Scalene Syndrome
Table of Contents
What Is Scalene Myofascial Pain Syndrome?
Scalene myofascial pain syndrome could be a regional pain syndrome wherein pain originates over the neck area and radiates down toward the arm. Scalene myofascial pain syndrome may present as primary or secondary to essential cervical pathology. Despite this, scalene myofascial pain syndrome could be a well-known medical entity. It is often diagnosed as being another pain related to radiculopathies, like thoracic outlet syndrome, cervical spinal stenosis, and cervical disc herniation.
Because this syndrome causes cervical radiculopathy, this condition may additionally result in mismanagement which ends in pain and suffering. In scenarios, patients may commit to surgical intervention. Moreover, clinical findings for this syndrome are “pathognomonic”.
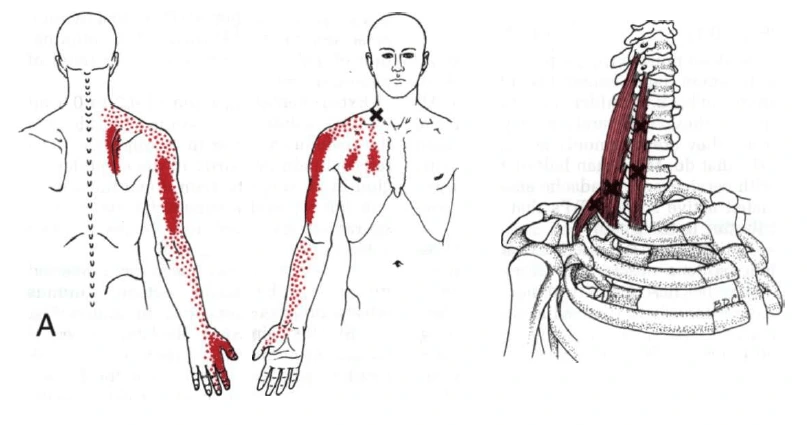
“Myo” means muscle and “fascial” means fascia. It’s a chronic pain condition that causes pain within the system. Fascia is thin and white animal tissue wrapped around all the muscles. This pain is related to trigger points in muscles. Trigger points radiate pain to the affected area when pressure is on sensitive points and sometimes spontaneously with no pressure, and sometimes in seemingly not related body parts. this is often called hurting. This syndrome occurs when muscle contractions are repeated. This syndrome is usually seen in those people that have repetitive movements utilized in jobs or hobbies or by stress-related muscle tension.
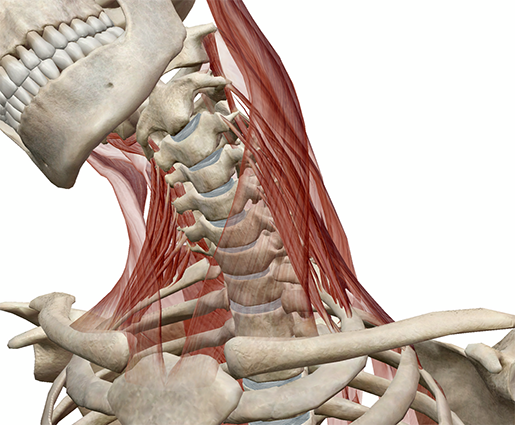
Scalene Muscles
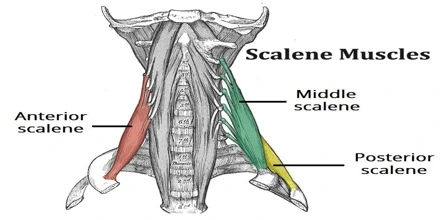
Scalene muscles are a group of three pairs on the lateral side of the neck that is Scalenus anterior, Scalenus medius, and Scalenus posterior. Sometimes a fourth muscle, the scalenus minimus, is present behind the lower part of the scalenus anterior.
Anterior Scalene Muscle
This muscle is one of the lateral sides of the neck muscle, it belongs to the scalene group. It is deeply located and lying behind the Sternocleidomastoid. It is also located between the subclavian vein and the subclavian artery. The phrenic nerve crosses its anterior surface.
