Limb-Girdle Muscular Dystrophy (LGMD)
Table of Contents
What is Limb-Girdle Muscular Dystrophy (LGMD) ?
Limb-girdle muscular dystrophy (LGMD) is not a single, but a rare group of inherited genetic disorders which are characterized by progressive weakening of the proximal muscles of the shoulder and hip. ( Distal muscles are farther away from the center — for example; the proximal muscles are those closest to the center of the body) .It is a different group of disorders with many sub-types classified by disease gene and inheritance.
The bony structure surrounding the hips is called a pelvic girdle and the bony structure that surrounds the shoulder area it’s called a shoulder girdle. Collectively, these are called the limb girdles, and it is the observed weakness and wasting (atrophy) of the muscles connected to the limb girdles that have given this group of disorders its name.
These disorders can now be eminent by genetic and protein analysis.LGMD is a general term that includes several disorders. The diverse forms of LGMD are classified as autosomal dominant or recessive traits. Autosomal dominant are further classified into 8 sub-types (LGMD1A-1H) and may know as LGMD1. Moreover, Autosomal recessive are further classified into 17 sub-types (LGMDA-Q) and known as LGMD2.

Clinically Relevant Anatomy:
LGMD is caused by multiple genes encoding for proteins within the cytosol, nucleus of the myocyte, or sarcolemma. The result of the deficiency is that the muscles cannot properly form certain proteins needed for normal muscle function. Several various proteins are affected, and the specific protein that is imperfect or absent identifies the specific type of muscular dystrophy. The proteins affected in LGMD are a, ß, ?, and d sarcoglycans. The sarcoglycans are a family of transmembrane proteins (a, ß, ? d, or e) involved in the protein complex responsible for linking the muscle fiber cytoskeleton to the extracellular matrix, preventing the damage of muscle fiber sarcolemma through shearing forces.
The dystrophin-glycoprotein complex (DGC) is a membrane-spanning complex that connects the interior cytoskeleton to the extracellular matrix in muscle. The sarcoglycan complex is a sub-complex within the DGC and is controlled by several muscle-particular, transmembrane proteins namely (a, ß, ? d, or e).
Causes Of Limb-Girdle Muscular Dystrophy (LGMD):
There is 33 type of limb-girdle muscular dystrophy (LGMD), and they are classified by the genetic defects that arise to cause them.
In each cell in the body, genes located on chromosomes, are the codes, or recipes, for the generation of the body’s different proteins. The genes connected with LGMD normally make proteins necessary for muscle function.
Protein deficiency arises because one of these genes is faulty, muscle fibers do not work properly. Gradually, the muscles become weak and people feel the symptoms of LGMD. Because LGMD is progressive, the muscles continue to become weaker throughout a person’s time of life.
During muscle contraction, a thin sheath around each muscle cell, help to protect from injury. If any of these proteins is missing, the membrane loses some of its “shock-absorber” characteristics and has a harder time protecting the muscle cell from injury during relaxation and contraction cycles.
The types of LGMD are classified by letters and numbers that show which gene is suspected or known to be involved, whether the disease is inherited as a dominant or recessive condition, meaning whether one or two defective genes are needed to cause it.
Inheritance:

How is LGMD inherited?
As mentioned above LGMD, mostly affected the muscles which are surrounding the shoulders and hips, with proximal muscles in both the upper and lower legs. These muscles are shown in red. Inside each muscle cell, many proteins, some of which are shown in yellow-orange and blue, due to the cell contract and protect from contractions.
When any of the proteins shown in yellow-orange are missing or unusable. Six proteins are normally found in the muscle cell membrane, a sheath surrounding each cell. Establishing which proteins are absent in LGMD and the normal functions in the muscle cell are important steps in the development of treatments.
The muscles most affected in LGMD are those around the shoulders and hips, with muscles of both the upper and lower limb, sometimes the legs and arms also weak. These muscles are shown as red in color. Inside some muscles shown in blue and yellow-orange, cells contract and protect them from the stress of contractions. When any of the proteins shown in yellow-orange are nonfunctional or missing. Minimum six of these proteins are normally found in the muscle cell membrane.
LGMD can be inherited in basic paths that are known as the autosomal recessive and the autosomal dominant. The word “autosomal” means that the genes affected are not on the X or Y chromosome, they are passed on from men, women, or both.
Signs and Symptoms Of Limb-Girdle Muscular Dystrophy (LGMD):
There are some recognizable main types of LGMD, severity, progression of symptoms and the age at onset associated with LGMD may vary greatly from case to case, even among members of the same family. Some cases of LGMD may have onset during mild symptoms, adulthood, and slow progression; others may have onset early severe disability such as difficulty in climbing stairs and walking. Some individuals require a wheelchair.
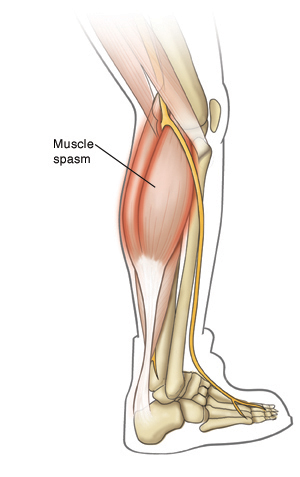
Muscle weakness usually affects the muscles of the pelvic and hip area first and affected individuals may have difficulty standing from a sitting position or walking upstairs. Weakness of the hip and upper leg muscles may cause a different waddling gait. Eventually, mostly affects the muscles of the upper arms and shoulders (limb-girdle area). Consequently, affected individuals may have difficulty raising their arms over their heads or lifting up heavy objects. Muscle weakness may be associated with soreness in the joint pain and muscles.
Abnormalities that may develop in individuals with LGMD include abnormal front-to-back curvature of the spine (lordosis) abnormal side-to-side curvature of the spine (scoliosis), thickening and shortening of tissue that cause deformity and restricts movement of affected areas, specially overgrowth (hypertrophy) and the joints (contractures) of certain muscles such as the calf muscle.
In some forms of LGMD, weakening of the heart muscle is known as cardiomyopathy. Cardiomyopathy is a condition that may result in an impaired ability of the heart to pump blood, heart block, irregular heartbeats (arrhythmias), fatigue, and heart failure. Heart abnormalities are not connected with all forms of LGMD.The respiratory system may also be involved in some cases resulting in slurred speech (dysarthria), difficulty swallowing (dysphagia), and breathing difficulties. Breathing difficulties may become progressively dangerous in such cases.
Autosomal Recessive LGMD:
It has 17 different subtypes of autosomal recessive LGMD have been identified. These disorders are characterized by muscle weakness of the shoulders, legs, arms, and pelvic girdle. increasing of muscle weakness may be rapid or slow and may differ even among individuals in the same family. Intelligence is normal. The age of onset differs from subgroup to subgroup. Overall, it is more common in childhood but it may even occur late in adult life.
LGMD2A (calpain-deficient LGMD; calpainopathy)
This type of LGMD usually affects children between the ages of 8-15, but may range from 2-40 years of age. Most of the cases are characterized by the hip-girdle area affecting muscle weakness although the spread of the hip adductor muscles. Degeneration (wasting) is prominent. The affected child may show a clear waddling gait and may fall frequently. They may also experience climbing stairs and difficulty running. Respiratory problems have been reported, but heart abnormalities have not been.
LGMD2B (dysferlinopathy)
The onset of this form of LGMD is usually during the immature years. Most individuals have normal mobility during childhood. Muscle weakness affects both the pelvic and shoulder area but usually progresses very slowly. an inability to walk on tiptoes and wasting (atrophy) of the calf muscle may be seen early in the stage. In rare cases, painful swelling of the calf, temporary (transient) overgrowth of the calf muscle, and early development of contractures may occur. The respiratory system and heart muscles are usually not affected.
The cause of LGMD2B is mutations of a gene that also causes Miyoshi myopathy a rare muscle disorder characterized by weakness of the distal muscles of the upper and lower limb (arms and legs).
LGMD2C-2F (sarcoglycanopathies)
This type of LGMD may often be from childhood-onset to a mild form often with adult onset. The severity varies greatly among individuals with the same family members. Initial onset forms may cause progressive muscle weakness of the abdomen, hips, legs, and shoulder. The progression of muscle weakness of the sarcoglycanopathies is more rapid than with other forms of LGMD and affected individuals may need a wheelchair between 12-16 years of age. Individuals usually experience a slower progression and more mild symptoms. Such individuals usually retain the ability to walk independently into adulthood.
Additional symptoms are correlated with the sarcoglycanopathies including overgrowth of the tongue and calf muscles, contractures, respiratory abnormalities, scoliosis, and cardiomyopathy.
LGMD2G (telethoninopathy)
This type of LGMD usually becomes visible during childhood or adolescence and presents with muscle weakness of the upper and lower legs. Affected children may have difficulty running and climbing stairs. Affected individuals need a wheelchair by the third or fourth decade. Heart abnormalities may occur in approximately half of the reported cases. Hypertrophy(Overgrowth) of the calf muscle may also occur.
LGMD2H (TRIM 32 mutations)
This type of LGMD has been reported in the Hutterite population of Manitoba, Canada. Affected individuals have been developing muscle weakness of the lower limbs that may be mild or severe. Facial muscle weakness may also occur. As the disease progresses, arm muscles may become involved. Affected individuals may remain able to walk well into their adult years.
LGMD2I (fukutin-related proteinopathy)
This type of LGMD may range from mild to severe. The initial childhood stage of LGMD2I usually indicates a severe clinical course with affected people needing a wheelchair by the second decade. There is overlap with an inherent form of muscular dystrophy, MDC1C. In some cases, affected individuals have weakness of muscle in both the arms and legs, delays in attaining motor milestones, and loss of muscle tone (hypotonia). The late or adult form of LGMD2I is progress slow as, a mild form of the disorder. LGMD2I is also connected with respiratory and cardiomyopathy abnormalities.
LGMD2J (titinopathy)
This type of LGMD occurs when two titin gene mutations are present and has a different age of onset ranging from 10-30 years. Affected individuals have proximal muscle weakness. The distal muscles become involved and some people may need the use of a wheelchair. Distal myopathy can be seen, when only one titin gene mutation is present.
LGMD2K
This is an extremely rare type of LGMD that has been reported in Turkish people. It occurs during infancy or the initial phase of childhood. Affected people show slowly progressive muscle weakness and most retain the ability to walk into late adolescence. All affected people had developmental put off.
LGMD2L (anoctominopathy)
Affected people were reported to have weakness of proximal muscle in both lower and upper limbs and muscle hypertrophy was common. Development of knowledge(Intelligence) was reported to be normal.
Recessive LGMD with primary alpha-dystroglycan defect and causative genes have been identified for LGMD2K, LGMD2L, LGMD2M, LGMD2N, LGMD2O, and LGMD2Q.
Autosomal Dominant LGMD:
The autosomal dominant type of LGMD occurs less frequently than the autosomal recessive type and is more likely to occur later phase of life. In such cases, autosomal dominant LGMD progresses at a slower rate than autosomal recessive LGMD and has symptoms that can be different, even among members of the same family. Many different groups of symptoms are caused by each gene mutation.Examples of some of the symptoms that can be connected with specific gene mutations are as follows:
LGMD1A (myotilinopathy)
The onset of LGMD1A differs, ranging from juvenescence to adulthood. This form of LGMD is characterized by proximal muscle weakness sometimes it leads, to an abnormally tight Achilles tendon and to slurred speech (dysarthria), and arm Muscle weakness may also occur. The distal muscles may also become involved as well. The progression of LGMD1A is extremely slow and only a few affected people need a wheelchair. In some cases, the heart has been also involved. The group of diseases known as myofibrillar myopathies is another heterogeneous group of muscle diseases, which may also be associated with myotilin mutations.
LGMD1B (lamin A/C)
This type of LGMD is characterized by slow weakness of proximal muscles. Affected people may also develop hypertrophy (overgrowth) of calf muscles and minor contractures of the elbows or Achilles tendon. Heart abnormalities are common and should be screened for including progressive conduction defects that can ultimately lead to heart block and arrhythmias (irregular heartbeats).
LGMD1C (caveolinopathy)
This type of LGMD is characterized by after exercise, cramping muscle pain is seen. Overgrowth of the calf muscle and mild to moderate proximal muscle weakness. Development of muscle weakness may be slow or rapid. It is usually during the initial stage of childhood. Patients may have so-called rippling muscles.
LGMD1D
This is a rare type of LGMD characterized by progressive muscle weakness that first affects the hip-girdle area before spreading to affect the limb-girdle area. It is usually during the initial stage of adulthood but may occur as late as the sixth decade. Disorder progression is slow. The heart is abnormal including conduction abnormalities and dilated cardiomyopathy. people with this type of LGMD usually remain able to walk.
LGMD1E
This type of LGMD is connected with progressive weakness of the proximal muscles of both the upper and lower legs. It is usually during childhood and the Disorder progression is slow. Affected people may also have difficulty swallowing (dysphagia) and contractures. Heart abnormalities occur in this type of LGMD usually one or two decades after the development of muscle weakness.
Causative genes have not been detected for LGMD1E, LGMD1F, LGMD1G, or LGMD 1H.
Such additional cases of LGMD have been indicated in the medical literature that have not been connected to any of the above-mentioned subtypes and for which no causative gene has been identified.
The signs and symptoms of an LGMD can differ widely, even among people within the same family. Symptoms may begin at any age.
In general, limb-girdle muscular dystrophy symptoms may include:

