Pisiform Impingement Syndrome
Table of Contents
What is a Pisiform Impingement Syndrome?
Pisiform impingement syndrome, also known as pisotriquetral impingement syndrome, is a condition that affects the wrist and can lead to discomfort and pain. The bone is a small, pea-shaped bone located in the wrist, on the ulnar side of the hand (pinky finger side). It articulates with the triquetral bone and is part of the carpal bones that form the wrist joint.
In pisiform impingement syndrome, there is irritation or compression of the structures surrounding the pisiform bone, such as ligaments, tendons, and nerves. This can result from various factors, including repetitive wrist motions, overuse of the wrist, trauma to the wrist, or certain anatomical variations.
Pisiform impingement syndrome, also known as pisotriquetral syndrome, is a condition in which there is irritation or compression of the pisotriquetral bone and its surrounding structures, particularly the pisotriquetral joint.
Anatomy of pisiform impingement syndrome
Pisiform impingement syndrome, also known as pisotriquetral syndrome, involves irritation or compression of the pisotriquetral bone and surrounding structures, particularly the pisotriquetral joint. To better understand this condition, let’s look at the relevant anatomy:
Small bone:
The pisiform is a small sesamoid bone located on the ulnar (pinky) side of the wrist. It is located in the tendon of the ulnar Carpi ulnaris muscle and articulates with the palmar surface of the three-dimensional bone.
Pisotriquetral joint:
The Pisotriquetral joint is formed by the joint between the longitudinal bone and the tricuspid bone. This joint allows smooth movement and stability between the two bones, which contributes to the function of the wrist.
Flexor Carpi Ulnaris Tendon:
The flexor carpi ulnaris (FCU) is a wrist flexor muscle located on the elbow side of the forearm. Its tendon passes through the wrist and attaches to a long bone.
When impingement syndrome involves the pisiform, it is usually caused by repetitive motion or direct trauma to the wrist, causing inflammation and irritation in the area. Some possible anatomical factors that may contribute to pisiform impingement syndrome include:
A. Repetitive motion: Activities that involve repeated flexion and extension of the wrist can stress the shape of the wrist and surrounding structures, causing inflammation and attack.
B. Anatomical variations: Some people may have different bone shapes, sizes, or locations, or the surrounding bones and ligaments, which can increase the risk of impingement.
C. Tendon changes: Degenerative changes or inflammation in the knee flexor tendon can also contribute to compression of the petiole.
Causes of pisiformis impingement syndrome
Pisiform impingement syndrome, also known as pisotriquetral syndrome, is caused by irritation or compression of the pisotriquetral bone and its surrounding structures, particularly the pisotriquetral joint. Too many factors can lead to the development of this condition, such as:
Repetitive movements:
- Repetitive activities of bending and extending the wrist can stress the longitudinal region and adjacent structures, causing inflammation and attack.
- It is often seen in people who participate in sports or occupations that require repetitive wrist movements, such as gymnastics, weightlifting, or certain types of manual labor.
Trauma:
- A direct blow or injury to the wrist can damage the small bone or the surrounding soft tissues.
- Trauma can result from falls, sports-related injuries, or accidents that significantly affect the wrist joint.
Anatomical variations:
- Some people may have anatomical variations of a long bone or surrounding structures that make them more susceptible to momentum.
- For example, a smaller or incorrect bone shape or changes in the shape of the pisotricetral joint can increase the risk of impetuousness and anger.
Overuse or strain:
Overuse of the wrist, especially in activities that involve repetitive gripping or weight bearing, can cause strain on the longitudinal region, increasing the risk of impingement.
Inflammatory conditions:
Certain inflammatory conditions, such as arthritis or tenosynovitis, can cause swelling and inflammation around the small bone, leading to impingement.
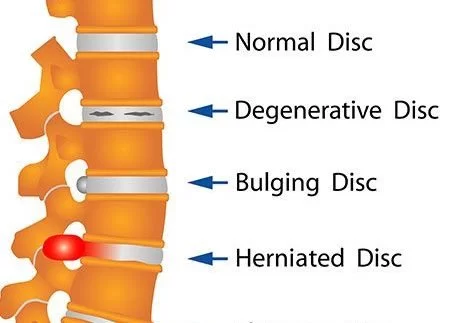
Degenerative changes:
Over time, wear and tear of the wrist joint can cause degenerative changes in the bones and soft tissues, contributing to impingement syndrome.
