Muscle Atrophy
Table of Contents
What is a Muscle Atrophy?
Muscle atrophy is when muscles waste away. It’s usually caused by a shortage of physical activity. The absence of physical activity due to an injury or illness, poor nutrition, genetics, and certain medical conditions can all contribute to muscle atrophy.
Muscle atrophy is the absence or thinning of muscle tissue. If a person has the presence of atrophied muscles, the person may notice a decrease in muscle mass and strength. With muscle atrophy, muscles look smaller than normal. Muscle atrophy can appear due to malnutrition, age, genetics, a lack of physical activity, or certain medical conditions. Disuse (physiologic) atrophy happens when a person doesn’t use their muscles enough. Neurogenic atrophy appears due to nerve problems or diseases.
Muscle atrophy that develops due to inactivity can occur if a person remains immobile for a long while they recover from an illness or injury. Regular exercise and physical therapy may reverse this type of muscle atrophy.
Types of Muscle Atrophy:
There are 3 main types of muscle atrophy:
- Physiologic atrophy: Physiologic atrophy occurs when muscles are not used enough, such as with prolonged illness.
- Pathologic atrophy: Pathologic atrophy is the type that occurs as a result of any disease such as cancer, severe infections, and malnutrition.
- Neurogenic atrophy: This happens when there is a disturbance of the nerve signals to the muscles.
Several of these issues can push each other and may compound the effects. For example, cancer can result in muscle breakdown due to the disease, and cancer-corresponding fatigue may also lead to an inactive lifestyle—which causes atrophy to advance further.
Disuse Muscle Atrophy:
With muscles, there is a word focused on “use it or lose it.” If a person has been active and exercising, muscles will get larger and more robust in response. If they stop using certain muscles for too long a period, they will decrease in size, as well as in strength.
Little or no physical exercise o work and a sedentary lifestyle are common causes of muscle atrophy, in this case, it is called disuse atrophy. Other common causes of disuse atrophy include medical conditions that decrease mobility, such as rheumatoid arthritis {which is a chronic autoimmune disease characterized by joint inflammation} or osteoarthritis (thinning and weakening of the bones), and injuries, such as breaks in bones and burns. The aging process often directs to slow but progressive muscle atrophy.
Some common reasons for disuse muscle atrophy:
- A sedentary inactive lifestyle and lack of regular physical activity can lead to disuse atrophy and weakness. The atrophy usually ranges from mild to moderate in severity.
- Muscle atrophy occurs very fast when a limb is immobilized. If a person has ever had their leg in a cast, probably how fast they lost muscle in that leg.
- Prolonged immobilization when bedridden due to any disease can direct to severe muscle atrophy that affects many muscles in the body.
- Often, people are motivated to walk and move around while in the hospital—one of the causes is to minimize muscle atrophy.
A vicious cycle can occur with nouse or inactivity of muscle atrophy. Sometimes pain, a condition such as osteoarthritis or rheumatoid arthritis pain, leads to lessened physical activity and muscle atrophy. And weakness due to muscle atrophy makes it a person difficult to follow the recommended exercises—which aggravates stiffness and pain.
Neurogenic Muscle Atrophy:
When a nerve that usually provokes a muscle is damaged, it can no longer trigger muscle contraction that produces muscle activity. Over a long time, the unstimulated muscles may get atrophied. This can happen as an effect of peripheral neuropathy, which is a type of nerve damage, and it can also result from spinal disease or conditions that affect the brain like a stroke.
Neurogenic atrophy:
Muscle atrophy caused by a nerve problem is known as neurogenic atrophy. Common causes comprise neuromuscular diseases, such as spinal cord atrophy, multiple sclerosis (a condition that affects the brain and spinal cord causing weakness, coordination, balance difficulties, and other problems), Amyotrophic Lateral Sclerosis (ALS, also known as Lou Gehrig’s disease; a severe neuromuscular disease that causes muscle weakness and disability), or Guillain-Barre Syndrome (autoimmune nerve disorder). Diabetic neuropathy, nerve damage associated with diabetes, may also direct to muscle atrophy.
