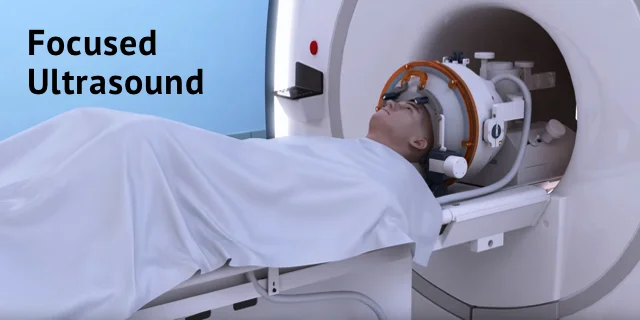
Focused Ultrasound
Table of Contents
Overview
- Focused ultrasound is a quickly evolving, noninvasive therapeutic technology with the potential to transform the treatment of several medical disorders by using ultrasonic energy to target tissue deep in the body without any type of incisions or radiation.
Focused ultrasound is the union of two different innovative technologies:
Focused ultrasound–
which gives the energy to treat tissue deep in the body precisely and noninvasively.
Magnetic resonance or ultrasound imaging—
which is used to recognize and target the tissue to be treated, guide and control the treatment in real-time, and confirm the effectiveness of the treatment.
- The fundamental principle is analogous to utilizing a magnifying glass to focus beams of sunlight on a single point to burn a hole in a leaf.
- With focused ultrasound, an acoustic lens is used to centralize multiple intersecting beams of ultrasound on a target deep in the body with extreme precision and accuracy.
- Depending on the design of the lens and the ultrasound parameters, the target can be as compact as 1×1.5mm or as large as 10x16mm in diameter.
- Where each of the single beams passes through the tissue, there is no effect. But, at the focal point, the convergence of the multiple beams of focused ultrasound energy results in many essential biological effects, generating the possibility of treating a variety of medical disorders.
- Focused ultrasound treatments may be performed on an outpatient basis, constrain no incisions, and may result in minimal discomfort and fewer complications, allowing for rapid recovery.
High-intensity focused ultrasound-
- High-intensity focused ultrasound (HIFU) is an intraoperative therapeutic technique, that uses non-ionizing ultrasonic waves to heat or ablate tissue.
- HIFU may be used to improve the flow of blood or lymph or to destroy tissue, like, tumors, via thermal and mechanical mechanisms.
- Given the generality and relatively little cost of ultrasound, HIFU has been subject to much more research and development.
- The premise of HIFU is that it is a non-invasive low-cost therapy that may at minimum outperform the current standard of care.
- The technology varies from that used in ultrasonic imaging, though lower frequencies and continuous, rather than pulsed, waves are used to accomplish the mandatory thermal doses.
- In spite of the fact that pulsed waves can also be used if mechanical rather than thermal damage is desired.
- Acoustic lenses are often used to accomplish the mandatory intensity at the target tissue without damaging the surrounding tissue.
- An association is using a magnifying glass to focus sunlight; only the focal point of the magnifying glass has high intensity.
- Nevertheless, lenses have occasionally been used, phased arrays are increasingly ordinary as they allow the focal position to be easily changed.
- HIFU is traditionally incorporated with other imaging techniques like medical ultrasound or MRI to enable guidance of the treatment and monitoring.
Medical uses-
- There is no clear agreement on the boundaries between HIFU and other forms of therapeutic ultrasound.
- In academic literature, HIFU generally refers to the high levels of energy required to demolish tissue through ablation or cavitation, in spite of the fact that it is also sometimes used to mark out lower-intensity applications like occupational therapy and physical therapy.
- Either way, HIFU is utilized to non-invasively heat tissue deep in the body without the need for an incision.
- The main applications are the demolition of tissue, increasing perfusion, and physical therapy.
- The application of ultrasound in the treatment of musculoskeletal conditions is another utilization in the physiotherapy setting.
Neurological disorders
- One of the first implementations of HIFU was the treatment of Parkinson’s disease in the 1940s.
- In spite of the fact that it is ineffective at the time, HIFU has the range for lesion pathology.
- A focused ultrasound system is accepted in Israel, Canada, Europe, Korea, and Russia to treat essential tremors, neuropathic pain, and Parkinsonian tremors.
- This proposal authorizes the treatment of the brain without an opening or radiation. In 2016, the US Food and Drug Administration (FDA) approved Insightec’s Exablate system to give treatment to essential tremors.
- Treatment for other thalamocortical dysrhythmias and psychiatric conditions is under research.
Uterine adenomyosis and fibroids
- Treatment for symptomatic uterine fibroids became the first approved solicitation of HIFU by the US Food and Drug Administration (FDA).