Wrist instability:
Wrist instability, often caused by ligament injuries or laxity, can change bone alignment and mechanics, which can lead to impingement.
Excessive pressure on the pisiform
Activities that involve direct pressure on the pisiform, such as using the palm of the hand as a weight-bearing support, can cause irritation and pressure.
It is important to note that pisiform impingement syndrome is relatively rare and its exact cause can vary from person to person. Correct diagnosis and treatment are essential to address any contributing factors to the condition. If you suspect that you may have pisiform impingement syndrome or persistent wrist pain and discomfort, it is important to see a qualified healthcare professional for a thorough evaluation and appropriate treatment.
Symptoms of pisiform impingement syndrome
Pisiform impingement syndrome, also known as pisotriquetral syndrome, can present with a variety of symptoms primarily centered around the pisiform bone and the structures surrounding the wrist. Symptoms can vary in intensity and worsen with activities involving wrist movements. Common symptoms of pisiform impingement syndrome include
Pain:
- Localized pain is a characteristic symptom of this condition.
- The pain is usually felt in the area of the small bone on the side of the ulna (pinky finger) of the wrist.
- The pain can be described as a dull ache or sharp discomfort and can vary in intensity.
Strain:
A strain can occur when pressure is applied to the long bone or the surrounding area.
Swelling:
Inflammation can occur around the wrist joint, resulting in swelling and sometimes a visible lump in the affected area.
Painful wrist movements:
Certain wrist movements, especially bending and extending the wrist, can make the pain worse. Activities that involve repetitive or forceful wrist movements may worsen symptoms.
Poor grip strength:
Prolonged impact can weaken the grip, making tasks that require a strong grip more difficult.
Limited range of motion:
The wrist range may be reduced due to pain and discomfort.
Painful palpation:
When the doctor examines the wrist and especially presses the pisiform area, it can be painful and repeat symptoms.
Sensory changes:
In some cases, a small stroke can cause tingling or numbness in the hands, especially in the pinky and ring fingers, although this is less common than other symptoms.
Sensory Changes:
In some cases, pisiform impingement may cause tingling or numbness in the hand, particularly in the pinky finger and the ring finger, though this is less common than other symptoms.
- It’s important to note that these symptoms can also be associated with other wrist and hand conditions, so a proper diagnosis is crucial.
- If you experience persistent wrist pain or any of the symptoms mentioned above, it’s recommended to consult a healthcare professional for a thorough evaluation.
- A qualified medical practitioner can conduct a physical examination, review your medical history, and may order imaging tests (such as X-rays or MRI) to accurately diagnose pisiform impingement syndrome and formulate an appropriate treatment plan to alleviate the symptoms and address the underlying cause.
Epidemiology of pisiform impingement syndrome
This condition is relatively uncommon, and research on its prevalence and incidence is limited compared to more well-known wrist and hand conditions.
- Pisiform impingement syndrome is considered a rare or rare-like condition, meaning that it is not frequently encountered in clinical practice compared to more common wrist disorders like carpal tunnel syndrome or wrist fractures.
- It is often underdiagnosed or misdiagnosed due to its rarity and similarity in symptoms with other wrist conditions.
- The scarcity of epidemiological data on pisiform impingement syndrome makes it challenging to provide precise figures on its prevalence and incidence.
- However, it is generally considered to be an infrequent condition that may affect a small percentage of individuals with wrist pain or related symptoms.
- Risk factors for developing pisiform impingement syndrome may include participation in certain sports or activities involving repetitive wrist movements, occupations with repetitive wrist strain, wrist trauma, and anatomical variations in the wrist structures.
- We recommend consulting medical databases, and research publications, or seeking guidance from healthcare professionals who stay up-to-date with the latest medical literature.
Diagnosis of pisiform impingement syndrome
The diagnosis of pisiform impingement syndrome, also known as pisotriquetral syndrome, involves a comprehensive evaluation by a healthcare professional. The process typically includes a combination of the following:
Medical History:
- The doctor will begin by discussing your symptoms and medical history.
- They may inquire about any recent injuries, activities that involve repetitive wrist movements, and any previous wrist or hand conditions.
Physical Examination:
- A thorough physical examination of the wrist and hand will be performed to assess for signs of inflammation, tenderness, swelling, and limited range of motion.