Pathologic Atrophy:
Several medical conditions can cause muscle atrophy due to factors such as inflammation, malnutrition, and metabolic problems. These factors can all contribute to a breakdown in muscle.
Examples such as Cancer, AIDS, Dumping syndrome, Dermatom
Causes of Muscle Atrophy:
There are mainly 2 types of muscle atrophy:
- Physiologic
- Pathologic
- Neurogenic.
- Physiologic atrophy is caused by not using the muscles enough or disusing muscles. This type of atrophy can often be treated with exercise and better nutrition. A person who is most affected is those who:
- Have jobs of sitting, health problems that limit movement, or decreased activity levels
- Are bedridden for a long time
- Cannot move their extremity because of stroke or another brain disease
- Are in a place that lacks gravity, such as during flights in space
- Pathologic atrophy is noticed with aging, starvation, and diseases such as Cushing’s disease (because of taking too many medicines called corticosteroids).
- Neurogenic atrophy is the most worse type of muscle atrophy. It happens from an injury to or disease of a nerve that connects to the muscle. This type of muscle atrophy tends to happen more suddenly than physiologic atrophy. When these nerves are damaged, they can not trigger the muscle contractions that are needed to stimulate muscle activity. When the muscles don’t contract, the body thinks that they don’t need them anymore. So the body starts breaking them down, which causes them to decrease in size and strength.
Examples of diseases affecting the nerves which are controlling muscles:
- Amyotrophic Lateral Sclerosis {ALS, or Lou Gehrig’s disease}
- Break to a single nerve, such as Carpal Tunnel Syndrome
- Guillain-Barré syndrome(GBS)
- Nerve damage provoked by injury, diabetes, toxins, or alcohol
- Polio (poliomyelitis)
- Spinal cord injury
- Multiple sclerosis is a disease that affects the brain and spinal cord and results in weakness, coordination, balance difficulties, and other problems)
- Neck or spinal cord injury
- Spinal cord atrophy {Genetic disease causing reduced muscle function from a neural defect}
Although people can adjust to muscle atrophy, even minor muscle atrophy causes some loss of mobility or strength.
Other causes of muscle atrophy may include:
- Lack of physical activity for a vast period of time
- Aging
- Alcohol-associated myopathy is a pain and weakness in muscles due to excessive drinking over long periods of time
- Burns condition
- Muscular dystrophy and other conditions of the muscle
- Osteoarthritis
- Rheumatoid arthritis
- Injuries, such as a tear in the rotator cuff or broken bones
- Malnutrition
- Injury in the Spinal cord or peripheral nerve
- Stroke condition
- Long-term corticosteroid therapy
- Disuse can lead to muscle waste away if a person is not active. But even after it starts, this type of atrophy can often be treated with exercise and improved nutrition.
Muscle atrophy can also happen if a person is bedridden or not able to move certain body parts due to any medical condition. Astronauts, for illustration, can experience muscle atrophy after a few days of weightlessness in space.
