cooking. A study in the Scandinavian Journal of Rheumatology of 67 patients with arthritis mutilans found that 42 % had retired early or were on sick leave. 21 % of patients reported little or no ability to perform self-care or everyday tasks.
What are the causes of Arthritis mutilans?
There are five forms of psoriatic arthritis, & psoriatic arthritis mutilans is considered the most severe. To understand how the disease develops, it’s helpful to understand how psoriatic arthritis occurs.
Patients usually develop psoriatic arthritis if they’ve already had psoriasis. Psoriasis is caused by an autoimmune response in the body, where the immune system attacks healthy cells. This can lead to inflammation throughout the body, including the joints. It’s the major cause of arthritis.
Long-term inflammation of joints can cause permanent damage. Certain bones, like those connected to frequently used joints, might start to erode. When this takes place, it’s known as psoriatic arthritis mutilans.
Arthritis mutilans can be triggered or caused by:
- physical trauma to the joint in a patient with psoriatic arthritis
- other environmental triggers
- genetics, which might play a roleTrusted Source in the development of psoriatic arthritis
- People can develop bone loss in one or more trusted Source joints.
Rare causes
While arthritis mutilans typically arise as a progression of RA or PsA, its symptoms can also develop in patients with other conditions.
Reports have described arthritis mutilans symptoms in patients with juvenile idiopathic arthritis, multicentric reticulohistiocytosis, & systemic lupus erythematosus, for example.
Nevertheless, cases of arthritis mutilans in patients with these conditions are frequently isolated, & in many instancesTrusted Source, they are not contemporary.
What are the risk factors of Arthritis mutilans?
Psoriatic arthritis mutilans is rare, so there’s small evidence on how to predict whether it will develop.
So far, research from trusted sources into the risk factors for psoriatic arthritis is inconclusive. Childhood obesity & diagnosis of
psoriasis at a young age might be a risk factors. But the only strong indicator of developing psoriatic arthritis is a family history of the condition.
Potential risk factors for psoriatic arthritis can involve:
- genetics
- family history
- history of infection requiring antibiotics
- skin trauma
- joint trauma
How to prevent Arthritis mutilans?
Conditions which are difficult to predict can be hard to prevent. There is recently no way to prevent psoriatic arthritis.
finding psoriatic arthritis early & seeking treatment can help prevent & slow down bone damage.
If the patient finds out they have a family history of psoriasis, talk with a doctor. If a patient experience symptoms of arthritis, especially If they have psoriasis, talk with a doctor.
What is the diagnostic procedure for Arthritis mutilans?
Arthritis mutilans are diagnosed first by confirming that the patient has arthritis & what kind of arthritis you have. the rheumatologist will check your joints for signs of swelling or tenderness. the rheumatologist will do bloodwork to help understand what kind of arthritis patients have. “History & physical exam are the main keys to a diagnosis”.
X-rays are then utilized to help physicians see exactly what’s happening with the joints & whether your joint damage could be arthritis mutilans.
Doctors currently utilize the Classification Criteria for Psoriatic Arthritis (CASPAR) to evaluate psoriatic arthritis. Even though psoriatic arthritis is a distinct disease, it’s underdiagnosed because of its wide range of symptoms. It’s estimated that more than half of patients with the condition are undiagnosed.
To be diagnosed with arthritis mutilans, the patient must have inflammatory arthritis in their:
- Joints
- Spine
- The connective tissue between bone & ligaments or tendons (enthesis)
- A rheumatologist or dermatologist will determine whether the patient has arthritis mutilans by asking you the following questions. the patient will be diagnosed with the disease if you have three or more points from the categories below:
- Evidence that the patient currently has psoriasis (2 points)
- Evidence that the patient has a history of psoriasis or a family history of psoriasis (1 point)
- Nail conditions typical of psoriasis, such as thickening of the skin beneath nails (hyperkeratosis), or detached nails (onycholysis) (1 point)
- Negative test result for rheumatoid factor utilizing any method other than latex (1 point)
- Current swelling of the whole toe or finger or a history of dactylitis (1 point)
- X-ray results showing new bone growth near a joint (1 point)
The patient has moderate or severe arthritis mutilans if you have:
At least three painful & swollen joints for more than six months
Psoriatic skin lesions
A history of psoriasis
To diagnose the condition, the doctor will first confirm that the patient has arthritis. After checking their joints for signs of swelling or tenderness, they’ll likely conduct diagnostic testing.
The doctor might order lab tests to find inflammation. The doctor will also likely advocate an X-ray or other imaging test to assess joint damage.
Once the doctor has diagnosed the patient with arthritis, they’ll test a blood sample to find out what kind of arthritis they have. For example, if the rheumatoid factor (RF) & cyclic citrullinated peptide (CCP) antibodies are in your blood, you might have rheumatoid arthritis (RA).
At this time, there is no lab biomarker for psoriatic arthritis or the psoriatic arthritis mutilans subset. Psoriatic arthritis mutilans is diagnosed by finding the severity of the bone damage. There are very few conditions related to such severe bone loss.
Patients with this condition might have certain features that can include:
- telescoping of one bone into another
- shortened digits
- pencil-in-cup deformity, where the bone appears sharp on an X-ray & the connecting bone has a cup shape
- osteolysis, a condition in which bone tissue degrades & becomes softer
- other nearby joints might be affected, like the small joints of the hands
Magnetic resonance imaging (MRI) is far better at imaging soft tissues & is useful in measuring cartilage loss and the formation of pannus.
