Ophthalmoplegia
Table of Contents
What is Ophthalmoplegia?
Ophthalmoplegia is a condition when the eye muscles are weak or paralyzed. It can impact either one or more than six muscles that control the movement of the eye and holds it in place.
Ophthalmoplegia is usually of two types: Internal and Chronic progressive external ophthalmoplegia are the two main kinds of ophthalmoplegia. Internal or internuclear ophthalmoplegia occurs when there is an injury to the nerve fibers which control lateral eye movement. This can lead to double vision. In contrast, drooping eyelids are a symptom of chronic progressive external ophthalmoplegia, which causes problems controlling the ocular muscles that control eye movement.
Ophthalmoplegia generally involves the third (oculomotor nerve), fourth (trochlear), or sixth (abducens nerve) cranial nerves. Double vision is the usual symptom in all three cases. In oculomotor paralysis, the muscles holding the eye are affected in such a way that the eye drifts outward and slightly downward and has problems turning inward and upward. In addition, the upper eyelid of the impacted eye usually droops, a condition named ptosis, and the pupil may be enlarged. If the pupil is abnormally big, the chance of a cerebral aneurysm arises. This can be associated with pain.
The treatment for ophthalmoplegia is typically based upon the underlying causes, symptoms, and type. When drooping eyelids are the primary cause of ophthalmoplegia, the doctor may suggest a surgery called a silicone sling. This approach helps to elevate a drooping eyelid. Ptosis, an eye disease, can also be treated with a silicone sling treatment. When the signs of sagging eyelids are not too severe, lid crutches or sticky tape can also be applied.
Types of Ophthalmoplegia:
Chronic progressive external ophthalmoplegia
The onset of chronic progressive external ophthalmoplegia in adults normally ensues between the ages of 18 and 40. Eyelids that droop and trouble coordinating the muscles that coordinate the eyes are typical early symptoms.
Progressive external ophthalmoplegia is a condition represented by the weakness of the eye muscles. Seen between the ages of 18 and 40 in adults, and it gradually gets worse over time. Ptosis, which can affect one or both eyelids, is often the initial sign of increasing external ophthalmoplegia. Ptosis sufferers may try to lift their eyelids with their forehead muscles as the condition worsens, or they may lift their chin to look up. Affected people have to turn their heads to see in diverse directions, specifically as the ophthalmoplegia exacerbates. In addition, to overall muscle weakness (myopathy), those with increasing external ophthalmoplegia may also experience weakness in their neck, arms, or legs. Exercise intolerance may make the weakness more noticeable during physical activity. Dysphagia, or trouble swallowing, can also result from muscle weakness.
Although muscle weakness is the first symptom of progressive external ophthalmoplegia.
Internuclear ophthalmoplegia
Injury to the nerve fibres that control lateral eye movement causes internuclear ophthalmoplegia. This leads to double vision. There are various other disorders that this syndrome is linked to.
Ocular movement disorder known as internuclear ophthalmoplegia is brought on by a medial longitudinal fasciculus injury. It is indicated by impaired adduction of the ipsilateral eye with nystagmus of the abducting eye. Internuclear ophthalmoplegia was first documented in 1903, despite the fact that the medial longitudinal fasciculus was previously identified in the 1870s.
Etiology:
A lesion of the medial longitudinal fasciculus (MLF), a fibre tract responsible for carrying information required for the coordination of various eye movements, causes the condition known as internuclear ophthalmoplegia. The cerebral aqueduct in the midbrain and the fourth ventricle in the pons and medulla are both reached by this paired white matter tract, which passes through the brainstem and lies ventral to the midline. It connects all of the ocular motor nuclei and serves as the last common conduit for various conjugate eye movements such as saccades, smooth pursuit, and vestibulocochlear reflex.
Causes of Ophthalmoplegia:
The brain and central nervous system can be impacted by a number of diseases, illnesses, or traumas, which can result in weakening and paralysis in the external or internal eye muscles. Some of them are more typical, while others are incredibly uncommon.
This condition can be congenital means present at birth; acquired means appearing later in life. The messages that are transmitted from the brain to the eyes are typically disrupted, which is the main cause.
Multiple sclerosis, trauma, or infarction are frequently the causes of internuclear ophthalmoplegia.
Graves disease, Kearns-Sayre syndrome, or other mitochondrial diseases are frequently to blame for external ophthalmoplegia.
Other common causes include:
- Migraines
- Thyroid disease
- Stroke
- Brain injury
- Brain tumor
- Infection
- Congenital conditions (being born with ophthalmoplegia
- Gene mutations
- Head injury
- Diabetes
- Infections that affect the central nervous system
- Multiple sclerosis (MS)
- Rare diseases such as Tolosa Hunt Syndrome
Ophthalmoplegia is a rare result of a head injury or a rare illness. On the other hand, the disorder is considerably more likely to be brought on by multiple sclerosis or a stroke.