Some medical conditions can compel muscles to waste away or can make movement difficult, leading to muscle atrophy. These include:
- Amyotrophic lateral sclerosis (ALS): Also called Lou Gehrig’s disease, affects nerve cells that control voluntary muscle movement
- Dermatomyositis: Causes muscle weakness and rash in the skin
- Guillain-Barré syndrome(GBS): An autoimmune condition that leads to inflammation in nerve and muscle weakness
- Multiple sclerosis: An autoimmune condition in which the body obliterates the protective coverings of nerves
- Muscular dystrophy: is an inherited condition that causes muscle weakness
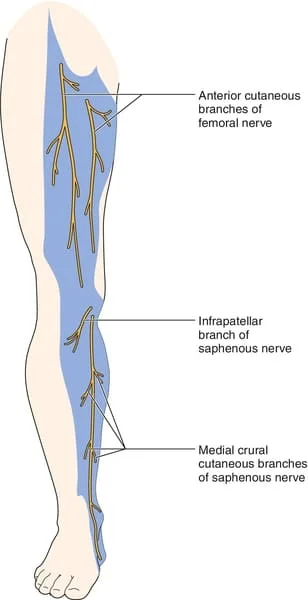
- Neuropathy: Damage to any nerve or nerve group, resulting in loss of sensation or function supplying to muscle
- Osteoarthritis: causes decreased motion in the joints
- Polio: It is a viral disease affecting muscle tissue that can lead to paralysis
- Polymyositis: An inflammatory disease
- Polymyositis: inflammatory muscle disease that causes muscle weakness
- Rheumatoid arthritis: A chronic inflammatory autoimmune disorder that affects the joints
- Spinal muscular atrophy: A genetic condition causing arm and leg muscles to waste away
Symptoms of Muscle Atrophy:
The symptoms of muscle atrophy differ based on the cause of the condition. The most noticeable sign of muscle atrophy is reduced muscle mass. Other signs of muscle atrophy may contain. In addition to decrease muscle mass, symptoms of muscle atrophy have:
- A single arm or single leg is smaller than the other leg.
- Weakness in one arm and one leg.
- Numbness or tingling sensation in the upper and lower extremity.
- Trouble walking or difficulty in balancing.
- Difficulty in swallowing or speaking.
- Facial muscle weakness.
- Gradual memory loss.
- Physically inactive for a very long time.
- Having difficulty balancing
- Remaining inactive for a long period
Muscle atrophy may accompany other signs that vary relying on the underlying disease, disorder, or condition. Symptoms that repeatedly affect the muscles may also involve other body systems.
Neuromuscular symptoms that may happen along with muscle atrophy
Muscle atrophy may accompany other manifestations affecting the neuromuscular system including:
- Balance problems, difficulty walking, and falls
- Difficulty in speaking and swallowing
- Facial muscle weakness
- Incremental difficulty walking and speaking, memory loss, tingling or weakness of extremities
- Impaired balance and coordination problem
- Loss of muscle coordination
- Numbness or tingling in arms or legs or side affected
- Progressive movement loss
- Progressive weakness and numbness in the legs
- Symptoms of multiple sclerosis are weakness, numbness or tingling, vision problems, unsteady walking, fatigue, and depression
Other symptoms that may occur with the muscle atrophy
Muscle atrophy may accompany signs related to other body systems and conditions including:
- Fatigue and a general feeling of not well
- General stiffness that stays more than one hour after rising in the morning
- More frequent episodes of falling and balance problem
- Swelling in an injured area
Serious symptoms that might reveal a life-threatening condition
In some cases, muscle atrophy can be life-threatening. Seek immediate medical care (call 911), have any of these life-threatening sudden symptoms including:
- Change in level of consciousness or alertness, such as handing out or unresponsiveness
- Garbled or slurred speech or incapability to speak
- Paralysis or unable to move a body part
- Sudden change in eyesight, loss of vision, or eye pain
- Sudden weakness or numbness on a side of the body
- Worst headache of life
Diagnosis:
To diagnose muscle atrophy, the healthcare provider will give you a physical exam and ask you about the symptoms. They will observe or look at the arms and legs and measure the muscle mass or muscle girth. In addition, the healthcare provider may order tests, including:
- Blood test.
- Muscle or nerve biopsy.
- Electromyography (EMG).
- Nerve conduction studies.
- X-rays.
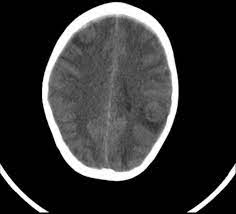
- Computed tomography (CT) scan.
- (MRI) Magnetic Resonance Imaging: To show internal tissues such as muscle, ligaments
If muscle atrophy is caused by any other condition, there may need to undergo testing to diagnose the condition.