- The healthcare professional will also palpate the pisiform bone and surrounding structures to check for pain and sensitivity.
Provocative Tests:
- The doctor may perform specific tests to reproduce or exacerbate the symptoms.
- For example, they may apply pressure on the pisiform bone or manipulate the wrist to see if it causes pain or discomfort.
Imaging Studies:
- X-rays may be ordered to assess the bones and rule out other wrist-related conditions.
- While X-rays are not always helpful in diagnosing soft tissue problems, they can identify any bone abnormalities or fractures that may contribute to the symptoms.
Magnetic Resonance Imaging (MRI):
- If necessary, an MRI may be recommended to provide more detailed images of the soft tissues around the wrist, including tendons, ligaments, and the pisotriquetral joint. An MRI can help detect inflammation, swelling, or structural abnormalities.
Ultrasound:
- Ultrasound imaging can also be used to evaluate the soft tissues around the wrist, and it may provide valuable information about inflammation and fluid accumulation.
Nerve Conduction Studies (NCS) and Electromyography (EMG):
- In some cases, nerve conduction studies and electromyography may be conducted to assess nerve function and rule out nerve-related conditions that may mimic the symptoms of pisiform impingement syndrome.
Differential Diagnosis:
The healthcare professional will consider other possible causes of wrist pain and symptoms to rule out conditions like carpal tunnel syndrome, wrist fractures, or other wrist ligament injuries.
- Diagnosing pisiform impingement syndrome can be challenging due to its rarity and similarity to other wrist conditions.
- Therefore, it’s crucial to consult with a qualified healthcare professional with experience in hand and wrist disorders.
- They can accurately diagnose the condition based on a combination of clinical evaluation and imaging studies, and they will recommend an appropriate treatment plan to address the specific underlying cause and alleviate symptoms.
- When evaluating a patient with symptoms suggestive of pisiform impingement syndrome, a healthcare professional will consider various other conditions that can present with similar symptoms.
- Differential diagnosis involves distinguishing between these different conditions to accurately identify the underlying cause of wrist pain and related symptoms.
- Some of the main conditions that may be considered in the differential diagnosis of pisiform impingement syndrome include:
Carpal Tunnel Syndrome:
- Carpal tunnel syndrome is a usual deformity that happens because of compression of the median nerve as it passes through the carpal tunnel in the wrist.
- It can cause pain, tingling, and numbness in the thumb, index finger, middle finger, and part of the ring finger.
- It can sometimes be mistaken for pisiform impingement syndrome due to overlapping symptoms, such as wrist pain and discomfort.
Triangular Fibrocartilage Complex (TFCC) Tear:
- The TFCC is a cartilage structure in the wrist that stabilizes the ulnar side.
- Tears or injuries to the TFCC can cause pain on the ulnar side of the wrist, which may be similar to pisiform impingement syndrome.
Wrist Fractures:
- Fractures of the wrist bones, such as the scaphoid or triquetrum, can cause pain and swelling in the wrist, resembling symptoms of pisiform impingement syndrome.
Ulnar Tunnel Syndrome:
- Ulnar tunnel syndrome occurs when the ulnar nerve is compressed at the wrist, leading to pain, tingling, and weakness in the pinky finger and part of the ring finger.
- It can sometimes be mistaken for pisiform impingement syndrome, especially if the pisiform area is involved in compression.
Wrist Tendonitis:
- Inflammation of the wrist tendons, including the flexor and extensor tendons, can cause pain and discomfort in the wrist, which may be similar to pisiform impingement syndrome.
Wrist Arthritis:
- Various forms of wrist arthritis, such as osteoarthritis or rheumatoid arthritis, can cause joint pain, swelling, and stiffness in the wrist joint, overlapping with some symptoms of pisiform impingement syndrome.
Ganglion Cyst:
Ganglion cysts are noncancerous lumps that can develop on the wrist and hand. They can cause pain and may be mistaken for other wrist conditions.
Intersection Syndrome:
Intersection syndrome is an inflammation of the tendons at the intersection of the forearm muscles, which can cause wrist pain and may have symptoms that overlap with pisiform impingement syndrome.
De Quervain’s Tenosynovitis:
- De Quervain’s tenosynovitis is a condition that involves inflammation of the tendons on the thumb side of the wrist, leading to pain and swelling in the wrist and thumb area.