The classification may be based on the source of the ophthalmoplegia or the movement patterns that are affected.
Ophthalmoplegia may result from a variety of illnesses or deficiencies in any organ system, including the following:
- Globe
- Muscle dysfunction: Graves disease, Kearns-Sayre syndrome, and progressive external ophthalmoplegia
- Neuromuscular junction: Myasthenia gravis
- Cranial nerves: Cavernous sinus syndrome and increased intracranial pressure (ICP) affect the cranial nerves.
- Brainstem nuclei: Brainstem stroke, e.g., Foville syndrome
- White matter tracts: internuclear ophthalmoplegia
- Dorsal midbrain: Parinaud syndrome
- Cerebral cortex: Stroke
- Toxin: Venom
- Deficiency: Thiamine deficiency in Wernicke encephalopathy
The cranial nerves that innervate the extraocular muscles and are responsible for eye movement include:
The oculomotor nerve (CN III): Innervates the striated part of the levator palpebrae superioris muscle, the inferior rectus muscle, the superior rectus muscle, the inferior oblique muscle, the pupilloconstrictor muscle, and the medial rectus muscle.
Trochlear nerve (CN IV): The superior oblique muscle is innervated.
Abducens nerve (CN VI): The lateral rectus muscle is innervated.
Causes of Internuclear Ophthalmoplegia
Internuclear ophthalmoplegia is caused by injury to the interneuron that lies between two particular cranial nerve nuclei. This may arise as a result of lesions forming in the medial longitudinal fasciculus (MLF), which typically happens in young people who have multiple sclerosis or in older persons due to stroke.
Other possible causes, which are less frequent, can be as follows:
- Brain tumour
- Lyme disease
- Head trauma
- Nutritional disorders
- Drug use
- Neurosyphilis
- Arnold-Chiari malformation (an uncommon skull deformity)
Risk factor:
People with diabetes are slightly more likely to develop ophthalmoplegia. Recently, it was shown that men with type 2 diabetes who are older than 45 and have had it for more than 10 years are at a higher risk of getting ophthalmoplegia.
More susceptible than others are those who suffer from a disorder like multiple sclerosis or Graves’ disease that impairs their ability to control their muscles. There are generally no lifestyle choices that increase one’s risk of developing ophthalmoplegia. But maintaining a balanced lifestyle will lower your risk of stroke and associated vision issues by preserving a healthy vascular system.
A stroke or a cerebrovascular event, such as multiple sclerosis, causes this syndrome in about 70% of patients.
- Risk factors for multiple sclerosis are given below:
- Age: 20 to 50
- Being a cisgender woman, perhaps because of hormonal variations
- Having northern European ancestry and being Caucasian, with some research also suggesting that African American women face a similar risk
- Risk factors for Cerebrovascular Accidents (CVA) include the following:
- Elderly person (70+ years old)
- Hypertension
- Diabetes
- Smoking.
Keep in mind that both of these conditions can affect people outside their primary risk groups. Even if one of the disorders listed above is present, ophthalmoplegia may not inevitably result.
Signs and symptoms of Ophthalmoplegia:
Depending on the type you have (for example, internal or external), the underlying reason, and the particular eye muscles involved, this ailment might have a variety of symptoms.
Signs and symptoms may include the following:
- Blurry vision
- Strabismus (misalignment of one or both eyes)
- Diplopia (double vision)
- Difficulty moving one or both eyes in a certain way
- Difficulty swallowing
- Ptosis (droopy eyelids)
- General muscle weakness
It’s essential to remember that ophthalmoplegia is not the only eye disease that can cause these symptoms. To determine the cause of these or other eye illnesses an eye doctor might perform an eye exam and tests.
Ophthalmoplegia often falls into one of two categories and can range in severity.
- Internuclear ophthalmoplegia (INO). The eyes can’t always function together when someone has this medical condition. An ipsilesional adduction deficiency, where one eye lags the other and frequently has a limited range of motion, is what distinguishes it.
- Progressive external ophthalmoplegia
Symptoms of Internuclear Ophthalmoplegia
Internuclear ophthalmoplegia can cause the following symptoms:
- Double vision
- Difficulty tracking fast objects
- Dizziness
- Progressive external ophthalmoplegia is superficially similar. The ocular muscles are impacted by this disorder. Symptoms can include the following:
- Droopy eyelids
- Difficulty moving the eyes
- Muscle weakness in other areas, involving the neck, arms, legs, and throat
Symptoms of INO may vary in severity. The symptoms can include:
- Horizontal diplopia: The restriction of adduction in the ipsilateral eye results in horizontal diplopia. Diplopia is typically not noticeable in the primary gaze and is more obvious when staring at items on the opposite side of the lesion.
