Posterior Tibial Tendon Dysfunction (PTTD)
Table of Contents
What is a Posterior Tibial Tendon Dysfunction?
Posterior Tibial Tendon Dysfunction (PTTD) is a condition that affects the posterior tibial tendon, which runs along the inside of the ankle and foot. The posterior tibial tendon plays a crucial role in supporting the arch of the foot and maintaining the foot’s stability during walking and other weight-bearing activities.
PTTD typically develops over time and is often caused by overuse, injury, or degeneration of the tendon. It can also be associated with certain risk factors such as obesity, diabetes, high blood pressure, and arthritis. As PTTD progresses, the tendon may become inflamed or even torn, leading to a gradual loss of arch support and a flattening of the foot.
Posterior tibial tendon dysfunction defect is the considerable specific cause of adult-acquired flatfoot deformation. Failure of the tendon involves surrounding ligamentous systems and will eventually lead to bony involvement and deformation.
PTTD is a materialized and debilitating disease, which can be detrimental to patients due to restrictions in mobility, significant discomfort, and weakness.
Tendon degeneration starts far before the clinical disease is apparent. First detection of PTTD may control operative means of restoration; if left to progress, surgical reconstruction with osteotomy and arthrodesis evolves necessarily
Risk factors for the condition have hypertension, obesity, diabetes, previous trauma, or steroid exposure.
Posterior tibial tendon dysfunction is a developed condition that can be categorized into four stages
In the early phases, there may be pain, the area may be red, warm, and swollen. There are not usually signs during gait but signs may be present in running.
The tendon has degenerated considerably and arthritis usually grows in the foot. In more extreme cases, arthritis may also develop in the ankle.

Clinically Relevant Anatomy
The Tibialis posterior arises from the posterolateral tibia, posteromedial fibula, and interosseous membrane.
It runs through the deep posterior compartment of the leg and its tendon passes after the medial malleolus.
Blood supply to the tendon is the most lacking in this area and is the most common site for a break.
Close to its insertion area, the tendon splits into a leading, plantar, and recurrent feature, with the main component inserting into the navicular tuberosity, the plantar portion onto the second, third, and fourth metatarsals, second and third cuneiforms and cuboid. The recurrent element attaches to the sustentaculum tali of the calcaneus.
The principal inverter of the midfoot and key dynamic stabilizer of the medial longitudinal arch is the tibialis posterior muscles.
Its contraction also promotes the medial longitudinal arch, causing the hindfoot and midfoot to evolve a solid structure. This allows the gastrocnemius to work with greater efficiency during the gait cycle
If compromised, a consequent pes planus foot may originate and place greater stress on the surrounding ligaments and soft tissue.
Causes of Posterior Tibial Tendon Dysfunction
Researchers have suggested numerous mechanisms for the deterioration of the posterior tibial tendon.
- Repetitive loading creating microtrauma and developed failure is the most prevalent cause of PTT worsening.
- A retromalleolar, hypovascular area does exist and may also donate to the disease.
- The posterior tibial tendon does make an acute turn around the medial malleolus, placing a significant amount of tension on the tendon in the region distal and posterior to the medial malleolus (the adjacent tendons of the flexor hallucis longus and the flexor digitorum longus do not accept this sharp turn). This anatomical study of the tendon is also likely a contributing factor.
- Other explanations include restriction beneath the flexor retinaculum, aberrant talus architecture, osteoarthritis-related degenerative changes, and preexisting pes planus.
Epidemiology
The overall incidence of this disorder, it is thought that the prevalence is anywhere from 3.3 to 10%, depending on the sex and age of the patient.
The real prevalence may be substantially greater than shown in the literature since PTTD is linked to adult-acquired flatfoot deformity, which makes it more likely that it will be misdiagnosed.
Up to 60% of persons have conditions including steroid usage, diabetes, hypertension, obesity, prior surgery, and foot or ankle damage.
Though many of these risk factors are generalized medical conditions, only one side is typically involved; the bilateral condition is rare
Risk factors to get PTTD are:
- Elderly: especially middle-aged females, with up to 10% majority in this group.
- Youthful athletes
- Hypertension
- Obesity
- Diabetes mellitus
- Seronegative arthropathies
- Supplement navicular bone
- Ligamentous laxity
- Pes planus (flatfeet)
- Steroid therapy
- Accessory navicular: may meddle with posterior tibial tendon function
- Overuse
- Previous trauma (certain types of ankle fracture)
- Steroid injections
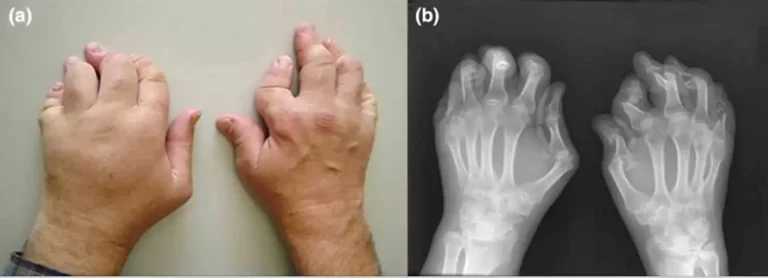
- Psoriatic arthritis / Rheumatoid arthritis
Symptoms of Posterior Tibial Tendon Dysfunction
Most patients convey a slow, insidious onset of unilateral flatfoot deformation.