- Muscle myalgia and cramps
- Difficulty lifting any objects and climbing stairs
- Stiffness of joint
- Arrhythmias and Conduction abnormalities
- Scapular-humeral-pelvic weakness, which may be similar to Facioscapulohumeral Dystrophy (FSHD), but without facial weakness.
- Muscle wasting (atrophy)
- Contractures
- Face muscle weakness
- Abnormal arch of the spine, such as lordosis and scoliosis.
- Gradual development
- Gower’s sign may be present
- Understanding and knowledge are usually normal
- Waddling gait – foot drop, gait dysfunction, weakness of hip musculature
- Scapular Winging
- Low back pain
- Palpitation
- Inability to get back position from a squatting position without using the arms
- Pseudohypertrophy of calf muscles
- Unable to do overhead activities
- The progressive problem for self-care and movements
- Slurring speech
- Cardiomyopathies
- Trouble in breathing
- Respiratory shortage
- The problem with long-distance walking
- Inability to transports
- Reduced toleration and endurance to activity
Investigations Of Limb-Girdle Muscular Dystrophy (LGMD):
LGMD can be complicated to diagnose because its signs and symptoms closely approximate those of related disorders. For many people, achieving a precise diagnosis takes several years.
Diagnosing Limb-Girdle: Diagnosing for limb-girdle muscular dystrophy includes ruling out other, similar disorders. We use advanced testing, including:
Complete physical examination and medical history, including the family history of muscular dystrophy or any other neuromuscular disorder.
Electrodiagnostic tests (EMG/NCS): Neuromuscular neurologists assess nerve function and the muscle using a machine that measures electrical signs in people’s muscles and nerves.
Laboratory tests: These tests may be used to check the enzymes of muscle, as well as other clues to diagnosis.
Muscle biopsy: Examine the small sample of muscle tissue for checking the abnormalities.
Imaging studies: Non-invasive testing is used including ultrasound, magnetic resonance imaging (MRI), or CT scan.
Electrocardiogram (EKG): Non-invasive testing is used to check heart rhythm.
Genetic testing: Examines the people’s genes to look for deformities known to cause limb-girdle muscular dystrophy.
Treatment Of Limb-Girdle Muscular Dystrophy (LGMD):
Medical Treatment:
There is no specific treatment protocol for LGMD disorder and treatment is based on the presentation of the case.
Cardiac Involvement – Placemaker placement is a life-saving procedure. The case should be referred to a cardiologist or surgeon. Other methods of treatment are implantable defibrillators or anticoagulant drugs,
Respiratory Symptoms – Initial mediation to treat the respiratory deficiency with non-invasive ventilation can help improve the function and life expectancy of the patient.
Dysphagia and Nutrition – Enteral feeding (gastrostomy tube) or nutritional supplementation.
Skeletal abnormalities – Muscle weakness causes an abnormal posture and it can lead to scoliosis/lordosis/kyphosis in later stages. It can be corrected by orthopedic procedures like spinal fusion, spinal correction, and spinal decompression.
Pain and inflammation – Non-inflammatory drugs can be given to delaying the progression of the disease.
Physiotherapy Treatment Of Limb-Girdle Muscular Dystrophy (LGMD):
The aim of physiotherapy is to maximize function and prevent contractures.
Low force aerobic exercise with submaximal strength practice usually benefits overall health and safety.
Gentle low force aerobic exercise increases cardiac endurance (swimming and stationary cycle or treadmill)and function.
Simple exercises include:
- Sit to stand
- Sidestep
- Backward walk
- Marching in place
- Step-ups
- Step-taps
- Step-overs
- Soccer kicks
Exercises For Limb-Girdle Muscular Dystrophy (LGMD):
Upper Limb Range of Motion Exercises (ROM):
Shoulder ROM:
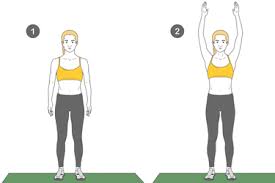
Shoulder flexion:
Position: standing
Instruction: Begin with your arms straight at your side. Keep your elbow straight and lift one arm up over your head as far as possible. Hold for 10 seconds and repeat 10 times.