Cancers
- HIFU is a captivating option for tumors in locations that are hard to reach or non-resectable.
- f particular attentiveness is intestinal cancers and brain cancer.
- When putting forward treatment, a therapist must think about the other modalities to determine if HIFU is a viable option [supposing commercial statement].
Prostate cancer
- It is also utilized in the treatment of prostate cancer in male patients.
Liver cancer
- HIFU is well-studied in liver cancer and in too many studies report a high response rate and constructive patient results.
Abscopal effect
- At the time of treatment of metastasized liver cancer with HIFU, immune responses have been noticed in the area that is distant from the focal region.
- In spite of the fact that the mechanism of this systemic response is unknown, it is thought to be brought out by liberating the tumor antigens with retained immunogenicity to be brought out by the release of tumor antigens with retained immunogenicity through histotripsy.
Other cancers
- HIFU has been applied in the therapy of cancer to demolish the solid tumors of the pancreas.
Palliative care
- HIFU has been found to have palliative effects. CE acceptance has been given for the palliative treatment of bone metastasis.
- Analytically, a palliative effect was established in cases of advanced pancreatic cancer.
Prostate enlargement
- Therapy of prostate enlargement (benign prostatic hyperplasia) by HIFU from inside the intestine (transrectal) has turned out to be ineffective.
Varicose veins
- In the field of varicose veins, the new medical achievement is high-intensity focused ultrasound (HIFU).
- Ultrasound therapy is a major technological innovation and a non-invasive intervention technique for individuals who are suffering from varicose veins.
- This treatment utilizes ultrasound: high-energy waves solicited to a specific area of the body allow a localized increase in temperature.
- The ultrasound waves are efficient in penetrating the skin without damage, to treat the veins in a targeted area.
- This heat denatures the selected cellular molecules in order to eliminate them.
- This method, also known as ecotherapy, is completely non-invasive and is not automatically performed in an operating room, unlike existing techniques.
- The procedure is performed from outer the body, leaving no scars and allowing the patient to return to his or her daily life straight away.
- Its chief strength is that it provides a substitute method of treating varicose veins that have developed into venous ulcers.
Mechanism
- The focusing effect of the transducer permits high sound pressures to be carried through to a focal point without causing unwanted damage to other tissue.
- This improvement in pressure may cause a number of effects including heating and cavitation.
- The transducers vary from ultrasonic imaging probes which many people are familiar with.
- Ultrasound sources may be utilized to create regional heating and mechanical changes in biological tissue, like, for cancer treatment.
- Focused ultrasound can be utilized to create highly localized heating to treat cysts and tumors (benign or malignant).
- This is well known as Magnetic Resonance guided Focused Ultrasound (MRGFUS) or High Intensity Focused Ultrasound (HIFU).
- These procedures commonly use lower frequencies than medical diagnostic ultrasound (from 0.250 to 2 MHz), but exceptionally higher energies.
- HIFU treatment is often guided by MRI.
- Focused ultrasound may be utilized to dissolve kidney stones by lithotripsy.
- Ultrasound can be utilized for cataract treatment by phacoemulsification.
Ideal temperature consideration
- The temperature of tissue at the focus will rise to between 65 and 85 °C, demolishing the diseased tissue by coagulative necrosis.
- If tissue is increased above the threshold of 60 °C for longer than 1 second this process is irreversible.
- Every sonication (individual ultrasound energy deposition) treats an accurately defined part of the targeted tissue.
- The whole therapeutic target is treated by utilizing multiple sonications to receptacle a volume of an incompressible material, like tap water, sea water…
- The treatment will be done by means of the shape of the cylinder in the part, therefore, it is supposed to be adopted the formula of Bessel’s (Cylinder) function.
- The ideal “IN-VITRO”, just in tap water examination, formulations of the CEM equation have been assumed as with the integral being over the treatment time, R=0.5 for temperatures over 43 °C and 0.25 for temperatures in the middle of 43 °C and 37 °C, a reference temperature of 43 °C, and time T is in minutes.
- The equations and methods mark out in this report are not deliberate to represent any clinical result, this is the only approach for thermal dose estimation in compressive material of just tap water.
- As an ultrasound acoustic wave may not propagate through the compressive tissue, like rubber, or human tissues part of it and the ultrasound energy will be turned to converted as heat, with focused beams, a very tiny region of heating may be achieved in the part of shallow deep in tissues (normally on the order of 3~5 millimeters).
- Tissue occurs as a function of both the subtle shaking to which the water is heated and how long the part of the water is uncovered to this heat level in a metric referred to as “thermal dose”.
- By focusing at more than one place or by scanning the focus, a volume may be thermally ablated.