Origin: anterior tubercle of transverse processes of the vertebrae C3 to C6
Insertion: anterior scalene tubercle of the first rib, superior border of the first rib (anterior to subclavian groove)
Innervation: anterior rami of spinal nerves C4 to C6
Blood supply: ascending cervical artery branch of the inferior thyroid artery.
Function: bilateral contraction- neck flexion; unilateral contraction- neck lateral flexion (ipsilateral), neck rotation (contralateral), elevation of the first rib.
Posterior Scalene Muscle
This muscle is one of the lateral sides of the neck muscle, it belongs to the Scalene group. It is deeply located and lying behind the Sternocleidomastoid.
Origin: posterior tubercle of the transverse process of the vertebrae C5 to C7
Insertion: external surface of the second rib
Innervation: anterior rami of spinal nerves C6 to C8
Blood supply: ascending cervical artery branch of the inferior thyroid artery and superficial cervical artery
Function: neck lateral flexion, the elevation of the second rib.
Middle Scalene Muscles
This muscle is one of the lateral sides of the neck muscle, it belongs to the Scalene group. It is deeply located and lies behind the Sternocleidomastoid.
Origin: posterior tubercles of the transverse process of the vertebrae C2 to C7
Insertion: superior border of the first rib ( posterior to subclavian groove)
Innervation: anterior rami of spinal nerves C3 to C8
Blood supply: ascending cervical artery branch of the inferior thyroid artery
Function: lateral flexion of the neck, elevates the first rib.
What is the trigger point?
A Trigger Point is a hyper irritable spot and a palpable nodule situated in the taut bands of the skeletal muscles. Muscle contraction or direct compression can provoke jump signs, local tenderness, local twitch response, and referred pain.
Jump sign- it is the characteristic behavioral response to pressure on a trigger point. Some individuals are frequently startled by intense pain. The response is seemingly out of proportion to the amount of pressure exerted by the examining fingers. The head or some other part of the body is not being palpated and is also jerky movement. This sign reflects the extreme tenderness of a trigger point.
Local twitch response -it is defined as when pressure is applied, a palpable contraction of the muscle and skin as the tense muscle fibers contract.
Referred pain- is also called reflective pain. This pain is perceived at a location other than the site of the painful stimulus. There is no specific joint swelling or neurological deficits. Pain from a myofascial trigger point is a distinct, discrete and constant pattern or map of pain with no gender or racial differences able to reproduce symptoms.
A trigger point may also manifest as headache, tinnitus, reduced or decreased range of motion in the legs, and low back pain, temporomandibular joint pain. Palpation of nodules of fibers of muscle harder than normal consistency is the physical finding normally associated with a trigger point. Palpation of the trigger point will provoke pain in the affected area and lead to radiation of the pain. Many modalities, such as the spray and stretch technique, ultrasonography, transcutaneous electrical nerve stimulation, manipulative therapy, and injection are used to inactive trigger points. The trigger point injection treatment is one of the most effective treatment modalities to inactive the trigger points and provides prompt relief of symptoms.
Causes of scalene myofascial pain syndrome
The exact cause of the myofascial syndrome is unknown but it may be due to mechanical stress on the muscle, resulting in the formation of scalene myofascial pain syndrome trigger points.
- weakness of muscle
- Nutritional and vitamin deficiencies
- Changes in hormones
- Chronic infection
- obesity
- Postural abnormalities
- presence of an inflammatory condition
- muscle strain
- lack of exercise
- Due to injuries to muscle, many factors that could result in the formation of trigger points
- Overuse of muscles or trauma
- Lack of muscle activity
- Fatigue
- Stress
- Anxiety
- Sleep disturbances
- Frequent exposure to cold weather
- Repetitive motions or movements
- Such traumatic events as a car accident or sports injury may lead to this condition.
- Ergonomic factors: one is poor posture, which might be due to working at a desk all day; another one may occur due to repetitive overhead activity, such as painting a ceiling.