Shoulder extension:
Position: standing
Instructions: Move your arm backward and do not lean forward while performing. Hold for 10 seconds and repeat 10 times.
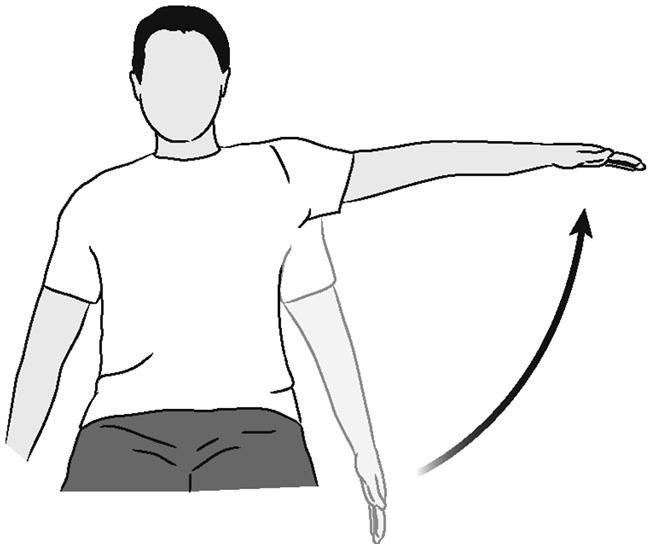
Shoulder abduction:
Position: sitting
Instruction: Lift your arm out to the side with a palm up and Keep your elbow straight. Hold for 10 seconds and repeat 10 times.

