The Lumbar Plexus
Table of Contents
What is lumbar plexus?
The lumbar plexus is a vital collection of nerves that arise from mostly the lumbar medulla spinalis. The term plexus refers to a “web” of nerves that’s created just lateral to where T12-L5 exit the neural structure via intervertebral foramina. The plexus exists bilaterally and allows nerves to mix with different levels to make multiple functioning nerves that serve to innervate various structures. this kind of nerve web is critical for the formation of larger, longer nerves that concentrate on peripheral tissues that altogether primarily help to innervate the portions of the lower extremities. the first functions of those nerves are motor innervation and sensory nerves to the skin mainly within the lower extremities, although the superior nerves within the plexus do contribute to the lower abdomen and pelvis. The nerves arising from the lumbar plexus are vital for the functioning of the lower extremity and maintaining the flexibility to increase the knee, flex the hip, adduct the thigh, and more.
Origin and Location
The origin of the lumbar plexus is within the psoas major muscle, anterior to the lumbar towards the transverse processes. The dorsolumbar nerve, which joins the anterior ramus of nervus L1, contributes to the creation of the lumbar plexus via the anterior ramus of nervus spinalis T12. The iliohypogastric and ilioinguinal nerves are derived from one trunk formed by these roots (T12, L1). The anterior rami of L1 and L2 each have a branch that unites to create the genitofemoral nerve.
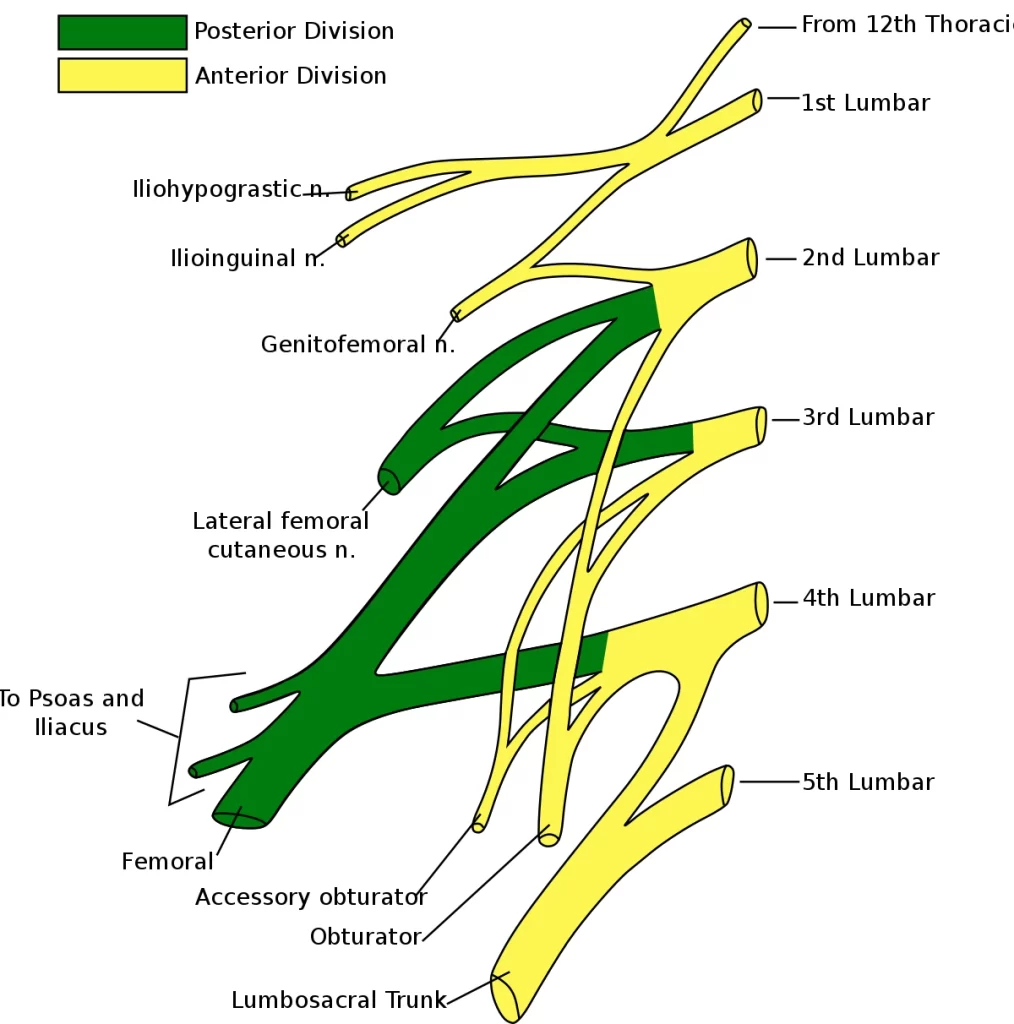
Branches of Lumbar plexus
The iliohypogastric nerve travels posterior to the psoas major on its proximal lateral border to travel laterally and obliquely on the anterior side of the quadratus lumborum. Lateral to the present muscle, it pierces the abdominal to run above the iliac crest between that muscle and the abdominal internal oblique. It provides several motor branches to those muscles and a sensory branch to the skin of the lateral hip. Its terminal branch then travels parallel to the inguinal ligament to exit the aponeurosis of the abdominal external oblique above the external inguinal ring where it supplies the skin above the inguinal ligament (i.e. the hypogastric region) with the anterior cutaneous branch.