- Systematic factors and diseases: some vitamin deficiencies, such as iron or vitamin D, may raise a person’s risk of this syndrome. Some health conditions may also cause this syndrome, like hypothyroidism.
Some structural factors: This condition may affect the structure of the musculoskeletal system and may lead to scalene myofascial pain syndrome. Some examples like;
- scoliosis
- Osteoarthritis
- It may develop from a muscle injury or excessive strain on a particular muscle or muscle group, ligament, or tendon.
- a pinched nerve in the neck
- emotional stress
- living or working in a cold environment
Some activities that cause scalene pain:
- Excessive coughing
- Sleeping on your stomach by turning your head on one side
- Wearing a tight collar tie
- lifting weight at arms level with a waist
- gasping of air
- Whiplash injuries
- carrying a heavy backpack
Symptoms of scalene myofascial pain syndrome
- Muscle stiffness
- Fatigue
- Headache
- Dizziness
- Tinnitus
- Mood swing
- Muscle sore
- Weakness in affected scalene muscle
- A tender knot in a muscle
- Difficulty sleeping due to pain
- Stress, anxiety, depression.
- Feeling tired
- Muscle pain fails to improve with time.
- Decrease or reduce the range of motion on the affected side
- Injure muscles are stretched or strained
- Pain like deep aching in the area of scalene muscles, thumb, tight, stiff
- Sleep and behavioral disturbances due to main
- Tenderness in some muscles like; levator scapulae, trapezius, rhomboid, supraspinatus, and infraspinatus
- Neck to Shoulder pain
- Abnormalities in posture may be affected, such as hunching, shoulder rounding, or forward head posture.
Risk factors of scalene myofascial pain syndrome
This syndrome is caused by a stimulus, like muscle tightness, that sets off trigger points in muscles. Some risk factors are may increase the risk of scalene muscle trigger points include:
Muscle injury: An acute muscle injury or stress may cause the development of trigger points. Some examples, like a strained muscle, may become a trigger point. Repetitive movement and improper posture also may increase the risk of causing this syndrome.
Sleep problems: This pain syndrome signs and symptoms may create difficulty sleeping at night. A person may have trouble finding a comfortable sleeping position. And if he/she moves during the night, they might hit a trigger point and awaken.
Fibromyalgia: In a few people, this pain syndrome may develop into fibromyalgia. It is a chronic condition that features extensive pain. It is believed that the brains of people with fibromyalgia become more sensitive to signals of pain over time. A few therapists believe myofascial pain syndrome may play an important role in starting this process.
Stress and anxiety: Some people who frequently feel stress and anxiety may be more likely to develop trigger points in their life.
Diagnosis of scalene myofascial pain syndrome
Diagnosis is usually based on the symptoms. This syndrome is an underdiagnosed and overlooked condition. It might be a problem with a person’s ligaments, tendons, nerves, and bones, but it is not. It is a problem with the muscles. This syndrome is examined depending on which area complaints of muscle pain and tenderness are during an examination. Laboratory testing is unnecessary. There are no changes such as redness, unusual muscle warmth, swelling, etc.
During the examination, the trigger points will be examined by the physiotherapist. For examination, apply gentle pressure with the finger on the painful area of a person’s body or feel for tense areas. There are many ways to provoke pain when pressing with finer on the trigger point, and get responses. On the tender nodules in the taut bands of muscles and gently press to find a pain response. Trigger points can be identified by pain, and they cause muscle pain. When pressing on a trigger point, the therapist will feel for a muscle twitch(also called a “jump sign”).
Essential criteria:
Magnificent place of tenderness in a taut band
The taut band is palpable, where the scalene muscle is accessible.
Patient recognition of the current pain complaint by the pressure given by the examiner
Painful limit to full stretch ROM
Confirmatory observations:
The visual or tactile local twitch response
On compression of the taut band, you may feel the referred pain sensations
SEA confirmed by electromyography
There are no tests. no imaging tests or lab tests/ blood work, electromyography, or muscle biopsy that can diagnose scalene myofascial pain syndrome.