Shoulder rotation:
Position: sitting
Instructions: Place your arm behind the head and Bring your arm behind your back. Hold for 10 seconds and repeat 10 times.
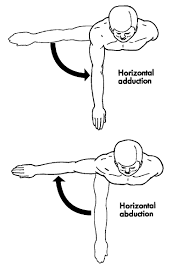
Horizontal shoulder abduction and adduction:
Position: sitting or standing
Instructions: Hold your arm out to the side at shoulder level and reach your hand out and bring it across your body. Keep elbow straight and Hold for 10 seconds and repeat 10 times.
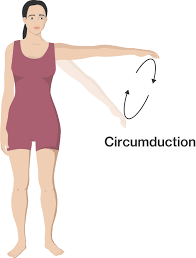
Shoulder circumduction:
Position: sitting or standing
Instructions: Hold arms out to the side at shoulder level and move arms in a circle, clockwise, five times, and then anti-clockwise five times. Repetition is 10 times each.
Elbow ROM:

Elbow flexion and extension:
Position: sitting
Instructions: Bend and straighten your elbow and hold for 10 seconds and repeat 10 times.
Forearm pronation and supination:
Position: sitting with forearm support
Instructions: Turn the palm upward keep the elbow at the side and turn the palm down and hold for 10 seconds and repeat 10 times.

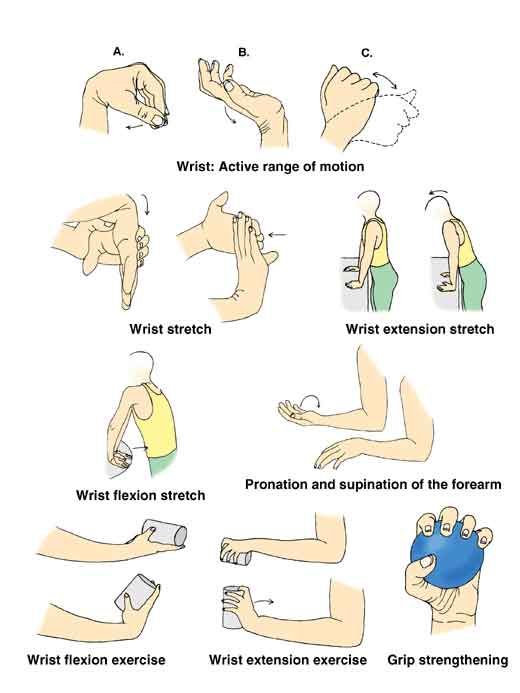
Wrist flexion/extension:
Position: sitting with forearm support
Instructions: Begin with palm down and raise hand up and then bring it down. Hold for 10 seconds and repeat 10 times.
Scapular Exercise