The ilioinguinal nerve closely follows the iliohypogastric nerve on the quadratus lumborum, then again passes below it to run at the extent of the iliac crest. It pierces the lateral wall and runs medially at the extent of the inguinal ligament where it supplies motor branches to both musculus transversus abdominis and sensory branches through the external inguinal ring to heal the pubic symphysis and also the lateral aspect of the labia or scrotum.
The genitofemoral nerve pierces the psoas major anteriorly below the previous two nerves to instantly split into two branches that run downward on the anterior side of the muscle. The lateral femoral branch is only sensory. It punctures the vascular lacuna near the saphenous hiatus and supplies the skin below the inguinal ligament (i.e. proximal, lateral aspect of the femoral triangle). The genital branch varies in males and females. In males, it runs within the funiculus, and in females within the channel along with the teres uteri ligament. It then transmits sensory branches to the scrotal skin in males and also the labium in females. In men, it supplies motor innervation to the cremaster.
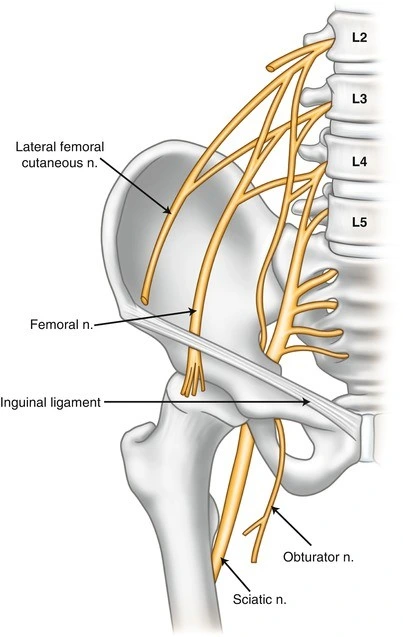
The lateral cutaneous anterior crural nerve penetrates the psoas major on its lateral side and runs obliquely downward below the iliac fascia. Medial to the anterior superior iliac spine it leaves the pelvic area via the lateral muscular lacuna it enters the thigh by passing behind the lateral end of the inguinal ligament. Within the thigh, it shortly moves under the fascia lata before it branches the fascia and supplies the skin of the anterior thigh.
The obturator nerve leaves the lumbar plexus and descends behind the psoas major on that medial side, then follows the linea terminalis into the lesser pelvis, and eventually leaves the pelvic area through the obturator canal. Within the thigh, it sends motor branches to the obturator externus before parts into an anterior and a posterior branch, both of which remain distally. These branches are separated by adductor brevis and provide all thigh adductors with motor innervation: pectineus, adductor longus, adductor brevis, adductor Magnus, adductor minimus, and gracilis. The anterior branch contributes a terminal, sensory branch which passes along the anterior border of the gracilis and supplies the skin on the medial, distal part of the thigh.