Properly diagnosing pisiform impingement syndrome involves a careful assessment of the patient’s medical history, physical examination, and appropriate imaging studies to rule out other conditions and arrive at an accurate diagnosis. If you are experiencing wrist pain or related symptoms, it is essential to seek evaluation from a qualified healthcare professional for an accurate diagnosis and appropriate treatment.
Medical treatment of Pisiform impingement syndrome
The medical treatment of pisiform impingement syndrome typically involves conservative measures aimed at relieving pain, reducing inflammation, and promoting healing. In most cases, surgery is not necessary, and symptoms can be effectively managed with non-invasive approaches. The specific treatment plan may vary based on the severity of the symptoms and individual patient factors. Here are some common medical treatments for pisiform impingement syndrome:
Rest:
Avoiding activities that aggravate the symptoms is essential to allow the wrist to heal. Resting the affected wrist can help reduce irritation and inflammation around the pisiform bone.
Immobilization:
- Wearing a wrist splint or brace can provide support and stabilize the wrist, preventing excessive movement that could worsen the impingement.
- The splint is usually worn for a few weeks or as recommended by the healthcare professional.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs):
- Over-the-counter NSAIDs, such as ibuprofen or naproxen, may be prescribed to reduce pain and inflammation.
- However, it is essential to use these medications as directed and consult a healthcare professional if there are any contraindications or concerns.
Ice Application:
Several times a day, apply ice to the affected area for 15-20 minutes to relieve pain and reduce swelling.
Physical Therapy:
- A physical therapist may be involved in the treatment plan.
- They can provide exercises to strengthen the wrist and forearm muscles and improve flexibility.
- Physical therapy can also focus on correcting any underlying biomechanical issues that may contribute to the impingement.
Corticosteroid Injections:
- In some cases, a healthcare professional may administer a corticosteroid injection into the pisotriquetral joint to reduce inflammation and alleviate symptoms.
Ultrasound Therapy:
Therapeutic ultrasound may be used to promote healing and reduce inflammation around the pisiform area.
Extracorporeal Shockwave Therapy (ESWT):
ESWT is a non-invasive treatment that uses shockwaves to stimulate the body’s healing process and may be considered in some cases.
Ergonomic Modifications:
If the impingement is related to specific occupational or sports activities, making ergonomic modifications to reduce strain on the wrist may be helpful.
- It is necessary to note that the effectiveness of these treatments can differ from person to person.
- Some individuals may find relief with conservative measures alone, while others may require a combination of therapies.
- If conservative treatments do not provide significant improvement, or if the condition is severe and impacting daily activities, surgery to release the impinged structures around the pisiform may be considered as a last resort.
- Always meet a qualified doctor for an accurate diagnosis and personalized treatment plan tailored to the specific condition.
Physiotherapy treatment in Pisiform impingement syndrome
Physiotherapy plays a crucial role in the management of pisiform impingement syndrome. A skilled physiotherapist can design a comprehensive treatment plan to address the underlying causes, reduce pain, improve wrist function, and prevent recurrence. The following are some common physiotherapy treatments for pisiform impingement syndrome:
Manual Therapy:
Physiotherapists may use various manual techniques to mobilize and manipulate the wrist joint and surrounding soft tissues. Manual therapy can help reduce stiffness, improve joint mobility, and alleviate pain.
Therapeutic Exercises:
- Specific exercises are prescribed to strengthen the muscles of the wrist, forearm, and hand.
- Strengthening these muscles can improve wrist stability and support the pisiform bone, reducing impingement.
- Common exercises include wrist flexion and extension, wrist pronation and supination, grip strengthening exercises, and forearm exercises.
- Performing basic range of motion exercises for the wrist, forearm, and hand can help maintain flexibility, reduce stiffness, and improve overall function.
- It’s essential to warm up before starting any exercises.
- You can warm up by gently moving your wrist, forearm, and fingers in various directions or by using a warm compress on the area.
- Remember to perform these exercises in a pain-free range and stop immediately if you experience any pain or discomfort.
- Below given are some basic range of motion exercises:
Wrist Flexion and Extension:
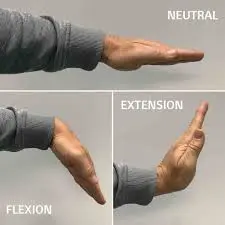
- Start with your forearm resting on a table or your thigh, palm facing down.