Retraction:
Position: standing
Instruction: At waist level put the band around a solid object, such as a bedpost, with your elbows at your sides and bent to 90 degrees, and pull the band back to move your shoulder edges toward each other.
Repeat 8 to 12 times.
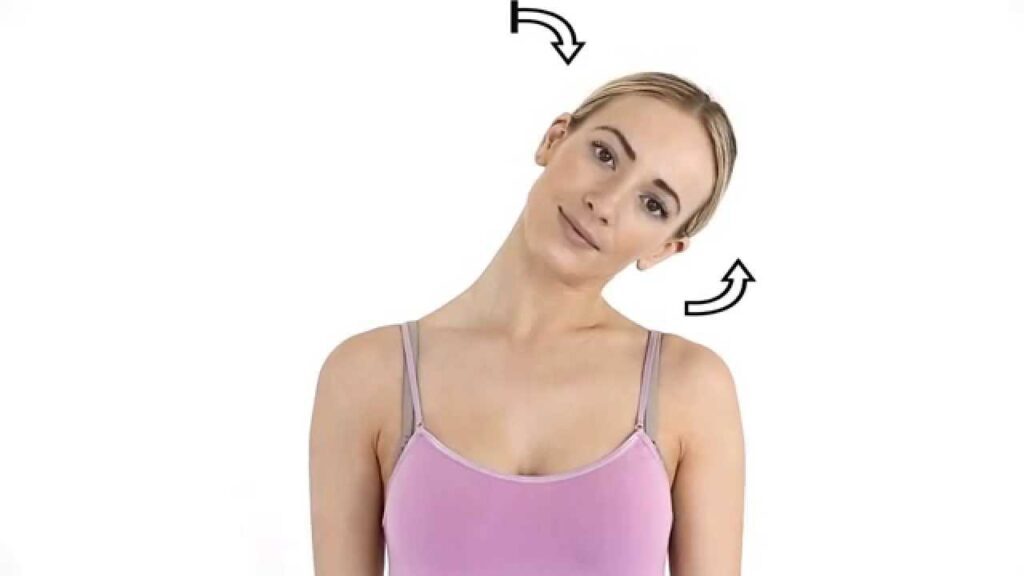
Lateral flexion of the neck:
Position: sitting and touching the ear to the Shoulder
Instructions: Gently bend your neck in try to touch your right ear to your shoulder. Stop when you feel the stretch on the left side of the neck. Hold for 20 seconds and then back to starting position. Repeat the above stretch four 3-4 times.

Neck forward flexion:
This exercise is used to loosen the tension of the neck and shoulders.
Position: sitting
Instructions: Bend your chin toward your chest and gently tilt your head to the left to stretch your right shoulder. You will feel a stretch along with the back of your neck. Hold this position for up to 1 minute after that repeat on the opposite side. Do each side 3–5 timesRange of motion (ROM) upper limb:
Upper Limb Stretching Exercises:

Wrist flexor stretch:
Position: sitting
Instructions: Extend your arm in front of you with your palm up and bend your wrist, showing your hand toward the floor. Gently bend your wrist further until you feel a mild to moderate stretch in your forearm, with your other hand. Hold for at least 15 to 30 seconds and repeat 2 to 4 times.

Raised fist stretch:
Position: sitting
Instructions: With your hand open, start with your arm up beside your head. Make a fist, keep your thumb outside of it. Until you feel a stretch Slide your fingers toward your wrist.

Wrist rotations:
Position: standing
Instruction: Use the other hand to gently pull the raised hand toward the body and stretch your arm out in front of you. Until you feel a stretch, slowly point the fingers down. Moreover, point the fingers toward the ceiling until you feel a stretch. This position was held for 3–5 seconds.

Prayer position:
Position: sitting
Instruction: Sit with your palms together and your elbows on the table in a prayer position. Until you feel a stretch lower the sides of the hands toward the table. Keep your palms together. Hold this position for 5–7 seconds.
Relax.
Repeat this three times.