- Trouble tracking fast-moving objects, or vertigo on lateral gaze.
- Headaches or other impairments: Due to the involvement of the brainstem
- Vertical oblique diplopia related to the associated skew deviation may also be another symptom.
- Reading fatigue, visual disorientation, stereopsis loss, oscillopsia, and diplopia can all come from the interruption of binocular vision that results from improper conjugate horizontal eye movements.
- The difficulty in looking at the sides may lead to difficulties while driving or walking and may increase the risk of road traffic accidents or falls.
- Vertigo and headaches are common complaints among patients.
Signs:
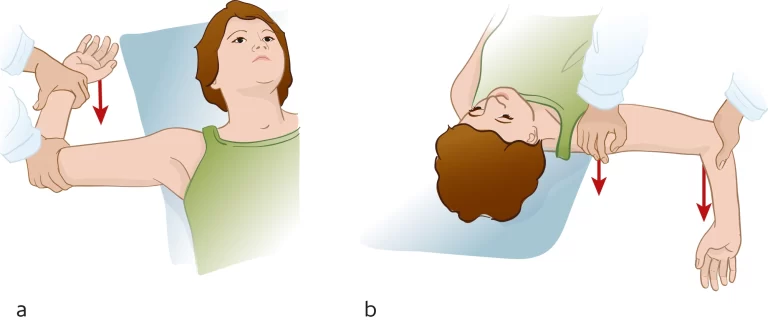
A good ocular examination is often all that is needed to diagnose INO. The INO is characterized clinically by an ipsilesional adduction deficit (partial or complete) with a contralateral, dissociated, horizontal abducting saccade or nystagmus on attempted gaze to the contralesional side. There is a slow adducting saccadic velocity on the affected side. A skew deviation in the ipsilateral hypertrophic eye may be noted. On upgaze, vertical gaze nystagmus may be seen. The INO may be unilateral, bilateral, or neurologically isolated and present with or without other brainstem abnormalities.
Symptoms of External ophthalmoplegia
Less frequently seen with increasing external ophthalmoplegia are the following signs and symptoms:
- Muscle weakness is the primary symptom.
- Hearing loss due to nerve damage in the inner ear (sensorineural hearing loss)Limb numbness
- Weakness and loss of sensation in the extremity (neuropathy) due to damage to the nerve
- Impaired muscle coordination (ataxia)
- Parkinsonism (abnormal movement patterns frequently linked to Parkinson’s disease)
- Depression
- Progressive external ophthalmoplegia is a disorder that develops with time and often manifests between the ages of 18 and 40.
There may be more symptoms and indications that go along with this illness. The illness is known as “progressive external ophthalmoplegia plus” (PEO+) in certain situations.
The hereditary disorder known as progressive external ophthalmoplegia is uncommon. It is a serious condition, and more study is required to understand its causes and how to aid those who are affected.
Diagnosis:
Eye movements can be seen during a physical examination to identify ophthalmoplegia. The eye may then be examined more thoroughly using an MRI or CT scan.
Blood tests may be required to determine whether it’s caused by another condition, such as thyroid disease. A person may be referred to an eye specialist or neurologist for these tests.
Internuclear ophthalmoplegia (INO) is diagnosed as:
INO is identified through a physical examination by a physician. They’ll look into their eyes and watch how they move. A person will be asked to do motions that will demonstrate whether one eye isn’t turning properly.
In particular, if you have had a stroke or been in a serious accident, it might also be discovered through tests for other illnesses.
What tests are done to diagnose internuclear ophthalmoplegia?
A doctor might require one of a few imaging tests to confirm damage to the medial longitudinal fasciculus, including:
- MRI (magnetic resonance imaging).
- A CT (computed tomography) scan.
A doctor may also suggest other tests if imaging tests aren’t helpful. These may include:
- Blood tests: These can show signs of infection or other issues that might affect the brain.
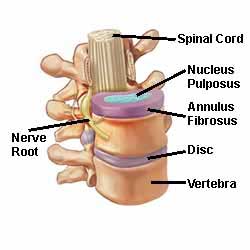
- Spinal tap (lumbar puncture): This procedure draws the cerebrospinal fluid from your back and examines it for signs of potential causes, particularly infections.
Treatment of Ophthalmoplegia:
The etiology of ophthalmoplegia will determine the optimal course of treatment.
Depending on the patient’s age, the type of ophthalmoplegia, symptoms, and the underlying cause of ophthalmoplegia, the treatment and therapy for ophthalmoplegia might differ significantly.
Children with this disorder are born typically learn compensatory skills and may not even be aware of their vision issues. Adults who experience double vision may be fitted for special glasses or advised to wear an eye patch in order to restore normal vision.
Double vision caused by ophthalmoplegia in children or adults may be treated with an eye patch or with special glasses. Some patients may choose to wear glasses with “stilts” that can support sagging eyelids.