A doctor will request for complete medical history. The doctor will likely be asked to:
- Inform about old or recent injuries and previously diagnosed medical conditions
- List prescriptions, over-the-counter medications, and supplements the person taking
- Tell a detailed description of the symptoms
A doctor may refer the person to a specialist depending on the results of these tests.
Treatment of Muscle Atrophy:
Treatments for muscle atrophy vary depending on how many degrees of muscle loss and the presence of any underlying medical conditions.
Treating the underlying disease causing muscle atrophy may help slow down the progression of muscle loss.
Muscle atrophy, or muscle wasting, is characterized by a marked shortening of the muscle fibers and a loss of overall muscle mass.
Several factors can donate to muscle atrophy, such as:
- Remaining stationary for long periods due to illness or injury
- Age
- Malnutrition
- Genetics
- Neurological problems
- Certain medical disorders, such as arthritis, myositis, ALS, and MS
Treatment options will rely on each case, but they may include physical therapy, nutritional intervention, or surgery.
Treatment will be based on the diagnosis and the severity of the muscle loss. Any underlying medical conditions must be addressed. Common treatments for muscle atrophy include:
- Exercise
- Physical therapy
- Ultrasound therapy
- Surgery
- Dietary changes
Recommended exercises might include water exercises to help move easier.
Physical therapy in Muscle Atrophy
Physical therapists can teach the correct ways to exercise. They can also move their arms and legs if they have trouble moving. Physical therapy may help improve movement in people with muscle atrophy. Physical therapy includes performing specific stretches and exercises to prevent immobility. Physical therapy offers the following advantages to people who have muscle atrophy:
- Preventing immobility
- Increasing muscle strength
- Improving circulation
- Reducing spasticity, which causes continuous muscle contraction
Physical activity provides a significant anabolic muscle stimulus and is an essential component in slowing or reversing muscle atrophy. It is still not known regarding the ideal exercise “dosing.” Resistance exercise is beneficial in reducing muscle atrophy in an older person. In patients who cannot exercise due to physical limitations such as paraplegia, functional electrical stimulation(FES) can be used to externally stimulate the muscles.
Modalities used while physical therapy:
Functional electric stimulation:
Functional electrical stimulation (FES) is another effective treatment for treating muscle atrophy. It involves the use of electrical impulses to stimulate muscle contraction in the muscles of the affected side.
During FES, a trained technician placed electrodes on an atrophied limb. The electrodes transmit an electrical current, which activates the movement in the limb.
Focused ultrasound therapy:
This technique delivers beams of ultrasound power to specific areas in the body. The rays stimulate contractions in atrophied muscle tissue. This unexplored technology is in the development phase and has not yet entered the clinical trial phase. Ultrasound therapy is a noninvasive procedure that uses sound waves to aid in healing the muscle. If your tendons, ligaments, skin, or muscles get too tight and prevent a person from moving, surgery may be necessary. This condition is called contracture deformity.
Exercises:
Exercise may increase the range of movement and strength of the atrophied muscle. Exercises may include:
Active and passive movement:
- Passive movement: If muscles do not have the strength to perform the movement, the therapist performs the movement in the available range.
- Active assisted: As muscles gain some strength and some range, actively assisted exercise starts. The therapist assists in the movements to perform full range.
- Active movements: As total muscle strength is achieved, a patient can perform active movements in full range.
Resisted exercise: As the patient can perform an active movement in full range, the therapist starts the movement with resistance to increase the strength. Resistance may be:
- Manual and mechanical: Manual by hand and mechanical by elastic, theraband, weight cuff. isometric exercise can be done.

Surgical treatment:
Surgical procedures may enhance muscle function in people whose muscle atrophy is related to neurological conditions, injuries, or malnutrition.
Surgery may be able to correct contracture deformity if the muscle atrophy is due to malnutrition. It may also be able to correct the condition if a torn tendon caused muscle atrophy.