The nervus spinalis is the largest and longest of the plexus’ nerves. It provides motor innervation to the iliopsoas, pectineus, sartorius, and quadriceps femoris; and sensory innervation to the anterior thigh, posterior lower leg, and hindfoot. Within the pelvic area, it runs in a very groove between the psoas major and iliacus giving off branches to both muscles, and exits the pelvis through the medial aspect of a muscular lacuna. Within the thigh, it parts into numerous sensory and muscular branches and also the nerve, its long sensory terminal branch which continues all the way down to the foot.
Nerves
The nerves arising from the lumbar plexus from superior to inferior are iliohypogastric, ilioinguinal, genitofemoral, lateral femoral cutaneous, spinal nerve, obturator, and nerve to the lumbosacral trunk.
The iliohypogastric nerve is formed from spinal levels T12 and L1. it’s motor innervation to the inferior oblique muscle and therefore the transverse abdominal muscles. Its sensory intakes are to the lateral gluteal area.
The ilioinguinal nerve comes from a branch of the L1 nervus spinalis. It provides sensory intake to the anterior superior and medial parts of the thigh. In men, the distal portions of the nerve become the anterior scrotal nerve that inputs sensory fibers to the basis of the penis and also the superior part of the scrotum. In women, the distal portions of the nerve are the anterior labial nerves that help to supply sensory intakes to the skin covering the mons veneris and therefore the labium. It also provides some motor inputs to the inferior oblique muscle and also the transverse abdominal muscles.
The genitofemoral nerves rise from the superior aspects of L1 and L2 spinal nerves. The nerve divides into the genital and also the femoral branch. The genital branch supplies the cremaster muscle and scrotal skin in males and supplies sensory to the animal tissue and so the labium in females. The genitofemoral nerve femoral branch gives sensory innervation to the anterior, superior area of the thigh.
The lateral femoral cutaneous nerve arises from the L2 and L3 spinal nerves. It supplies the singular function of supplying sensory innervation to much of the lateral part of the thigh.
Iliohypogastric Nerve
The iliohypogastric nerve is the first major branch of the lumbar plexus. It runs to the iliac crest, across the quadratus lumborum muscle of the posterior wall. It then perforates the abdominal muscle and divides into its terminal branches.
Roots: L1 (with contributions from T12).
Motor Functions: Innervates the interior oblique and abdominal.
Sensory Functions: Innervates the posterolateral gluteal skin within the loins.
Ilioinguinal Nerve
The ilioinguinal nerve follows an identical anatomical course because of the larger iliohypogastric nerve. After innervating the muscles of the anterior wall, it passes through the superficial inguinal ring to innervate the skin of the genitalia and middle thigh.
Roots: L1.
Motor Functions: Innervates the interior oblique and transverse muscle of the abdomen.
Sensory Functions: Stimulates the skin on the superior anteromedial thigh. In males, it also supplies the heal the basis of the penis and anterior scrotum. In females, it supplies the healing fatty tissue and labium.
Genitofemoral Nerve
After leaving the psoas major muscle, the genitofemoral nerve rapidly divides into a genital branch and a femoral branch.
Roots: L1, L2.
Motor Functions: The genital branch stimulates the cremasteric muscle.
Sensory Functions: The genital branch stimulates the skin of the anterior scrotum (in males) or the heal fatty tissue and labium (in females). The femoral branch stimulates the skin on the upper anterior thigh.
Lateral Cutaneous Nerve of the Thigh
This nerve encloses a purely sensory function. It enters the thigh at the lateral aspect of the inguinal ligament, where it gives cutaneous innervation to the skin there.
Roots: L2, L3
Motor Functions: None.
Sensory Functions: Stimulates the anterior and lateral thigh all the way down to the extent of the knee.
Obturator Nerve
Roots: L2, L3, L4.
Motor Functions: Stimulates the muscles of the medial thigh – the obturator externus, adductor longus, adductor brevis, adductor Magnus, and gracilis.
Sensory Functions: Stimulates the heal the medial thigh.
Femoral Nerve
Roots: L2, L3, L4.