A record of trauma may be current in up to 50% of cases.
Patients will describe their medial foot and ankle discomfort and edema, which may get worse with activity.
Standing on their toes may be discouraging and difficult, as may walk up or down stairs or on rough surfaces.
patients may complain of a worsening of a preexisting limp.
As the medial longitudinal arch collapses, the deformation of the foot increases; in this instance, patients may describe irregular wear on their shoes.
In some extreme cases of deformity, the distal fibula will come into connection with the calcaneus, and pain will drive to the lateral aspect of the foot; patients at this location may describe the sensation of stepping on the medial ankle.
The difference in static/dynamic foot ( pes planus)
Poor balance
Impaired MMT PF/IV
Difficulty/inability to complete unilateral heel raise. Limited calcaneal inversion upon ascent
Challenged subtalar mobility
Stages of PTTD
As per Johnson and Strom:
- Stage I: Posterior tibial tendon undamaged and inflamed, no deformation, mild node
- Stage II: Posterior tibial tendon dysfunctional, developed pes planus but passively correctable, commonly incapable to perform a heel raise
- Stage III: Degenerative modifications in the subtalar joint and the deformation is designated
- Stage IV ( Myerson): Valgus tilt of talus conducting to lateral tibiotalar deterioration
- Stage I
- Deformity: tenosynovitis
- Physical exam: single-leg toe raise test (+)
- Radiography: Normal
- Stage IIA
- Deformity: Flatfoot deformation, flexible hindfoot, normal forefoot
- Physical exam: single-leg heel raise (-), gentle sinus tarsi discomfort
- Radiography: Arch collapse deformation
- Stage IIB
- Deformity: Flatfoot deformation, flexible hindfoot/rearfoot, forefoot abduction
- Physical exam: Same stage IIA
- Radiography: same stage IIA
- Stage III
- Deformation in stage II becomes selected, rigid, or inflexible
- Deformation: flatfoot deformation, tough forefoot abduction, rigid hindfoot/rearfoot valgus
- Physical exam: extreme sinus tarsi pain, single-leg heel raise test (-)
- Radiography: arch collapse deformation(subtalar arthritis)
- Stage IV
- Deformity: flatfoot deformity, solid forefoot abduction, solid hindfoot/rearfoot valgus, deltoid ligament compromise
- Physical exam: single-leg heel raise test (-), painful sinus tarsi pain, ankle pain
- Radiography, arch collapse deformation, subtalar arthritis, talar tilt ankle mortise
Differential Diagnosis
Diagnoses recorded below can give very besides to PTTD and should merit reference during evaluation :
- Tarsal coalition
- Inflammatory arthritis
- Charcot arthropathy
- Neuromuscular disorder
- Traumatic disorder of midfoot ligaments
Diagnostic Procedures
Besides the clinical diagnosis, radiographic evaluation can be used to assess deformation and the possible presence of degenerative arthritis or other reasons for pes planus. MRI has the highest sensitivity, specificity, and precision, but ultrasound is less costly and almost as sensitive and specific as MRI.
Clinical tests for PTTD (more details in Examination):
- Too multiple toes sign
- Single-leg heel raise
- First metatarsal rise sign
- Plantar flexion and inversion of the foot against antagonism
- Mobility of TN and CC joints
- Weightbearing X-Rays
Examination
The examination can be based on past records.
Subjective
Before a clinical study is performed, the patient should be asked a series of queries to rule out other conditions. It is necessary to interpret PTTD in an before stage to prevent permanent deformations of the foot/ankle, a physical assessment is therefore essential.
Objective
The physiotherapist can palpate the posterior tibial tendon from beyond the medial malleolus to its insertion, to maintain the integrity and evaluate probable pain and swelling that are expected for the first phases of PTTD. In the later phases, the deformation can move and pes planus may be visual. The entire lower body should be examined, not just the foot, because the valgus in the knees might make the pes planus more obvious. The physiotherapist can select the severity of the pes planus by determining how many fingers can be passed underneath the midfoot.
special tests for PTTD/AAFD contain:
The too many toes sign: the foot should be examined from behind and above. The too many toes sign is a method of inspection from behind. It is based on how many toes you can see from rearward. An engaged foot will be more than one and a half to two toes see also Foot Posture Index
Double leg heel elevation: to go with both feet from a flatfoot posture to standing on the toes. Patients with stage I dysfunction can do this, but it’s discouraging. Patients with stage II, III, or IV dysfunction are incapable to do a heel raise. When a patient stands on tiptoes the heel of the involved foot will not bend inwards; the normal foot will stay into inversion while the concerned hindfoot will stay in valgus.