Differential diagnosis
The differential diagnosis depends on patterns of pain. Both entities lead to severe muscle pain and tenderness but they do not have the same etiology or pathogenesis and also their clinical presentation is not the same. Therefore, two different conditions should be distinguished. Myofascial Pain and Fibromyalgia pain feel similar. Both have trigger points that cause pain.
My main differences between Myofascial pain and fibromyalgia:
Myofascial Pain
- Local Pain or one specific area
- Regional Condition
- Palpable of Taut Band
- The pain pattern follows a distribution of muscular referred pain
- Restricted range of motion
- slight weakness of the muscle
Fibromyalgia
- Widespread Pain
- This pain is felt throughout the entire body.
- Fibromyalgia has more trigger points; general pain, a sensation of swelling, irritable bowels, worse fatigue and sleep issues, headaches, and sometimes burning, pickling, or tingling feeling.
- Pain is on both sides of the body. Axial skeletal pain is present in the thoracic or lower back, neck, chest, and so on.
- Absence of taut bands
- Presence of at least 11 tender points
A differential diagnosis made with some other conditions such as:
- Delayed muscle pain
- Muscle spasm
- Neuropathic or radicular pain
- Articular dysfunction
- Infectious myositis
Treatment of scalene myofascial pain syndrome
This syndrome requires a correct treatment plan. No evidence supports using one therapy over another therapy, but exercise is taken into account as a crucial part of any treatment program. We must try quite one approach to find pain relief or reduce pain. Many of us use combined treatment, that’s medication with another therapy that reduces pain and muscle stiffness. Management of Scalene myofascial pain syndrome includes:
Remove the trigger points by stretching, deep heat therapy, massage, medications, and trigger point injections.
Medications
Some Medications like non-steroidal anti-inflammatory drugs (NSAIDs), acetaminophen, or opioids are also used to treat this kind of myofascial pain. Medicines for sleep, depression, or spasm are used, as well. Many medicines will be used for myofascial pain syndrome, including Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs are pain relievers. Over-the-counter pain relievers like ibuprofen (Advil, Motrin, IB, others) and nonsteroidal anti-inflammatory drugs (Aleve) may help some people and will prescribe stronger pain relievers. Some are available in patches that you simply place on your skin. Over-the-counter drugs like acetaminophen (Tylenol) can relieve pain and swelling. Analgesics(Pain-killing medications) are Pain relievers like lidocaine or diclofenac patch, tramadol, COX-2 inhibitors, and tropisetron could also be considered.
muscle relaxants: Benzodiazepines and tizanidine are used for the reduction of muscle spasms.
Sedatives: Clonazepam helps to treat the anxiety and sleep disturbance that sometimes occurs in this syndrome. It must be used because it can cause sleepiness. Sedatives increase the quality of your sleep.
Botox injections: Botulinum A is a potent neurotoxin. It avoids and may have pain-relieving effects and muscle contractions.
Physiotherapy treatment
Physiotherapy treatments may include:
Physiotherapy involves many exercises, like gentle stretching and recovering the full range of motion and motor coordination. Strengthening exercises can start after the trigger point is gone. Once the trigger points are gone, it supports the long-term health of the local muscle system.
A physiotherapist can devise a plan to help reduce or relieve pain depending on signs and symptoms. In some chronic cases of myofascial pain, combinations of physiotherapy, myofascial release therapy (MFR), trigger point injections, or massage are needed.
Many treatments are available and the following modalities help to manage or reduce the pain and restore the affected muscles. Physiotherapy helps to relax, strengthen and stretch the muscles.
Physiotherapy helps to reduce myofascial pain syndrome and may involve:
There are two different approaches to treating psychological trigger points. Non-invasive techniques such as Low-level laser therapy, Therapeutic Ultrasound, and TENS (Transcutaneous Electrical Nerve Stimulation).
Low-level light therapy / cold laser
Lasers are used to stimulate the release of pain-relieving chemicals. A trigger point is exposed to near-infrared light, and low-level light therapy is also known as cold laser.
