Ankle Fracture
Table of Contents
What is an Ankle Fracture?
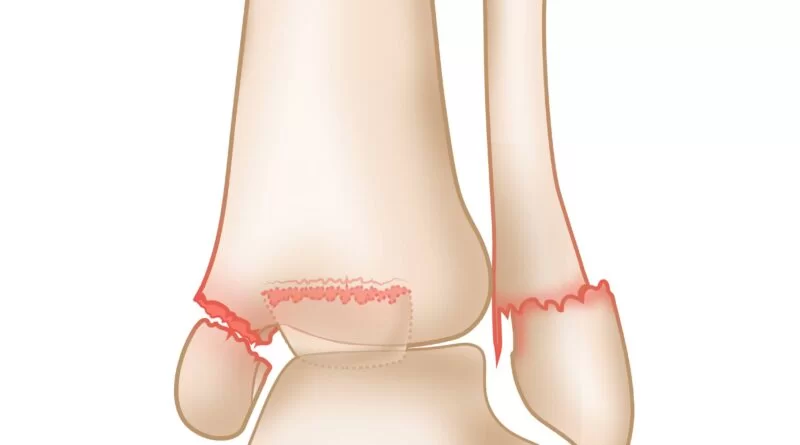
An Ankle fracture refers to a break or a crack in one or more bones that form the ankle joint. Ankle fractures are usually caused by a sudden twist or force on the ankle, such as during a fall or a sports injury.
Symptoms of an ankle fracture may include severe pain, swelling, bruising, difficulty bearing weight or walking, and deformity or misalignment of the ankle. Ankle fractures can range in severity from a simple crack in the bone to a complete break, which may require surgery to repair.
A fracture is a break of the continuity of the bone. Fractures of the ankle joint are familiar among elders. Kannus et al. document an incidence of up to 174 cases per 100 000 individuals per year in a Finish population. Fractures of the foot are rare.
Ankle fractures are most generally diagnosed via clinical assessment and X-ray. Ottawa rules deliver clinicians with a means to determine whether the joint should be imaged or not. various types present and are utilized to decide the severity of injury and management. Examples comprise the Danis-Weber classification which determines the level of injury and; the Lauge-Hansen type which is based on the mode of the injury and has predictable patterns and imaging results.
Complications of ankle fractures may have decreased range of motion at the ankle and foot joints, as a result of peri-articular and intra-articular adhesions or disruption of articular surfaces. Disruption to articular surfaces may result in the development of osteoarthritis.
Fractures in the absence of displacement can be managed with a below-knee cast that may be used for 3-6 weeks. If displaced, a physician must reduce the broken piece to the normal anatomical position of the joint. If not possible to be achieved by closed reduction and plaster cast, a person may have to undergo an open reduction with internal fixation (ORIF) with immobilization in a plaster cast.
General ankle fractures are:
- Potts Fracture
- Avulsion Fractures
Clinical Anatomy
The ankle joint also called the talocrural joint, is constructed by the three bony structures: the lower ends of the tibia (commonly named as shinbone) and fibula, proximally, and the talus, distally. The tibia and fibula have particular characteristics that construct up the ankle:
- Medial malleolus – inside aspect of the tibia
- Posterior malleolus – the posterior aspect of the tibia
- Lateral malleolus – end portion of the fibula
The tibia and fibula construct the ankle joint with structure and strength provided by the subsequent connective tissues:
- Interosseous membrane
- Anterior, posterior, and transverse tibiofibular ligaments
The collateral ligaments support the joint in front of abduction and adduction forces. Laterally, the anterior talofibular ligament (ATFL), calcaneofibular ligament (CFL), posterior talofibular ligament (PTFL), and, medially, the wide fan of the deltoid ligament and the plantar calcaneonavicular ligament, whose medial border is combined with the forepart of the deltoid ligament.
The foot
The foot incorporates 26 bones. The foot is separated into three major components: hindfoot, midfoot, and forefoot.
- Hindfoot has included 2 bones: calcaneus and talus. They construct the subtalar joint.
- Midfoot is made up of 5 bones: navicular, cuboid, and 3 cuneiforms (medial, intermediate, and lateral). The bones are attached to the forefoot and the hindfoot by muscles and the plantar fascia (arch ligament).
- Forefoot included 19 bones: 5 metatarsals and 14 phalanges.
The Chopart joint is the relation between the hindfoot to the midfoot involving the ‘talonavicular joint’ and the ‘calcaneocuboid joint’; the Lisfranc joint joins the forefoot to the midfoot.
Causes of Ankle Fracture
Caused of the ankle fracture is by traumas for example falls, twisting injuries, and sports-related injuries. It happens in both older and younger populations.