- Slowly bend your wrist upward (toward the ceiling) as far as you can comfortably go.
- Hold the position briefly and then slowly lower your wrist back down.
- Repeat this movement 10-15 times.
Wrist Radial and Ulnar Deviation:
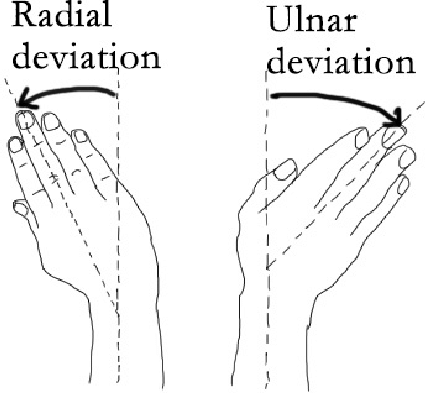
- Start with your forearm resting on a table or your thigh, palm facing down.
- For radial deviation, move your wrist sideways, so your thumb moves toward your forearm’s inner side.
- For ulnar deviation, move your wrist sideways, so your little finger moves toward your forearm’s outer side.
- Perform 10-15 repetitions for each direction.
Wrist Circles:
- Extend your arm forward, palm facing down.
- Gently make circular motions with your wrist, moving it clockwise for a few rotations and then counterclockwise.
- Perform 5-10 circles in each direction.
Forearm Pronation and Supination:
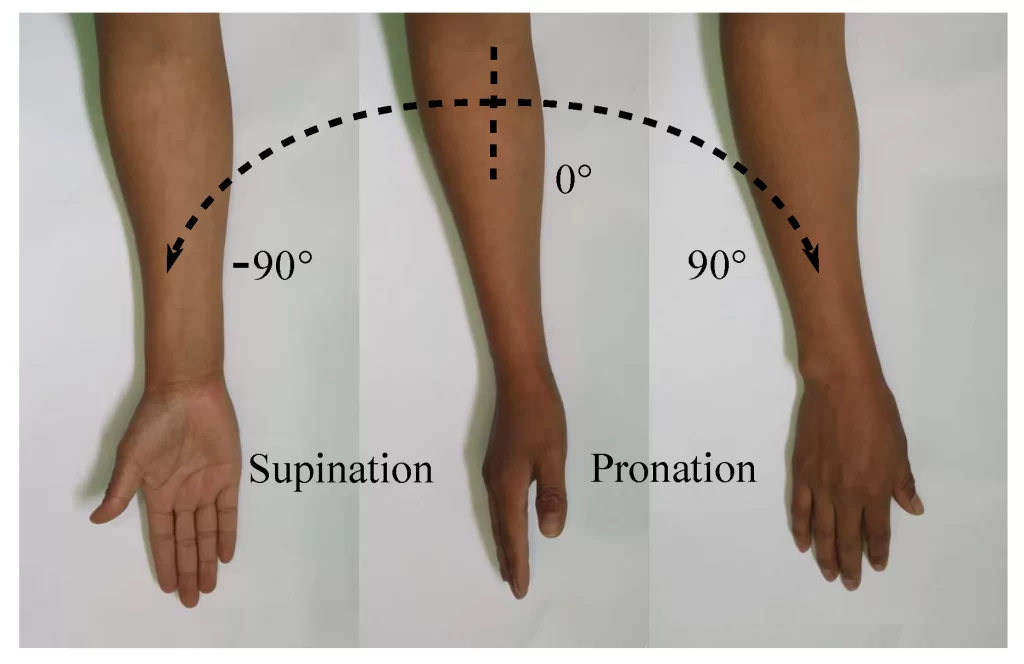
- Sit or stand with your elbow bent at a 90-degree angle, forearm resting on a table or your thigh, palm facing down.
- Rotate your forearm to turn your palm up (supination) and then back to palm down (pronation).
- Repeat this movement 10-15 times.
Finger Flexion and Extension:
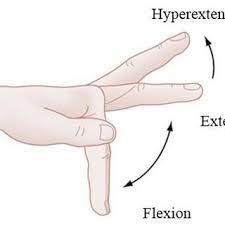
- Start with your hand open and your fingers straight.