Blood work can help confirm the underlying cause, measure inflammation, & evaluate disease progression. Results can help direct appropriate medical treatment & monitor the patient’s responses to it.
In addition, assessing which underlying illness has led to the disease is crucial in developing a treatment plan.
What is the treatment plan for Arthritis mutilans?
Arthritis mutilans worsen over time. Receiving early, aggressive treatment can help delay or prevent further damage.
The aim of treating are:
- Alleviate pain
- Preserve joint structure
- Prevent bone deterioration
- Improve your ability to move your hands & feet
- Patients with arthritis mutilans should also be given psychological counseling & physiotherapy treatment.
Medical treatment:
Non-steroidal anti-inflammatory drugs. Doctors will significantly prescribe non-steroidal anti-inflammatory drugs (NSAIDs) to treat milder forms of arthritis mutilans.
Disease-modifying antirheumatic drugs. These drugs, known as DMARDs, involve methotrexate, cyclosporine, leflunomide, & others.
A weekly dose of methotrexate is generally effective in treating your pencil-in-cup deformity, but treatment depends on the the severity of your condition & your medical history. Nevertheless, methotrexate might cause liver damage if used with NSAIDs.
Cyclosporine is another common drug utilized to treat arthritis mutilans. It’s much more effective when utilized with adalimumab, an anti-tumor necrosis factor agent.
Anti-tumor necrosis factor agents. This form of treatment is for patients with moderate to severe arthritis mutilans who have an intolerance to NSAIDs or DMARDs for more than 3 months.
TNF is a protein in the body accountable for inflammation. According to the American College of Rheumatology, TNF inhibitors can help decrease inflammation & keep the disease from getting worse. Suppressing inflammation retains joints from feeling stiff or painful. Reducing inflammation might also help restore joint function.
A 2017 review trusted Source suggests that switching between anti-TNF medications in the event that one becomes less effective might be an effective treatment strategy.
Surgical treatment:
This is the least usual form of treatment for arthritis mutilans.
For severe cases, a doctor might recommend surgery to repair bone & tissue damage caused by arthritis mutilans. For example, a patient might benefit from bone graft procedures or surgical joint fusing. Nevertheless, because of the rareness of this disease, establishing the effectiveness of these procedures will need more evidence.
Although a 2011 research article stated that disagreements between hand surgeons & rheumatologists remain regarding the indications, timing & effectiveness of rheumatoid hand surgery, arthritis mutilans might be successfully treated by iliac-bone graft & arthrodesis of the interphalangeal joints & the metacarpophalangeal joint in each finger.
Physiotherapy treatment:
Physical therapy can play a major role in improving the life of a patient with mutilans arthritis.
The physical therapist should target patient awareness, patient education, regaining range of motion, strengthening of hand muscles & general cardiovascular conditioning. Therapists may also apply ultraviolet therapy & other modalities to alleviate pain. Cryotherapy might help to reduce swelling and tenderness in affected joints. Heat might be utilized to relieve joint pain. Paraffin baths contribute be soothing for the hands.
A routine physiotherapy program can alleviate pain & regain muscle strength, physical function, & quality of life for a patient with mutilans arthritis. Splinting might be beneficial to prohibit deformity.
Recent studies have shown that hydrotherapy is also an effective technique for patients with psoriatic arthritis. Hydrotherapy has been revealed to regain physical function, sleep & cognitive function, relaxation, work, & also participation in patients with this condition.
Summary
Arthritis mutilans is a rare form of advanced joint disease, & it is most usual in patients with PsA & RA. It is a progressive condition & worsens if a patient does not receive effective treatment.
This type of arthritis can cause permanent disability if it is not treated. But an evaluation of psoriatic arthritis mutilans means something different now than in the past when it was called “opera glass hand.”
A range of physical therapies, medications, & in severe cases, surgery, might slow the progression of the disease & improve the quality of life.
patient’s outlook can improve dramatically when you detect & treat psoriatic arthritis. Early treatment can prevent bone loss.
Bone tissue can not be fully restored. But treating psoriatic arthritis can slow the damage to bones. Instead of losing the usage of fingers or toes, treating them can help remain them functioning.
If a patient does not receive effective treatment, arthritis mutilans can lead to severe bone destruction & loss of movement. It can also change the shape of the involved joints.
Arthritis mutilans’ parent condition psoriatic arthritis leaves patients with a mortality risk 60% higher than the general population, with premature death causes mirroring those of the general population, cardiovascular issues being the most common. Life expectancy for patients with psoriatic arthritis is estimated to be decreased by approximately 3 years.
FAQ (frequently asked questions)
Because of the more effective treatment of psoriatic arthritis, arthritis mutilans rarely develop, so it is not that common.
Arthritis mutilans is explained as the most severe form of psoriatic arthritis. It is characterized by digital shortening related to severe osteolysis of peripheral joints.
Psoriatic arthritis is divided into five forms: distal interphalangeal predominant, symmetric polyarthritis, spondylitis, asymmetric oligoarticular & arthritis mutilans.
The index and middle fingers & the thumb are the areas of the hand most usually involved. Many patients find that the hand they use most is affected more than the other. When the fingers are affected, it might be in the joints closest to the fingernails or the ones in the middle of the fingers.
Scientific research has revealed that a routine hand massage might help ease pain, improve hand strength, & decrease feelings of stress & anxiety. Massage can accomplish treatments for carpal tunnel syndrome, arthritis, neuropathy, & other diseases.