There are various threat factors linked with an increased risk of maintaining foot and ankle fractures. These are smoking, diabetes, obesity, prior falls and or fractures, very high or low levels of physical activity, and low bone mineral density (BMD). For older people over the age of 50, additional risk elements have female gender, comorbidities, and multiple medications.
The highly active life in younger men, especially in risk-taking and sports activities, may justify the increased rates of ankle and foot fractures in this year’s group. Younger women, under the age of 50, although less active than males have a greater propensity to fall, after in life which overlaps with postmenopausal bone loss; this outcome in an increase in fracture threat
Symptoms of Ankle Fracture
- Problems or inability to walk or bear weight on the ankle (it is likely to walk with less intense breaks, so depending on walking as a test of whether a bone has been fractured is not trustworthy)
- Pain
- Swelling
- Bruising (soon afterward the injury)
- Difference in appearance
- Observable differences compared to the unaffected side
During an ankle break, there is not only structural damage to the skeletal structure but also to the ligaments (deltoid ligament and the anterior and posterior tibiofibular ligaments) and also nervous and musculoskeletal tissue near the ankle complex. This can cause impaired balance capacity, decreased joint position sense, slowed nerve conduction, and velocity, poor cutaneous sensation, and reduced dorsal extension range of motion.
Fracture Classifications
Ankle fractures can be classified depending on either the AO or OTA, Danis-Weber, or Lauge-Hansen classification system.
The Lauge-Hansen classification depends upon a rotational mode of injury. There are four classes and 13 subgroups of ankle fractures detailed in the given below.
Supination external rotation (SER)
Stage (subgroups)
- Damage of the anterior inferior tibiofibular ligament
- Oblique or spiral fracture of the distal aspect of the fibula
- Damage of the posterior inferior aspect of the tibiofibular ligament
- Medial malleolus fracture or damage to the deltoid ligament
Supination adduction (SA)
- Transverse fracture of the distal aspect of the fibula
- Vertical fracture of the medial malleolus
Pronation external rotation (PER)
- Medial malleolus fracture or damage to the deltoid ligament
- Damage to the anterior inferior tibiofibular ligament
- Oblique or spiral fracture of the fibula proximal aspect of the tibial plafond
- Damage of the posterior inferior aspect of the tibiofibular ligament
Pronation abduction (PA)
- Medial malleolus fracture or damage to the deltoid ligament
- Damage to the anterior inferior aspect tibiofibular ligament
- Transverse or comminuted fracture of the fibula proximal aspect of the tibial plafond
The Danis-Weber type depends on X-ray criteria. It took into consideration the position of the distal aspect fibular fracture in connection to the syndesmosis of the ankle joint. Three classes were created:
- Type A fracture: below the level of the tibial plafond (syndesmosis) and can be related to oblique or vertical medial malleolar fractures
- Type B fractures: at the level of the tibial plafond (syndesmosis) and spread oblique fashion in the proximal aspect
- Type C fractures: proximal aspect to the level of the tibial plafond and usually have related syndesmotic damage. It may be related to medial malleolus fractures or damage to the deltoid ligament.
AO type or OTA system types all long bone fractures with a well-ordered process, relying on area, topography, and severity of the bony lesion. It depends upon X-ray criteria and includes the mode of injury. The fractures are typed as infra syndesmotic, trans syndesmotic, and supra syndesmotic with further subcategories depending on the existence or lack of medial or posterior malleolar damages.
The AO and Lauge-Hansen type systems are largely utilized in the clinical examination of injuries of the ankle. The AO classification system is easy to comprehend, highlighting the coordinating function of the fibula and syndesmosis of the ankle joint. The Lauge-Hansen type system shows the various phases of pathological damage in addition to the fracture pattern, and it insists on understanding the damage to the ankle ligament system. It can provide a detailed examination of ankle injuries.
Differential Diagnosis
- Rheumatoid Arthritis
- Gout and Pseudo gout
- Ankle Dislocation
- Ankle Impingement
- Compartment Syndrome of the Foot
- Deep Venous Thrombosis
- Peroneal Tendinopathy
- Sinus Tarsi Syndrome
- Ankle ligament sprains
The symptoms of some subtle fractures of the ankle may be similar to that of ankle sprains. This similarity makes an ankle fracture frequently misunderstood as an ankle sprain. These injuries are quite different and required an accurate and initial diagnosis.
Diagnostic Procedures
Ottawa rules
An ankle X-ray is just required if there is any pain in the malleolar zone and any one of the following given below:
- Tenderness at bone along posterior end of the tibia or tip of the medial malleolus, or
- Tenderness at bone along the distal six centimeters of the posterior end of the fibula or tip of the lateral malleolus, OR
- It is difficult to put weight both immediately and in the emergency department for four steps.
