Sandifer syndrome
Table of Contents
What is Sandifer syndrome?
- Sandifer syndrome (SS) is a type of movement disorder that is associated with acid reflux and sometimes a type of stomach hernia.
- Movements can range from bending in your back to tense neck postures.
- They normally happen right after eating.
- Sandifer syndrome was first noted in the early 1960s, and the precise number of cases is unknown. It is most often seen in infants and young children yet can also happen in teenagers and adults.
- It is an infrequent disorder that is found in less than 1% of cases of a related condition called gastroesophageal reflux disease (also known as GERD).
What are the symptoms of Sandifer syndrome?
Symptoms of Sandifer syndrome include:
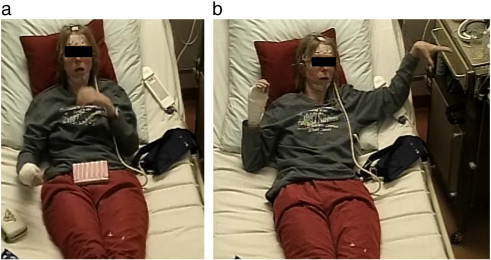
- Dystonic movement of the neck and back: These are involuntary muscle spasms that lead to repetitive and twisting movements. The spine can arch, bending your head toward your feet & twisting your neck to one side.
- Acid reflux: This is when stomach acid journey to your esophagus and throat and causes pain & damage.
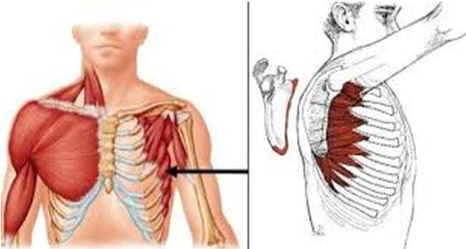
- Hiatal hernias: This is when the upper part of your stomach swells into your diaphragm.
- Vomiting: This is typically related to the same conditions that lead to acid reflux.
- Anemia: This condition occurs when your RBC count is low.
- Malnutrition: Severe reflux can make it hard to eat, and you may not get sufficient nutrients.
- Rumination: This occurs when you spit up your food and need to remasticate and swallow it.
- Abnormal eye movements: Episodes of the involuntary muscle spasms and reflux usually last between 1 and 3 minutes. They can happen more than 10 times a day.
The symptoms of Sandifer syndrome are often misidentified as other conditions, including:

- Infant spasms
- Epilepsy
- Seizures (an unknown neurological condition)
- Dystonia (a condition where the muscles spasm in a like way)
- These misidentify can be problematic because they can lead to a lot of unnecessary tests on your infant, including MRI and other imaging procedures.
- If your doctor misidentifies a condition like epilepsy, you run the risk of giving your child un-required medications. These medications can have their admit complications.
What are the causes of Sandifer syndrome?
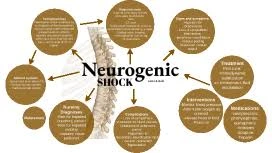
- Since Sandifer syndrome is seen in gastroesophageal reflux disease (GERD) patients, researchers were not sure at first if the neck and back spasms were causing the flow back or if the flow back was causing the back spasms. Current research indicates the latter— that the movements are your body’s attempt to relieve the pain from the stomach acid.
- The neck and back movements that distinguish Sandifer syndrome always seem to occur when the person’s throat is acidic from a lot of flow back.
- Some links have also been noticed between allergies to cow’s milk and Sandifer syndrome.
What is the diagnosis of this syndrome?
- Diagnosis is made on the basis of the association of gastroesophageal flow back with the characteristic movement disorder.
- Neurological examination is usually normal.
- Misidentifies as benign infantile spasms or epileptic seizures is common, particularly where clear signs or symptoms of gastroesophageal flow back are not apparent.
- Early diagnosis is critical, as treatment is simple and leads to cause resolution of the movement.
How is Sandifer syndrome treated?
- Treating Sandifer syndrome involves an attempt to reduce symptoms of gastroesophageal reflux disease (GERD).
- In many cases, you may just require to make some changes in feeding habits.
- These incorporate:
- not overfeeding,
- keeping your child honest for a half an hour after feeding,
- using a hydrolyzed protein formula if you are formula feeding or eliminating all dairy from your diet if you are breastfeeding because your doctor feels your child might have a milk protein sensitivity
- Mix up to 1 tablespoon of rice (wheat) for every 2 particles of formula in the baby bottle.
- If none of these changes work, your child’s doctor might propose medication, including:
- H2 receptor blockers, for example, ranitidine (Zantac).
- Ranitidine, brand name Zantac, is now marketed as Zantac 360, which contains a different active element (famotidine).
- Famotidine is in the same class as ranitidine and works the same way yet has not been found to contain intolerable levels of NDMA.
- antacids, for example, Tums
- proton pump inhibitors, like lansoprazole (Prevacid)
- Each of these medicines has potential side effects and may not always lessen symptoms.
- Ask your doctor about the risks versus goods of any recommended medicine for your baby.
- In rare cases, your child may require a surgical procedure called Nissen fundoplication.
- This precludes wrapping the top of the stomach around the lower esophagus.
- This tightens the lower esophagus, which impedes acid from coming up into the esophagus & causing pain.
- Treating the underlying cause of the symptoms: gastroesophageal reflux.
- These treatments may involve feeding and lifestyle changes, medications, and in infrequent circumstances, surgery.
- Your doctor will outline your options and will help you develop a safekeeping plan for your child.
- The Academy of American Pediatrics (AAP) has some helpful hints for managing gastroesophageal reflux.
- Feeding alter For Infants
- Hold your baby honest after feeding
- Belch your baby frequently
- Consider smaller, more recurrent meals so that your child has an easier time digesting
- Feeding Changes For toddlers/children
- Decrease fatty or fried foods
- Consider avoiding flow back triggers, like peppermint, caffeine, or tomato sauces
- Certain asthma medications may increase flow back symptoms; talk to your doctor about changing medications
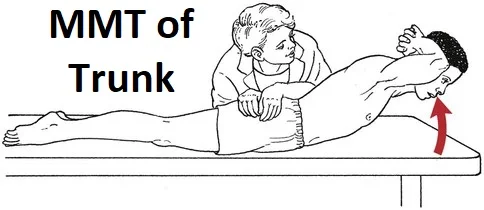
Physiotherapy treatment for dystonic movement of the back and neck:
- natural warm
- keyboard trays, mirrors
- swimming, cycling, walking
- yoga pose
- exercises for weak muscles
- advice for posture correcting
- foam roller
- balance training
- coordination exercise
- strengthening exercise
What is the prognosis of this syndrome?
- Sandifer syndrome is not typically life-threatening and the prognosis is typically good.