Ultrasound therapy
Ultrasound is employed to increase the circulation and heat of the blood, which can help with soft tissue healing which is littered with myofascial pain syndrome. These machines transmit sound waves into the soft tissue through a sound-conducting gel applied to the skin. The gel is used to avoid friction between the top of the ultrasound and the skin. The sound waves can heat up and relax the muscles, increasing the flow of blood flow and taking away the connective tissue. In the initial phase, the pain-reducing effects are also minimal, but this treatment may diminish stiffness and increase mobility. This therapy is used for penetrating soft tissues.
This therapy is employed for pain related to atrophic arthritis.
TENS includes a low-voltage electric signal from a tiny low device to the painful area through electrodes that are attached to your skin.
Massage therapy:
There are many types of massage that can relax the myofascial trigger points. These include:
- passive rhythmic release
- active rhythmic release
- shiatsu (acupressure)
- trigger point pressure release
Massage increases the flow of blood and warms up muscles. This can help to reduce pain and stiffness. Therapeutics apply gentle pressure with fingers on the trigger points, which will provoke the pain and then release the tension. Physiotherapists may massage the affected muscle to help reduce the pain. A physiotherapist may use long hand strokes along muscles or place pressure on specific areas of the muscle to release tension. Massage using trigger-point release treatment could also be effective in short-term pain relief. massage may help to improve the condition.
Scalene: Self-massage
Trigger points and tender points can be found on all of these three muscles. For massaging the muscles, especially use the fingertips. Press on the affected part of the muscle and pull the skin over the muscle. Be aware between the front and middle parts where the nerves run. Be careful not to get pressure on that nerve. If you have any difficulty with massaging, you see a professional and ask for help. This muscle is not that easy to massage. Still, if you find tender points and/or trigger points, work them with gentle and precise strokes. Also, be aware while applying a massage to the neck, which is a very sensitive part of the body. In addition, glow gently and get pressure on the exact point.
Myofascial release therapy (MFR)
Myofascial release therapy includes gentle fascia manipulation. Most of these types of release treatments take place during the massage session. Therapeutics will start massaging and stretching the areas that at that time feel rigid with light manual pressure. Your therapist then aids the tissue and sheath in releasing pressure and tightness. The process is repeated multiple times on the same trigger point and another trigger point until the therapist feels the tension is fully released.
In the massage area, a therapist might not be near where the pain originates or where you feel pain most prominently. Myofascial release works the broader network of muscles which may be resulting in pain. It tries to decrease tension throughout your body by releasing trigger points across a broad section of the muscular system. Myofascial release therapy can even be done in reception by employing a tool, sort of a massage gun to use pressure on the muscles and interconnective tissues, or a foam roller. This type of myofascial release is often especially helpful for athletes scuffling with facial tension as a result of repetitive muscle use.
Myofascial Release is the hands-on treatment performed on skin with no oils or any creams. The gentle tension between a therapist’s hands and a patient’s skin is what allows access to the fascia in a way that the gliding effect of a normal massage cannot achieve. The myofascial release incorporates many new styles of body manipulation to enhance function and movement.
Trigger point release therapy
There are some ways you’ll be able to release a trigger point. The foremost common way is using sustained pressure with the thumb, fingers, elbow, or a massage ball or some tool. Dry needling is additionally a style of trigger point therapy that’s becoming more extensive as its effectiveness is being seen.
Manual therapy for trigger points: this generally involves sustained pressure on the trigger point until it releases. If you discover the nodule within the taut band of tissue, you hold pressure on that until the pressure starts to decrease. This could take from thirty seconds to several minutes. If the trigger point is chronic, then it’s going to take multiple sessions to release this pain. You’ll do this with the ball to help to release the trigger point. This method is additionally called ischemic pressure.
Precaution of trigger point therapy: Persons with infectious diseases, open sores, and/or recent injuries should wait until they need to recover before beginning trigger point therapy. The person taking anticoagulant pharmaceuticals may experience bruising after trigger point therapy.