Motor Functions: Stimulates the muscles of the anterior thigh – the illiacus, pectineus, sartorius, and quad.
Sensory Functions: Stimulates the skin on the anterior thigh and therefore the medial leg.
Embryology
The spinal cord forms from the neural plate. Peripheral nerves derive from neuroepithelial cells. These nerves help create the neurons, support cells, and axons that contribute to the peripheral nervous system. These are important in the creation of peripheral nervous structures such as the lumbar plexus.
Morphology remains similar when comparing structures from a fetal lumbar plexus to an adult lumbar plexus. Specifically, nerve thickness, length, and spinal nerve branching are observed to remain the same throughout development.
Blood Supply and Lymphatics
Blood supply to the lumbar plexus is complex. The plexus embeds itself within the posterior aspect of the psoas major muscle. thanks to this anatomical relevancy an oversized muscle, can share its blood supply. the first blood supply of the plexus comes from the lumbar branch of the arterial blood vessel, a branch of the interior arterial blood vessel. The lumbar plexus has protection from ischemic damage because of multiple collateral arterial systems that it receives from small arteries of the psoas muscle. Therefore, ischemic injury to the current area during aortoiliac surgery is unusual.
Muscles
The lumbar plexus provides innervation to many important muscles. Notable muscles include the psoas muscle, quadratus lumborum, lumbar transverse muscles, quadriceps, musculus transversalis abdominis, and internal oblique muscles. Nerves that arise directly from the plexus are answerable for innervation to the psoas muscles, quadratus lumborum, and lumbar transverse muscles. The remains of the muscles receive stimulation from nerves that form after exiting the lumbar plexus.
The innervation supplied to the quadriceps muscle is critical for the proprioception of the hip and knee. Stimulation to the vastus lateralis, vastus intermedius, and also the vastus medialis help give proprioceptive details about the knee to the central system. Stimulation of the rectus femoris helps gives prospective details to the central nervous about the hip.
Surgical Considerations
The lumbar plexus and its derivatives are essential to think about when performing surgery. An anterior abdominal approach surgery may result in iatrogenic injury to superficial branches of either the iliohypogastric nerve, ilioinguinal nerves, or genitofemoral nerve. Injury to those during surgery may end up in paresthesias. Of these, the genitofemoral nerve is the most difficult to spot intraoperatively. Additionally, damage to the lumbar plexus could be a well-documented iatrogenic injury following a minimally invasive lateral retroperitoneal transposons approach. This injury to the lumbar plexus most ordinarily causes neuropraxia, with recovery within 3 months.
It is crucial to notice the utilization of nerve blocks to the ilioinguinal nerve, Iliohypogastric nerve, and genitofemoral nerve are considerations within the management of treatment-resistant groin pain, likewise as surgery to the present area. Ultrasound-guided erector spinal block is simpler than ultrasound-guided ilioinguinal/ iliohypogastric blocks in children requiring hernia surgery. An ilioinguinal transversus abdominal plane nerve block has produced more practical analgesia for patients undergoing an elective cesarean.
In joint surgery of either the hip or the knee may end up in proprioceptive impairment. Innervation of the musculature surrounding the joint, furthermore as innervation to the joint itself is important for proprioceptive information sent to the central system. it’s important to think about this aspect of joint when planning rehabilitation techniques for patients’ status post hip or knee arthroplasty.
Clinical Significance
Damage to the lumbar plexus or nerves proximal and distal to that may result in several pathologies. Lumbar disc herniation may end up in occlusion of the intervertebral foramen, which may compress lumbar spinal nerves proximal to their entrance to the lumbar plexus. This condition may result in paresthesia and weakness of the areas innervated by nerves of the lumbar plexus. Commonly, peripheral nerves and therefore the lumbar plexus can suffer damage thanks to trauma.
An important reflex to notice is the cremasteric reflex. The femoral portion of the genitofemoral nerve and therefore the ilioinguinal nerve provides the afferent fibers for this reflex. The genital branch of the genitofemoral nerve supplies motor innervation to the cremaster muscle and is chargeable for the efferent. because the afferent portion is the sensory aspect, stroking the medial thigh should cause contraction of the cremasteric muscle end in the ascension of the scrotum. In patients with testicular torsion, the genital branch of the genitofemoral nerve will become entrapped, and this reflex is going to be absent.
