OSTEOGENESIS IMPERFECTA
Table of Contents
DEFINATION :
- Osteogenesis imperfecta (OI) is a rare genetic disorder of the synthesis of collagen that affects bone and connective tissue that can also be referred to as brittle bone disease. OI can occur by both inheritance and spontaneous genetic mutation andhas been linked to over 150 genetic mutations that all take effect on the genes COL1A1 and COL1A2. These are the genes that make up type I collagen.
- The mutation can either cause collagen production that is too low, or cause abnormal polypeptide chains that are unable to properly form type I collagen. There are four primary types of osteogenesis imperfecta that are described by the Sillence Classification of Osteogenesis Imperfecta.
CLASSIFICATION of OSTEOGENESIS IMPERFECTA :
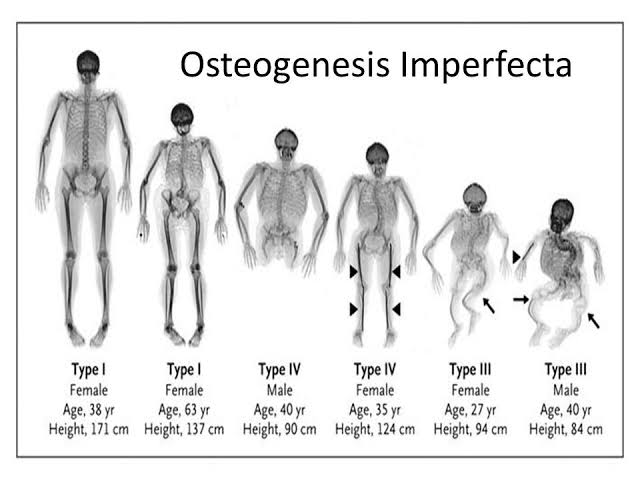
1.) type I
- Mildest form of OI
- Mild to moderate fragility without deformity
- Most fractures occur before puberty
- Associated with blue sclerae, triangular face, hearing loss (beginning in twenties or thirties), easy bruising
2.) Type II
- Most severe form of OI (perinatal lethal)
- Stillbirth or death during infancy or early childhood
- Extreme fragility of connective tissue
- Multiple in utero fractures
- Usually intrauterine growth retardation
- Severe bone deformity
- Soft, large cranium
- Micromelia: long bones crumpled and bowed; ribs beaded
3.) Type III
- Moderately Severe
- Progressive deformities
- Scoliosis
- Triangular face, large skull
- Severe osteoporosis
- Severe fragility of bones; usually in utero fractures
- Fractures heal with deformity and bowing
- Associated with tinted sclerae (blue, purple, or grey)
- Extremely short stature
- Usually wheelchair bound by teenage years
- This picture of the Wyse family is included courtesy of the Agape
- Family Life House website agapeflh.org.
4.) Type IV
Variable but usually milder course; normal or near-normal lifespan
Mild to moderate skeletal fragility and osteoporosis (more severe than type I)
- Associated with bowing of long bones
- Barrel-shaped rib cage
- Bones fracture easily before puberty; some children improve at puberty
- Light or normal sclerae; may or may not have moderately short stature and joint hyperextensibility”
CAUSE OF OSTEOGENESIS IMPERFECTA :-
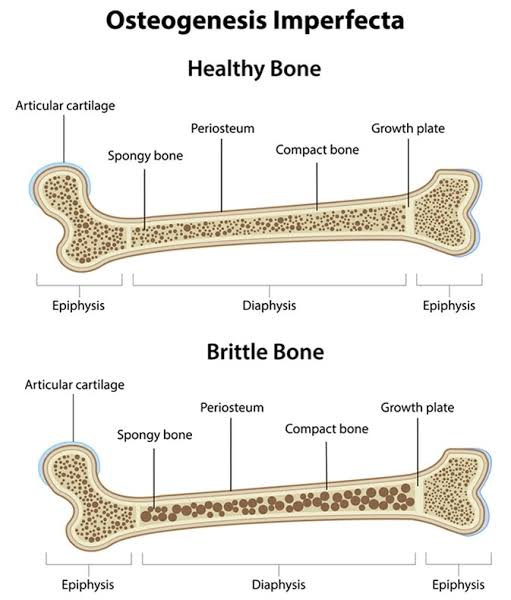
- Osteogenesis imperfecta is a genetic disorder that can be caused by inheritance from a parent with OI, or a random genetic mutation. The genetic disorder in most cases is passed from one of the parents to the child through autosomal dominant inheritance. This means that one copy of the mutated gene in each cell is enough to cause the osteogenesis imperfecta. This type of inheritance is usually the cause for most people with type I or type IV OI. Random mutation of the COL1A1 or COL1A2 gene may also occur. These children have no family history of OI and tend to have either type II or type III osteogenesis imperfecta, which are more serious. The least common way that osteogenesis imperfecta is caused by autosomal recessive inheritance. This is when each cell has two copies of the mutated gene. This cause occurs by two people that are carriers of the mutated gene passing one copy each to a child. This cause usually results in a child with type III OI.
DIFFERENTIAL DIAGNOSIS:

The differential diagnosis for osteogenesis imperfecta can be grouped into stages of life that the differential diagnoses occur.
1) Prenatal/Neonatal :
- Thanatophoric dysplasia
- Jeune dystrophy
- Achondroplasia
- Camptomelic dysplasia
- Chondrodysplasia punctata
- Chondroectodermal dysplasia (Ellis–van Creveld syndrome)
- Nonaccidental injury
- Menkes kinky-hair syndrome
- Menkes Kinky Hair Disease
- Hypophosphatasia”
2) Preschool/Childhood :
- Pyknodysostosis
- Hajdu-Cheney syndrome
- Osteopetrosis
- Vitamin D–resistant rickets
- Osteochondromatosis
- Secondary osteoporosis (immobilization)
- Rickets
- Scurvy
- Leukemia
- Cushing syndrome
- Nonaccidental injury”
3)Adolescence/Adulthood :
- Maffucci syndrome
- Homocystinuria
- Albright hereditary osteodystrophy
- Wilson disease
Milder forms of osteogenesis imperfecta may not be diagnosed early and can often be mistaken for child abuse by physicians.
PHYSIOTHERAPY MANAGEMENT:

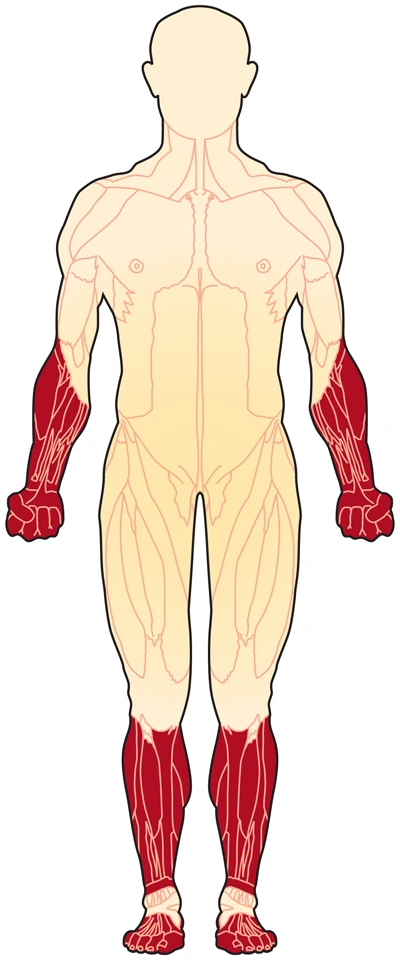
- Physical therapy management for osteogenesis imperfecta can help prevent disuse atrophy of muscle and disuse loss of bone mass. It has also been found that physical therapy can strengthen muscles and even increase bone density in patients with OI. Physical therapy may also help cardiovascular fitness, mental alertness, improved sleep, weight control, ability to fight infection, decrease the chance of certain cancers, and improve activities of daily living. Physical therapy should begin as soon as the child begins to show signs of muscular weakness or motor skills are being accomplished later than other children of the same age.
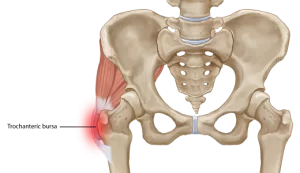
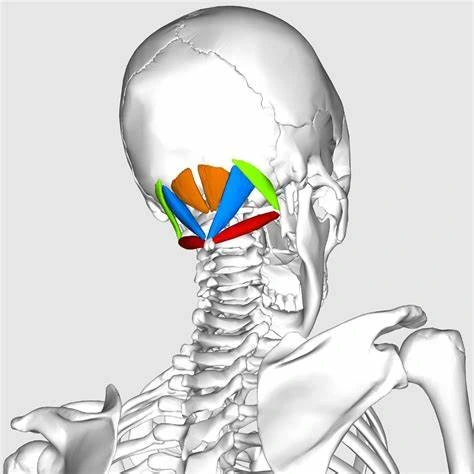
- Physical therapy intervention should include light resistance exercises to strengthen the hips and the core. A combination of hip extension, hip abduction, spinal musculature strengthening, and an aquatic exercise program twice a week has been found to increase the patient’s ability to achieve an upright position and ambulate. Positioning is essential in the care of children with OI. Neutral positioning of the head, trunk, and extremities with the hips in extension is the correct positioning. In more severe cases the prone position should be avoided.
- Physical therapy management may also include the selection and adaptation of ambulation devices that are safe and beneficial to the patients. Adaptive equipment, even powered wheelchairs, may be essential for the child to have as much independence as possible.
- Physical therapy and occupational therapy interventions include muscle strengthening; prevention of joint contractures; prevention of malalignment; improvement in function, including personal activities for daily living; transfers and ambulation; and modification and graded performance of everyday tasks. The therapy team supports children with OI to overcome the many obstacles to independent living, encouraging and respecting their individual problem-solving approaches.


4 Comments