Dry needling
The dry needling technique is one of all of the fastest ways to inactivate scalene myofascial trigger points. Dry needling, during which the doctor will insert a skinny needle directly into and around your trigger point, move it around, and poke it in and out. The dry needling technique involves inserting a needle into several places in and around the trigger point. It will be quite painful and helps chop up muscle tension, but it’s one of the foremost effective ways to inactivate a trigger point and reduce the pain. Acupuncture also appears to be helpful for some folks that have scalene myofascial pain syndrome. Some therapists use acupuncture needles, which are smaller and less painful than hypodermic needles. There are some differences between dry needling and acupuncture. Pushing thin needles into the trigger point to scale back tightness, increase blood flow and relieve pain. A scientific review concluded that dry needling for the treatment of this pain syndrome within the lower back gave the impression of being a useful adjunct to straightforward therapies, but that clear recommendation couldn’t be made because the published studies were small and of inferiority.
Wet needling/trigger point injections
Trigger point injections are like dry needling. Typically, doctors use a needle to inject saline or a neighborhood anesthetic like lidocaine into the trigger point to alleviate pain. The consequences are compared to dry needling, but the procedure may cause less discomfort and trigger point injections with steroids are also an option. Wet needling, also called trigger point injections, is the same as dry needling apart from the doctor simultaneously injecting a numbing agent or steroid.
Stretching techniques (e.g. spray and stretching)
A physiotherapist may lead you thru gentle stretching exercises to help ease the pain in your affected side of the muscle. If you are feeling trigger point pain when stretching, the physiotherapist may spray a numbing solution on the skin. Stretching helps many of us with myofascial pain syndrome. Some physiotherapists apply a chilly, numbing spray to the muscle area before leading someone through stretches. There are some gentle stretches and exercises. You’ll try reception to decrease pain.
“Stretch and spray” technique: this system involves spraying a muscle and a trigger point with a coolant and then slowly, manually stretching the muscle.
Heat: Heat applied via a hot pack or a hot shower, can help to relieve muscle tension and reduce or decrease pain.
Posture training
It improves posture and can help to relieve myofascial pain, particularly in the neck muscles. Exercises that strengthen the muscles surrounding your trigger point will help you prevent overworking your muscles.
Many physical and manual therapy techniques, such as:
- Post-isometric relaxation
- Active Release Techniques
- Trigger point pressure release
- Muscle energy techniques
Other treatment options include:
- Dietary changes to scale back inflammation and stop ingredients that appear to trigger pain
- Hot Pack / Cold pack
- Behavior modification like exercise, posture, workstation setup, yoga, meditation, sleep habits, etc.
- Physiotherapy, including steps to realign posture, as needed
- Acupuncture
Exercise for Scalene Syndrome
While sitting straight on a chair, grab hold of the seat with one hand. Hold on to your head with the opposite hand as you pull your head towards the pulling hand. Turn your head backward to figure the anterior scalenes muscle, straight to figure the center, and downwards to figure the posterior scalenes muscle.

Posterior Scalene stretch:
Sit forward on the sting of a chair, with the chest up. Hold the seat of the chair tightly with one hand to stay the ribs down. Side flex your head to the other side without flexing your head forward. Rotate the head slightly toward the hand-holding chair and slightly extend the neck to induce more of a stretch.

Anterior scalene stretch:
Keep your head squarely over your shoulders and your back straight. Slowly turn your head to the correct one until you are feeling a stretch within the side of your neck and shoulder. Hold the stretch for 15-30 seconds, so slowly turn your head forward again. Repeat on your left side.
Medial scalene stretch:
Keep your head bent over your shoulders and keep your back straight. Slowly turn your head to the right until you’re feeling a stretch within the side of your neck and shoulder. Hold it for 15-30 seconds, and then slowly turn your head forward again. Repeat on your left side.
Scalene PNF strengthening:
To strengthen scalene sits in a comfortable chair. Place the palm of your hand on the correct side of your head. This hand acts as a stabilizer within the exercise. Begin to maneuver your right ear toward your right shoulder while maintaining the resistance provided by your hand. Repeat 8 to 10 times on either side.