Ptosis surgery or strabismus surgery are two examples of operations that certain individuals may benefit from in order solve a specific problem.
Treatment for the underlying problem may occasionally assist to lessen ophthalmoplegia symptoms.
Treatment for internuclear ophthalmoplegia (INO):
The cause of INO will determine the treatment method. Instead of treating the INO directly, a clinician will address the underlying cause
Some INO-related conditions, such as multiple sclerosis and strokes, demand ongoing care—possibly for the rest of one’s life.
Infections can result in internuclear ophthalmoplegia, which often improves once the infection is treated.
If the symptoms are persistent (last a long time), a doctor might inject botulinum toxin to relax muscles around the eyes. This can help reduce double vision (diplopia) and decrease uncontrolled eye movements (nystagmus).
A doctor will tell a patient which treatments they need and what to expect.
Treating migraines can help people with ophthalmoplegia have better outcomes.
Treatment for Chronic Progressive External Ophthalmoplegia:
Chronic progressive external ophthalmoplegia develops with drooping eyelids and directs to problem controlling the eye muscles which coordinates eye movement.
The goal of treating ophthalmoplegia is, whenever possible, to treat any underlying diseases. Isolated nerve palsies frequently go away on their own with time, and the only real therapy is to patch the affected eye to prevent any temporary double vision. People with chronic ophthalmoplegia may benefit from prism-equipped eyeglasses or surgical treatment.
The underlying causes, symptoms, and kind of ophthalmoplegia will largely determine the course of treatment. Ophthalmoplegia frequently comes on by drooping eyelids, and in these circumstances, a silicone sling technique may be advised by the ophthalmologist. A drooping eyelid can be raised with this treatment. Ptosis, an eye disease, can also be treated with a silicone sling treatment. When the signs of a sagging eyelid are not too severe, lid crutches or adhesive tape can also be applied.
How is the treatment done?
A Seiff silicone suspension must be used in silicone sling procedures. The silicone is inserted into the muscle through a stab incision. This procedure is highly popular and efficient because it includes early recovery, minimal oedema (minimum postoperative scars), no multiple incisions, and less surgical time. For individuals with impaired levator functions brought on by ophthalmoplegia, this technique is excellent. Compared to traditional sling techniques, it offers additional benefits.
Prevention
This condition is rare enough that active prevention efforts likely aren’t important for most people. However, leading a healthy, secure lifestyle can significantly lower the risk of developing ophthalmoplegia as well as other illnesses at the same time.
Eating a good diet, avoiding smoking or quitting if a person already smokes, and making sure to monitor yourself closely if you have diabetes can all help reduce the risk of vascular health issues.
Protecting the brain by wearing the appropriate protective gear and avoiding unnecessary risks can further help to reduce the risk of trauma, which is best avoided for many reasons.
Summary:
Although internuclear ophthalmoplegia may only be a short-term problem, some symptoms may last for the remainder of your life. It depends on what caused it initially. Long-lasting internuclear ophthalmoplegia can also be brought on by conditions like multiple sclerosis and some autoimmune illnesses.
When an infection is treated, people who have internuclear ophthalmoplegia normally recover and experience no long-term complications.
A person is more likely to have long-term symptoms if they have experienced a stroke, hemorrhage, or traumatic brain injury, or if they have multiple sclerosis. How the eyes and vision recover will depend on how long the blood supply to the brain and nerves is interrupted.
Talk to the doctor about what to expect and how you can manage the symptoms.
FAQs:
Can ophthalmoplegia cause blindness?
The unusual but horrible and deadly consequence of blindness with ophthalmoplegia and ptosis is extremely common. The patient’s social life is typically significantly impacted by the damaged appearance.
Can a stroke cause ophthalmoplegia?
A mild acute ischemic stroke involving the MLF can cause isolated unilateral internuclear ophthalmoplegia, which is a rather uncommon condition.
Does ophthalmoplegia cause pain?
A pathological condition called painful ophthalmoplegia is brought on by the cavernous sinus being inflamed in an unspecific way because of a tumor, vasculitis, basal meningitis, neurosarcoidosis, or diabetes. It includes periorbital or hemicranial discomfort, as well as other cranial nerve palsies and ipsilateral ocular motor nerve palsy.
Which vitamin causes ophthalmoplegia?
Wernicke Encephalopathy (WE), which is traditionally defined as a triad of encephalopathy, ophthalmoplegia, or nystagmus, and gait ataxia, is particularly dangerous for thiamine deficiency.
What nerve is affected in ophthalmoplegia?
INO, also known as internuclear ophthalmoplegia or ophthalmoparesis, is an eye movement condition that manifests as ophthalmoplegia and the inability to perform conjugate lateral gaze due to interneuron injury between two cranial nerves (CN) VI and CN III (internal) nuclei.




One Comment