- Slowly curl your fingers into a fist, bringing your fingertips to touch the base of your fingers.
- Then, open the hand and spread the fingers as wide as possible.
- Repeat this movement 10-15 times.
Finger Abduction and Adduction:
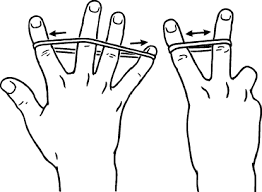
- Keep your fingers together and extended.
- Spread your fingers apart as far as you can (abduction) and then bring them back together (adduction).
- Perform 10-15 repetitions.
Remember to perform these exercises slowly and with control. Do not force any movement that causes pain or discomfort. If you have any pre-existing conditions or injuries, it’s best to consult a healthcare professional, such as a physical therapist or an occupational therapist, to make that these motions are safe and appropriate for your specific needs.
Stretching Exercises:
- Stretching is essential to improve flexibility and range of motion in the wrist joint.
- A physiotherapist may recommend gentle stretching exercises to increase the suppleness of the wrist muscles and ligaments.
- Stretching the wrist muscles and ligaments can help improve flexibility, reduce stiffness, and alleviate discomfort. It’s important to perform these stretches gently and gradually, without forcing any movement.
- If you experience pain or have a wrist injury, it’s essential to consult with a healthcare professional before attempting these stretches. Here are some effective wrist stretching exercises:
Wrist Flexor Stretch:
- With the palm up, extend the arm forward.
- With the other hand, slowly grasp the fingers and pull them back towards the body.
- A person should experience a stretch in the underside of the wrist and forearm.
- Maintain the stretch for 15-30 seconds and repeat 2-3 times on each hand.
Wrist Extensor Stretch:

- Extend the arm forward with your palm facing down.
- Use your other hand to gently push your hand and fingers down towards the floor.
- You should feel a stretch on the top of your wrist and forearm.
- Maintain the stretch for 10-15 seconds and repeat 2-3 times on both hands.
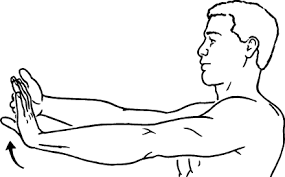
Wrist Flexor and Extensor Stretch:
- Extend both arms forward with the palms facing each other and fingers pointing up.
- Gently press your palms together and lower your hands towards the floor, keeping your fingers pointing upward.
- You should feel a stretch on both sides of your wrists and forearms.
- Maintain the stretch for 10-20 seconds and repeat 2-3 times.
Wrist Pronation and Supination Stretch:

- Extend your arm forward, palm facing down.
- With your other hand, gently rotate your hand and forearm to turn your palm up (supination) and then back to palm down (pronation).
- Hold the end position of each rotation for 5-10 seconds and repeat 5-10 times in each direction.
Prayer Stretch:

- Bring the palms together in front of the chest, with the fingers pointing upward.
- Gently lower the hands towards the waist while keeping the palms pressed together.
- Your wrists and forearms need should feel stretched.
- Maintain the stretch for 10-20 seconds and repeat 2-3 times.
Finger and Thumb Stretch:

- Extend the arm forward with the palm facing bottom side.
- Gently pull each finger and thumb back one at a time, feeling a stretch in the fingers and hand.
- Hold each stretch for a few seconds and repeat for all fingers and thumbs on both hands.
- Remember to perform these stretches with slow and controlled movements.
- Avoid bouncing or jerking, as it may cause injury.
- If you have any concerns about your wrist health or experience persistent pain, it’s crucial to seek advice from a healthcare professional, such as a physical therapist or an occupational therapist, for proper evaluation and personalized guidance.
Nerve Gliding Exercises:
If there is any involvement of nerve compression, nerve gliding exercises may be incorporated to mobilize the nerves gently and reduce irritation.
- Nerve gliding exercises, also known as neural gliding or nerve flossing exercises, are designed to improve the mobility and flexibility of nerves, reducing tension and irritation.
- These exercises can be beneficial for people experiencing symptoms like tingling, numbness, or shooting pain due to nerve compression or entrapment in the wrist and hand area.
- Before attempting nerve gliding exercises, it’s essential to consult with a healthcare professional, as these exercises may not be suitable for everyone, especially in certain medical conditions.