A single-leg heel raise: patients can’t do one heel raise with the involved foot;
The first metatarsal rise sign: the patient stands on both feet, and the shin of the involved foot is taken with a hand and rotated externally. When the patient has PTTD, the head of the metatarsal I am expanded, while normal metatarsal I stay on the ground;
Plantarflexion and inversion of the foot against opposition: test the tibialis posterior’s power.
Outcome Measures
Foot Function Index
5-Minute Walk Test
Tools to record kinematics from the tibia, calcaneus, and first metatarsal: e.g. Milwaukee Foot Model
Treatment of Posterior Tibial Tendon Dysfunction
Medical Treatment
A number of factors must be taken into consideration by the treating physician in order to determine whether patients require operational or non-operative therapy for their posterior tibial tendon dysfunction.
Non-invasive treatment, such as orthosis and physical treatment is preferable because they do not hurt healthy surrounding tissue, but only when non-operative treatment fails, surgical therapy is needed.
There is ample proof that persons with posterior tibial tendon impairment have a significantly reduced quality of life.
There is evidence that early conservative management can enhance pain, function, and disability quality of life.
All Stages initially:
Conservative management with NSAIDs and activity transformation. Also meant for non-surgical patients or low-demand, elderly age patients.
Stage 1:
For a conservative approach, the posterior tibial tendon may be immobilized in a walking boot for up to 3–4 weeks to allow for tendon repair as seen by eccentric strengthening during physical therapy.
If immobilization and physical treatment are thriving, transitioning into custom-molded orthotics or AFO is appropriate to support comfort. Emphasis on medial forefoot posting is necessary.
Conservative treatment should be for 3 to 4 months, and if it fails, then surgical intervention may be deserved. A tenosynovectomy, with tubularization, may be disclosed
Stage 2A:
Conservative immobilization and physical treatment with orthotics or ankle-foot orthosis (AFO) as indicated in stage 1
Surgical treatment affects medial calcaneal osteotomy with posterior tendon debridement and rehabilitation. The transfer of the flexor digitorum tendon (FDL), the rebuilding of the spring ligament, or the stretching of the Achilles tendon are all examples of ancillary methods.
Stage 2B:
All of the earlier listed systems in Stage 2A +/- lateral column lengthening, or confidential subtalar joint arthrodesis
Stage 3:
Conservative treatments, as noted above.
Surgical therapy is often deserved as it involves rearfoot arthritic transformations and a medial double arthrodesis or triple arthrodesis common (subtalar, calcaneocuboid, and talonavicular arthrodesis) is exhibited with or without deltoid ligament rehabilitation.
Stage 4
Conservative treatments, as mentioned above.
Surgical treatment is often required as it includes arthritic changes in the ankle, as well as rearfoot.
Important valgus alignment of the talus inside the ankle mortise requires a tibiotalocalcaneal (TTC) arthrodesis for the hindfoot.
Physical Therapy Treatment
The key to a successful result is early detection of the dysfunction and conventional control to prevent chronicity.
The goals of nonoperative treatment contain the
- Elimination of clinical signs,
- Advancement of hindfoot alignment, and the Prevention of developed foot deformity.
- Patient reeducation: Activity restriction and changeover
- Supplying relief through medications for medial arch support insoles or custom orthotics (necessary in many cases).
The first choice is conservative treatment, which includes physiotherapy and orthotics for Stage I and II. Options contain:
- To support the arch, use bracing or orthotic devices.
- The foot can be kept immobile with the use of a walking cast or CAM boot. If this provides relief, the patient can have orthotics, an ankle-foot orthosis (AFO), or shoe inserts or modifications installed.
- Stretching the Achilles tendon, strengthening the posterior tibialis, and exercising the posterior tibialis in concentric and eccentric motions. in addition to non-steroidal anti-inflammatory drugs
- Immobilization, such as a short-leg cast or boot, prevents the tendon from bearing any weight and enables it to recover.
- Non-steroidal anti-inflammatory medicines (NSAIDs), including ibuprofen, are medications that can be used to treat inflammation and discomfort.
- Shoe alterations: suggest adjustments like unique inserts used to enhance arch support.
- Exercise: Pick up little things with your toes, such as pebbles, marbles, or tiny toys, and drop them into a bucket.