Hooked stretch:
Position: sitting
Instructions: Hook one elbow under the other and pull both arms towards the center of the torso. You feel a stretch in your shoulders. Unfold one arm around the other so that the palms are touching. Hold the position for 25 seconds and switch arms and repeat it on the other side.

Finger stretch:
Position: sitting
Instructions: Separate the middle and index fingers from the ring finger and bring the little and ring fingers together. Repeat the stretch 10 times.
Fist-opener:
Position: sitting
Instructions: Make a fist and hold it in front of you. Stretch your fingers until your hand is open, with the fingers together. Repeat the movements 10 times.

Sponge-squeeze:
Position: sitting
Instructions: Stress ball, make a fist, or squeeze a sponge. Hold the position for 10 seconds.
Relax.
Repeat this 10 times.

Windshield wiper wrist movement:
Position: supine lying
Instructions: Start with your hand face down on a table. Gently, without moving the wrist point the hand to one side as far as it can go Hold it there for 3–5 seconds. Do the same on the other side.
Repeat the movement 3 times on each side.

Thumb pull:
Position: sitting
Instruction: Grasp your thumb with the other hand. Pull the thumb backward, away from the hand. Hold the stretch for 25 seconds. Repeat it on the other thumb.
Alternate finger stretch:
Position: sitting
Instructions: Bring the middle and ring fingers together. Separate the little and index fingers from them. Repeat the stretch 10 times.
Wrist-strengthener:
Position: sitting
Instructions: Get into position on your hands and knees, with the fingers pointing toward the body. Slowly lean forward and keep your elbows straight. Hold the position for 20 seconds.
Relax, then repeat the stretch.
Lower Limb Strengthening Exercises:

Straight leg raise (SLR):
Position: supine lying
Instructions: Lying on your back, legs straight and together. Keep your legs straight and lift them up to the ceiling until your butt comes off the floor. Lower your legs back down slowly till they’re just above the floor. Hold for 10 seconds and your legs back to the starting position and then repeat.

Donkey kicks:
Position: Quadriped position
Instructions: Bracing your core with knees and hips slightly bent, use your glute to kick your working leg directly back as high as it will go without compromising your hip position. Squeeze at the top. Resist the weight and slowly lower your foot back to the. position. Complete 10-12 reps for 2-4 sets on each leg.

Quadruped superman:
Position: Quadriped position
Instructions: Start on your hands and knees. Raise your right arm off the floor and reach ahead at the same time raise your right leg off the floor. After that same is done on another side, raise your left arm and your right leg at the same time.

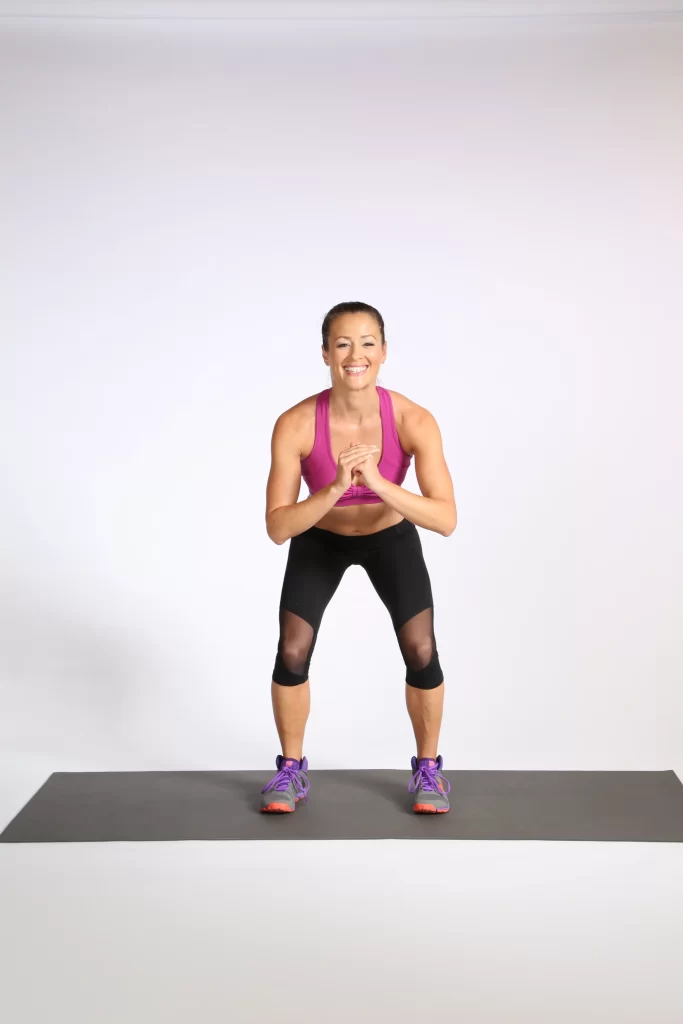
Bodyweight Squat or Mini-Squat:
Position: standing
Instructions: Stand with your feet hip-width apart, your toes pointing slightly outward or straight outside. Keep your weight on your heels and your hips backward, bending your knees as if sitting down on a chair.
Lower Limb Stretching Exercises:

Lower Limb Stretching Exercises:
Quadriceps stretching:
Position: standing
Instructions: Stand on your left foot and grab your right by bending your leg behind you. Tuck your pelvis in, pull your shin toward your glutes, and make sure that your knee is pointing to the ground. Try not to pull the knee sideways or backward. Hold for 30 seconds and then switch sides.

Hamstrings stretching:
Position: long sitting
Instructions: With both legs out straight sit on the floor. Extend your arms and reach forward by bending at the waist as far as possible during this try to keep your knees straight. Hold this position for 15 to 30 seconds.
Relax back into the starting position.
Repeat three times.

Hip adductors stretching:
Position: supine lying
Instructions: Lying on your front bend the knee to 90 degrees and then slowly let the footfall away from the body. Try to keep the knees together and hold the position at the end of your comfortable range. Repeat.

Hip abductors stretching:
Position: standing
Instruction: Stand facing a wall with the feet together. Place the hands on the wall or the hips for balance. Without rotating the hips, raise the left leg out to the side as high as possible. Hold for 5 seconds and then return to the starting position and repeat 10 times, and then repeat on another side.

Calf stretching:
Position: standing position
Instructions: Standing and facing toward a wall from 3 feet away. Take one step toward the wall with your foot. Place both palms on the wall. Bend your right knee. Lean forward, keep the other leg straight and the heel on the floor.
Trunk Exercises:

Trunk rotations:
Position: supine lying
Instructions: Bring both knees up and keep your feet flat on the ground then just rotate your knees to one side trying to keep your upper body flat on the ground and then switch to the other. Side you.

Lateral bending of trunk:
Position: standing position
Instructions: Shoulder width apart, stand with your feet a little wider. Raise your right arm over your head and slowly lean to the left. Keep your stomach tight. During leaning, you feel the hip and stomach muscles pulled. Repeat with the other side.

Crunches:
Position: supine lysing
Instructions: Starting with forwarding crunches maintain posture and lie flat on the floor. For stability, hands behind your head and balance crunch forward so as to squeeze the muscles just below the ribcage.
Lateral Walk :
Instructions:
- Position is standing with your feet hip-width apart and squatting down into an athletic position.
- Take the first step on the left with your left foot till your feet are shoulder-width apart.
- The next steps on the right with your right foot till your feet are hip-width apart.
- Keep taking small steps to the left and then repeat on the right side.

Toe tap-ups:
- Lie down on an exercise mat with your knees bent and arms at your sides.
- Lift both feet off the floor and extend your legs up until your thighs are perpendicular to the floor. …
- Fully extend your arms until your fingertips are pointing towards your toes.
- The abdominals and lift your torso off the floor.

Heel raises exercise:
Instructions: Stand with your feet about 10 centimeters apart, with your hands lightly resting on a counter or chair in front of you. While keeping your knees straight slowly raise your heels off the floor. Hold for 6 seconds, then slowly touch your heels to the floor.
Complications:
People with limb-girdle muscular dystrophies may experience complications such as:
- Heart problems.
- Heart rhythms are abnormal.
- Facing trouble while using arms.
- People may face difficulties in way of life activities because of shoulder weakness.
- Gradually weakness may result in needing a wheelchair.
- Difficulty in walking.
- Contractures of the various joints or shortening of the muscles round the joints.
- Scoliosis (Curved spine)
- Swallowing problems may occur.
- Difficulty in breathing.