- Here are some nerve-gliding exercises for the wrist:
Median Nerve Gliding Exercise:
- Begin by sitting or standing with the back straight.
- Extend the involved arm in front of you, with the palm facing down.
- Begin by flexing your wrist and fingers down towards the floor, like you’re making a “stop” gesture with your hand.
- Next, slowly extend your wrist and fingers back up, as if you’re signaling someone to “come here.”
- Perform this gliding motion smoothly and continuously for 10-15 repetitions.
Ulnar Nerve Gliding Exercise:
- Sit or stand with your back straight.
- Extend your affected arm out to your side at shoulder level, with your palm facing up.
- Bend your elbow slightly and keep it in that position throughout the exercise.
- Begin by moving your wrist, fingers, and thumb in a claw-like motion, curling them down towards the floor.
- Then, extend your wrist, fingers, and thumb back up, spreading them wide.
- Repeat this gliding motion for 10-15 repetitions.
Radial Nerve Gliding Exercise:
- Sit or stand with your back straight.
- Your injured arm should be extended in front of you, palm upward.
- Keep your elbow straight throughout the exercise.
- Begin by moving your wrist, fingers, and thumb downward, bending your wrist like you’re pouring out a drink from a jug.
- Next, extend your wrist, fingers, and thumb back up, like you’re carrying a tray.
- Perform this gliding motion for 10-15 repetitions.
- During these exercises, it’s crucial to move gently and avoid any movement that causes pain or discomfort.
- If you experience worsening symptoms or if nerve gliding exercises exacerbate your condition, stop immediately and seek guidance from a healthcare professional.
- Remember, nerve gliding exercises are just one component of a comprehensive treatment plan.
- If you’re experiencing persistent wrist or hand issues, it’s important to consult with a qualified healthcare provider, such as a physical therapist or an occupational therapist, to receive a proper diagnosis and individualized treatment program.
Ultrasound and Electrical Stimulation:
Therapeutic modalities like ultrasound and electrical stimulation may be used to promote tissue healing, reduce inflammation, and alleviate pain in the affected area.
Taping and Bracing:
The physiotherapist may apply kinesiology tape or recommend wrist braces to provide additional support and stabilize the wrist during activities. This can help reduce strain on the pisiform bone and surrounding structures.
Activity Modification:
The physiotherapist will advise on modifying daily activities and work-related tasks to prevent exacerbation of symptoms. Proper ergonomics and wrist positioning are essential in reducing strain on the wrist.
Education and Self-Management:
Physiotherapy includes educating the patient about the condition, its causes, and strategies for self-management. This may involve teaching proper posture, wrist exercises, and techniques to avoid aggravating activities.
Home Exercise Program:
A tailored home exercise program will be provided to the patient to continue rehabilitation between physiotherapy sessions and maintain progress.
- The treatment duration and frequency of physiotherapy sessions will depend on the severity of the condition and the individual’s response to treatment.
- It’s important for patients to actively participate in the prescribed exercises and follow the physiotherapist’s recommendations to achieve the best outcomes.
- If conservative physiotherapy treatments do not provide sufficient relief, or if the condition is severe and persistent, the physiotherapist may collaborate with other healthcare professionals, such as orthopedic specialists, to explore other treatment options, including possible surgical intervention.
FAQ
Chronic pain in the pisiform region can be caused by tendinitis of the elbow flexor of the carpo-ulnar, fractures, or osteoarthritis of the pisotriquetral joint, which is degenerative arthritis of the wrist joint after scaphotrapezoidal osteoarthritis.
The pisiform is one of the eight and smallest carpal bones that make up the carpal joint. It is a small pea-shaped bone. it develops in the tendon and is a sesamoid bone.
Function Recovery from this procedure should be relatively quick, but it can take up to 6 months before you can rest your hand firmly on the heel. You should be able to drive in 3-4 weeks if you feel comfortable. The time to return to work depends on your profession and is worth discussing.
The radial edge has a hamate hook and the medial edge has a petiole with a pisohamate ligament. The ulnar nerve and artery access within this canal. The ulnar nerve joins the canal as a diverse sensory and motor nerve.
The clinical diagnosis of long-term dislocation usually depends on the mechanism of injury and pain, swelling and tenderness in the ulnar part of the wrist. Our patient presented with pain, swelling, and tenderness in the dorsomedial aspect of the wrist.