- Caterpillar Exercise to Strengthen Your Arch To begin the caterpillar exercise to strengthen your arch, lie on your back with your knees bent and your feet flat on the ground, approximately two feet apart from your buttocks. Pull your toes back toward your heels while raising the arches of both feet. Arches should be relaxed, and feet should be moved backward toward the buttocks. Repeat the exercise while letting your feet move in a caterpillar fashion toward your glutes. Repeat the process in reverse, gently sliding your feet away from your buttocks in a caterpillar motion, until your feet are almost touching.
- Arch raises: Lie back in a chair with your feet flat on the floor and your knees bent at a 90-degree angle. With no heel lift or toe curl, raise the arch of one foot off the floor. (It’s more difficult than it seems!) When done correctly, your foot, lower leg, and thigh muscles should feel strained.
- Alphabet Writing: By picturing a pencil in between your toes, pointing the toes outward, and “writing” the alphabet in the air in front of you, you may strengthen your entire foot.
- A tendon synovectomy or debridement may be necessary after up to 4 months of nonoperative therapy if there has been no improvement.
- Orthotics:
- The most crucial element of treatment is optimizing foot loading control using foot orthoses and suitable footwear. Depending on the pathology’s evolution, semi-rigid ankle-foot orthoses, individualized foot orthoses, and over-the-counter non-individualized foot orthoses can all be used to manage the condition. Nonsurgical therapy should be considered for at least three to four months in stage I illnesses. For individuals with acute tenosynovitis, a brief walking cast or removable cast boot immobilization is recommended. After immobilization, if symptoms subside, the patient may be fitted with an ankle-foot orthosis (AFO) or a bespoke orthotic. The orthotic should be a complete contact insert that is full-length, semirigid, and has medial posting. The orthotic’s main job is to support the arch and treat the flexible aspect of the malformation.
Depending on whether there is an acute inflammation and if the foot deformity is stable or flexible, several treatment options are available for different phases of PTTD:
- Stage I: Chronic: flat shoes and corrective orthoses or ankle-foot orthoses, lace-up; Acute: 4–8 weeks of immobilization; RICE
- Stage II: RICE, 4–8 weeks of acute immobilization, lace-up, corrected orthosis, and flat footwear for chronic conditions.
- Stage III: Semirigid shoes with laces, personalized footwear, orthotics, and lace-up footwear
- Stage IV: Custom-made lace-up shoes or semi-rigid shoes with accommodating orthoses
Prognosis
Without therapy, posterior tibial tendon dysfunction is a progressive condition that will worsen with time.
Progression can be slowed down with early identification and management.
Custom orthotics and therapy have been demonstrated to significantly improve patients’ conditions.
In recent research, 89% of the patients with stage I and stage II PTTD responded to orthotics and physical therapy. By 4 months, almost all of these patients had recovered their full strength.
Surgery has far less predictable results, so a return to the pre-disease state shouldn’t be assumed. Patients who have had reconstructive surgery could still experience certain aftereffects.
Clinical conclusion
To get the best patient outcomes for PTTD, a multidisciplinary team approach involving doctors, specialists, physiotherapists, and pharmacists is necessary.
Usually a slow-onset ailment, posterior tibial tendon dysfunction primarily affects middle-aged, obese women.
Obesity, hypertension, diabetes, steroid usage, and seronegative arthropathies are risk factors.
Patients may express concerns about exacerbating an existing limp, medial ankle discomfort, edema, or mobility issues.
The tendon may be sensitive throughout its path, it may be difficult to elevate only one heel, or it may appear that the feet have “too many toes” when viewed from behind when standing.
MRIs and X-rays can help stage the illness, confirm the diagnosis, and aid in preoperative planning.
Although the condition as a whole is underdiagnosed and can be misdiagnosed in its early stages, quick treatment can avert deformity and the need for surgery.
FAQs
Most people may be corrected with braces and orthotics without undergoing surgery. Surgery can be a successful pain management option if orthotics and braces are ineffective. Surgery might consist of anything as straightforward as removing the inflammatory tissue or mending a small rip.
Early movement on a tendon that is mending might cause a setback in recovery, and posterior tibial tendon dysfunction typically improves after 6 to 8 weeks. Patients might become highly frustrated by non-compliance and the healing time can be doubled.
Heel lifts are the simplest exercise to begin tibialis posterior muscle training. You might want to begin performing exercises while seated on a chair, and as your muscular power increases, you might consider standing.
The discomfort associated with posterior tibial tendonitis in the foot and ankle can be eliminated with physical therapy. You can regain: this through physical treatment. Your foot’s and ankle’s typical range of motion. Strength
Your path to recovery might include physical therapy. The Achilles tendon, the biggest and most often damaged tendon in the body, is typically treated with physical therapy. Your therapist will create a strategy to address your unique objectives, difficulties, and requirements.






3 Comments