By strengthening the striated muscle you’ll increase your ability to stabilize your cervical spine, which reduces the danger of a future injury.
Strengthen the scalene exercise #2
Sit or get up straight with a resistance band looped around your head. Hold the ends of the band firmly to at least one side ensuring there’s some tension within the band. Pull the bar far away from your head, resisting the movement by keeping your head in a very neutral position. hold this position, relax and repeat.
Massage variation for anterior scalene:
This self-massage for the scalene is another good way to alleviate pain around the collarbone and deep inside the highest of the shoulder.
If you get arm numbness while sleeping or while your arm is overhead, this is often how for you to cut back that tingling down the arm.
Massage this muscle for 30-90 seconds in various spots, starting by pressing down right behind the collarbone and dealing up the side of the neck.
Make sure to stay your posture upright, reaching the highest of your head to the ceiling, and pulling both of your shoulders DOWN.
While pushing on the scalene along with your fingers, take a deep breath, then side bends the top while exhaling.
You do not have to slide your fingers on your skin. If you do, use some lotion to permit the fingers to glide. you’re welcome to use tools just like the Theraband, a ball, a barbell, etc to urge into the neck, except for a fast massage while you’re on the go, just use your fingers!
Home advice
Treatments you’ll do reception include:
- Heat as in an exceeding heater. Some people enjoy cold/ice packs.
- Exercise. Specifically, weight-bearing exercises to strengthen muscles, stretching exercises to stretch muscles, and aerobic exercises to bring more oxygen into the muscles.
- Soaking in warm water.
- Massages.
- Over-the-counter painkillers like acetaminophen or NSAIDs like ibuprofen or naproxen. Don’t take these drugs if you’re taking analgesics or NSAIDs prescribed by your doctor.
- Relaxation techniques include decreasing stress, yoga to stretch, relaxing the muscles, breathing exercises, and meditation.
- Changes in diet and avoid foods that avoid causing inflammation.
- The duration of pain syndrome differs from person to person. With treatment, it should deviate after each day or some weeks, but it can take longer for some.
How fast this pain syndrome resolves depends on some factors, including
- your general health.
- Balance the diet and quality of sleep.
- Take care of yourself if you’ve got this pain syndrome.
- Self-care measures to require care of your body healthily may make it easier for you to give some thought to managing your pain.
- Try to Exercise: Gentle exercise can facilitate your coping and improve pain. When your pain allows you, get moving. Ask your doctor or physiotherapist about proper exercises.
- Relax: If you’re stressed and tense, you’ll experience increased pain. Find ways to relax.
- Meditating, talking with friends, or writing during a journal entry can all be helpful.
- Take care of your body.
- Eat a healthy diet of vegetables and fruits. Get enough sleep so you can rest.
- Confirm the body so that you will put your energy toward addressing your pain.
Prevention
How to prevent scalene myofascial pain syndrome?
Certain factors can put you more in danger of developing myofascial pain syndrome and managing these risk factors might not prevent you from developing the syndrome but could help reduce or diminish the severity of this condition.
Many of the avoidable suggestions to follow are also pain-manageable procedures:
- Maintain proper sleep hygiene.
- Reduce your stress.
- Get exercise.
- Prevent muscle injury. (this is an example of preventing muscle injury because the purse or purse you carry is too heavy).
- Practice relaxation methods.
- Eat a healthy diet, like the Mediterranean sea diet. Some foods result in inflammation and inflammation causes myofascial pain.
Some foods to avoid include:
- Fried foods (French fries, for example).
- Dairy (milk, cheese, yogurt).
- Refined carbohydrates and foods with refined flour like pizza, pasta, pastries, breadstuffs, and breakfast cereals.
- Margarine (butter), oil.
- Sugary foods and beverages like soft drinks.
- Red meat (burgers, steaks).
- Artificial lures and general additives (“no sugar added” products, zero-calorie “diet” soft drinks, and refined foods that include candy, ice cream, and fruit).
- Processed meat like hot dogs, and sausage.