If malnutrition is the reason for muscle atrophy, a doctor may suggest dietary changes or supplements.
Diet and nutrition:
Adequate calories and protein are crucial to prevent muscle atrophy. Protein needs may vary dramatically based on metabolic factors and disease state, so high-protein supplementation may be beneficial. Supplementation of protein or branched-chain amino acids, especially leucine, can deliver a stimulus for muscle synthesis and inhibit protein breakdown and it has been studied for muscle atrophy for sarcopenia and cachexia. β-Hydroxy β-methyl butyrate (HMB), a metabolite of leucine that is marketed as a dietary supplement, has presented efficacy in preventing the loss of muscle mass in several muscle-wasting conditions in humans, particularly sarcopenia. HMB supplementation has efficacy as a treatment for maintaining lean muscle mass in older adults. More research is needed to determine the accurate effects of HMB on muscle strength and function in various populations.
In extreme cases of muscular atrophy, the use of an anabolic steroid such as methandrostenolone may be allocated to patients as a potential treatment although use is limited by side effects. A novel class of drugs, called selective androgen receptor modulators, is being investigated with bright results. They would have rarer side effects, while still stimulating muscle and bone tissue growth and regeneration. These effects have yet to be verified in larger clinical trials.
Outcomes:
Outcomes of muscle atrophy rely on the underlying cause and the health of the patient. Stationary or bed rest in populations predisposed to muscle atrophy, such as the elderly or those with illness states that commonly cause cachexia, can cause dramatic muscle atrophy and impact functional outcomes. In the elderly, this often leads to decreased biological reserve and increased vulnerability to stressors known as the “frailty syndrome.”Loss of lean body mass is also associated with a raised risk of infection, reduced immunity, and poor wound healing. The weakness that accompanies muscle atrophy leads to a higher risk of falls, fractures, physical disability, need for institutional care, reduced quality of life, increased mortality, and increased healthcare costs.
FAQs:
What happens if you have atrophied muscles?
If a person has atrophied muscles, a person sees a decrease in muscle mass and strength. With muscle atrophy, the muscles look smaller than normal. Muscle atrophy can occur due to the following reasons: malnutrition, age, genetics, a lack of physical activity, or certain medical conditions. Disuse (physiologic) atrophy occurs when they don’t use their muscles enough.
What are the different types of muscle atrophy?
Muscle atrophy. Pathologic atrophy is noticed with aging, starvation, and diseases such as Cushing’s disease (because of taking many medicines called corticosteroids). Neurogenic atrophy is the most painful type of muscle atrophy. It can be from an injury to, or disease of a nerve that attaches to the muscle.
What is musculoskeletal atrophy?
Muscle atrophy is the reduction of skeletal muscle mass. It can be caused by these reasons: Immobility, Aging, Malnutrition, Medications, or a wide range of injuries or diseases that impact the musculoskeletal or nervous system.
How does muscle atrophy diagnose?
Doctors can diagnose muscle atrophy by observing the muscle mass. And to confirm, the doctor may perform some examinations such as:
Blood tests, Muscle or nerve biopsy, Electromyography (EMG), Nerve conduction studies, X-rays, and Computed tomography (CT) scans.
(MRI) Magnetic Resonance Imaging: To show internal tissues such as muscle, ligaments
If muscle atrophy is caused by any other condition, there may need to undergo testing to diagnose the condition.How can muscle atrophy treat?
Muscle atrophy can be treated with medicine, surgery, and physical therapy.





My grandma who has been Lou Gehrig’s disease for 2 years at the age of 75 had all his symptoms reversed with a herbal medicine from health natural centre . org after undergoing their herbal treatment plan. God Bless all ALS Caregivers. Stay Strong, take small moments throughout the day to thank yourself, to love your self, and pray to whatever faith, star, spiritual force you believe in and ask for strength. I can personally vouch for these remedy but you would probably need to decide what works best for you.