Also, the Ottawa ankle rules show whether a foot X-ray sequence is needed. It chose that it is suggested if there is any pain in the midfoot area and any one of the following:
- Tenderness at bone at the base of the fifth metatarsal (for foot injuries), OR
- Tenderness at bone at the navicular bone (for foot injuries), OR
- It is difficult to put weight both immediately and in the emergency department for four steps.
Ankle fractures are originally assessed by physical examination and observed by X-ray.
To decrease the use of X-rays, an infrasound machine can be utilized to find malleolar fractures even though it cannot be depended upon just due to an 85 percent sensitivity and 52 sensitivity.
Therapeutic ultrasound had excellent sensitivity and specificity for analyzing fifth metatarsal, lateral, and medial malleolus fractures in patients with foot and ankle sprains. Regardless, the sensitivity and specificity of therapeutic ultrasound for navicular fractures were not very high.
Treatment of Ankle Fracture
Medical Treatment
Many patients with a malleolus fracture need 6 weeks of immobilization. Patients who undergo early non-displaced fracture or were treated for operation will typically need four weeks of non-weight bearing in a below-knee cast or removable walking boot, observed by two weeks in a walking cast. The removable boot will permit earlier range-of-motion movements.
Surgery is needed for various kinds of ankle fractures. While not always required, surgery for ankle fractures is expected. The demand for surgery relies on how ankle joints appear on X-ray and also the kind of ankle fracture.
Surgery aims to reach the smooth anatomical reconstruction of the joint surface and the protection of the injured ligamentous structures to help with the initial postoperative functional treatment of the joint. Sufficient reduction with congruency of the joint has been noted as one of the most significant signs of a good end outcome. Insufficient reduction may result in osteoarthritis.
The timing of traditional surgical therapy relies mostly on the soft-tissue finding and is possible only if the soft tissues are not critically vulnerable (a few hours after the trauma). The demand for surgery relies on how ankle joints appear on X-ray and also the kind of ankle fracture.
While it’s not always required, surgery for ankle fractures can be performed with three kinds of metal plate and multiple screws: one-third tubular plate; locking compression (LCP) metaphyseal plate for lateral aspect malleolar fracture, and Weber B fracture; LCP lower fibula plate Weber A fracture and Weber B fracture.
Physical Therapy Treatment
Fractures that are stable with non-displaced or slightly displaced pieces can be treated conservatively. Type A fractures do not require to be immobilized in a cast, but can rather be treated like external ligament ruptures in a stabilizing ankle orthosis for earlier function with pain-adapted full weight-bearing.
More significant fractures are immobilized and need a rehabilitation program after cast removal. Programs must be patient-centered and take into consideration patient purposes and aspirations. Programs tend to contain ankle mobility, strengthening exercises, weight-bearing, and balancing exercises. Physical therapy must encourage the patient with home exercises and provide proper education, guidance, and do and don’t.
Patients have complained of difficulties with ADLs of the lower extremity, for example, climbing stairs, and walking, and lessened participation in work and enjoyment. other complaints can be pain, swelling, stiffness, wasting muscle atrophy, reduced muscle torque, impaired ankle mobility, insufficient balance capacity, and improved ankle circumference at the ankle after cast removal.
Passive joint mobilization can be employed to work on the difficulties of pain and joint stiffness, in order to permit an earlier return to activities. For this strategy, the physical therapy glides the articular surfaces of a joint to deliver oscillatory movements. Manual procedures must be complementary to a protocol that contains active exercise.
Strength exercise may be useful after fracture and should be regarded as an important rehabilitation choice by physiotherapy. Lack of strength is one of the most ordinary complications of an ankle fracture.
FAQ
Purchase a specialized pillow, for example, a body pillow, for elevation—keeping the fractured bone above your heart to avoid blood from pooling and resulting swelling. Attempt sleeping on your back first while supported up on a few pillows. If that doesn’t work, gradually adjust yourself to a side-line position if practicable.
Bony injuries and fractures near the ankle joint are colloquially called Pott’s fractures. Accurate anatomical decrease of the fracture by closed or open means is very significant. Any residual incongruity left in the articular surface will result in early degenerative arthritis of the joint.
Generally, a little ankle fracture won’t avoid you from walking. You may even be capable to walk right after the injury. If you have a severe break, you’ll require to prevent walking for a few months. As your ankle gets better, you can gradually return to your usual activities.
A broken ankle usually takes 6 to 8 weeks to recover, but it can take longer. The physician will tell you: how long you’ll have to wear the boot or have the plaster cast on. how much load to put on your ankle – you can be provided crutches or a walking frame to assist keep the load off it.