A common and significant nervous disorder syndrome can arise from the lateral femoral cutaneous nerve, which could be a branch of the lumbar plexus. This syndrome is termed meralgia paresthetica and is caused usually by entrapment of the nerve because it passes under, or through the inguinal ligament. This status can present as a painful syndrome including the anterolateral area of the thigh. Non-steroidal anti-inflammatory drugs (NSAIDs), narcotics, and anti-neuropathic pain medications may regularly treat this condition; however if the patient remains symptomatic surgical decompression is often a consideration.
Lumbosacral Plexopathy
A lumbosacral plexopathy could be a disorder affecting either the lumbar or nerve plexus of nerves. they’re rare syndromes, caused by damage to the nerve bundles.
A plexopathy is suspected if the symptoms can’t be localized to one nerve. Patients may complain of pains, numbness or weakness, and wasting of muscles.
One of the most causes of lumbosacral plexopathy is diabetic amyotrophy, also referred to as lumbosacral radioplexus autophagy. During this condition, high glucose levels damage the nerves. Idiopathic plexopathy is another leading to, being the lumbosacral corresponding to Parsonage-Turner syndrome, which affects the brachial plexus. Tumors and other local attacks can cause plexopathy because of the compression of the plexus.
Treatment depends on what’s causing the symptoms. Tumors and space-occupying lesions, ought to be removed if possible. For diabetic and idiopathic causes, treatment with high-dose corticosteroids is beneficial.
Physiotherapy implications
A common and significant nervous disorder syndrome can arise from the lateral femoral cutaneous nerve, which could be a branch of the lumbar plexus. This syndrome is termed meralgia paresthetica and is led to general entrapment of the nerve because it crosses under, or via the inguinal ligament. This condition can present as a painful syndrome including the anterolateral area of the thigh. Non-steroidal anti-inflammatory drugs (NSAIDs), narcotics, and anti-neuropathic pain medications are accustomed to treat this condition; however, if the patient continues symptomatic surgical decompression is a consideration.
Damage to the lumbar plexus or nerves proximal and distal thereto may end up in several pathologies. it’s important that physical therapists have a decent understanding of the lumbar plexus within the treatment of symptomatic patients.
Lumbar disc herniation can lead to occlusion of the intervertebral foramen, and pressure on lumbar spinal nerves near their entry to the lumbar plexus. This syndrome can lead to paresthesia and weakening within the lumbar plexus nerves’ stimulated locations.
The lateral femoral cutaneous nerve, which could be a branch of the lumbar plexus, can cause a standard and high neurological disorder condition. This can be mentioned to as meralgia paresthetica and leads to the nerve becoming trapped because it passes beneath or via the inguinal ligament.
In order to accurately determine the reason behind patients’ pain or dysfunction, first, it’s important to see which level is affected. this can assist in choosing the correct interventions which can cause better outcomes.
FAQ
What area of the body is stricken by the lumbar plexus?
Lumbar plexus: Back, abdomen, groin, thighs, knees, calves. Sacral plexus: Pelvis buttocks, genitals, thighs, calves, feet. Coccygeal plexus: a tiny low region over the coccyx (your “tailbone”)
What happens if the lumbar plexus is damaged?
Malfunction of the nerve plexus causes pain within the lower back and leg also as weakness and loss of sensation altogether or a part of a leg (such because the foot or calf). Recovery depends on the cause.
What is the function of the lumbar plexus?
The lumbar plexus allows nerves to mix at different levels to form multiple functioning nerves that serve to innervate various structures. The nerves that arise from the lumbar plexus are listed below, from superior to inferior. The iliohypogastric nerve is made from spinal levels T12 and L1.
What causes lumbar plexus pain?
The most frequent causes are high-energy trauma, sports injuries, injury, and surgery that ends up in damage to the plexus.
How lumbar plexus is formed?
The lumbar plexus is created within the psoas major muscle from the ventral rami of the primary four lumbar nerves and a contribution of the last spinal nerve (T12).




2 Comments