- Thermal doses of 120-240 min at 43 °C coagulate cellular protein and leads to irrevocable tissue destruction.
- There is some proof that HIFU can be applied to cancers to interrupt the tumor microenvironment and trigger an immune response, as well as possibly enhance the efficacy of immunotherapy.
Mechanical theory-
Inertial cavitation
- At high sufficient acoustic intensities, cavitation (microbubbles forming and interacting with the ultrasound field) may occur.
- Microbubbles create in the field oscillate and grow (due to factors including rectified diffusion), and may ultimately implode (inertial or transient cavitation).
- At the time of inertial cavitation, very high temperatures happen inside the bubbles, and the collapse at the time of the rarefaction phase is associated with a shock wave and jets that may mechanically damage tissue.
Stable cavitation
- Stable cavitation produces microstreaming which involves high shear forces on cells and leads to apoptosis.
- Elaborating, bubbles create by the vaporization of water because acoustic forces oscillate under a low-pressure acoustic field.
- Strong streaming can cause cell damage but also decreases tissue temperature via convective heat loss.
Theory
- There are too many ways to focus ultrasound—via a lens (for example, a polystyrene lens. Parabola curved transducer, a phased array, etc.
- The special individual and very precise technology solve the problem.
- This may be intent on using an exponential model of ultrasound attenuation.
- The ultrasound intensity profile is bounded by an exponentially reducing function where the reduction in ultrasound is a function of the distance traveled through tissue:
The ultrasound beam may be focused in these ways:
Geometrically-
- As an example with a lens or with a spherically curved transducer.
Electronically-
- By regulating the relative phases of elements in an array of transducers (a “phased array”).
Dynamically –
- Adjusting the electronic signals to the elements of a phased array, the beam may be steered to various locations, and aberrations in the ultrasound beam because of tissue structures may be corrected.
Beam delivery
- Beam delivery contains beam steering. The beam has the capacity to pass through overlying tissues without damage and focus on a localized area with a size limit of 3–4 mm, with clinical ultrasound such as 1 MHz to 5 MHz usually.
- The part at the focal point of the beam undergoes coagulative necrosis.
- Following ablation a distinct boundary forms among the healthy and necrotic tissue (width less than 50 microns).
Beam streaming
- The most usual transducer utilization is a concave focusing transducer with a fixed aperture and a fixed focal length.[44] Phased array transducers can also be used with different arrangements (flat/bowl).
Focused Ultrasound In Parkinson’s Disease
- Focused ultrasound is a quickly evolving, noninvasive, therapeutic technology with the potential to increase the quality of life and reduce the cost of care for patients with Parkinson’s disease.
- This narrative technology pivots the beams of ultrasonic energy precisely and accurately on targets deep in the brain without damaging nearby normal tissue.
How it Works
- Where the beams converge, focused ultrasound constructs a variety of therapeutic effects enabling Parkinson’s disease to be treated without surgery.
- For movement disorders, the mechanism is ablation (thermal disruption of the tissue) that may be aimed at several different treatment targets.
- For the preclinical work in treating the underlying cause, the mechanisms may be temporarily disrupting the blood-brain barrier (BBB), which will permit the desired therapeutics the ability to enter the brain.
- Opening the BBB also may authorize undesired materials to depart from the brain.
Advantages
- Nowadays, there is no rehabilitation for Parkinson’s, and the major options for the treatment of motor symptoms include drug therapy and invasive surgery (For example, deep brain stimulation, and radiofrequency lesioning).
- For particular patients, focused ultrasound could permit a noninvasive alternative to surgery with a lower risk of complications and lower cost.
- In the long term, focused ultrasound has the prospect to treat the underlying disease pathology and prevent progression and/or restoring function.
Relief of Motor Symptoms
- The FDA has approved the utilization of focused ultrasound for the treatment of tremor-dominated Parkinson’s disease.
- Focused ultrasound has the prospective to carry off symptomatic relief by making thermal lesions deep in the brain to intersperse circuits involved with tremors and dyskinesia.
Symptoms and targets being evaluated for treatment using focused ultrasound include:
Parkinsonian tremor –
- Pick out in the thalamus (thalamotomy)
Parkinsonian dyskinesia –
- Pick out in the globus pallidus (pallidotomy) or subthalamic nucleus
Parkinsonian tremor, akinesia, or dyskinesia –
- Pick out in the pallidothalamic tract.
Summary-
- At this time, focused ultrasound is only being evaluated to treat one side of the brain, so it will influence tremors or dyskinesia unilaterally.
- Studies are being organized to evaluate the possibility of treating patients bilaterally, and one is included below.
- Focused ultrasound is non-invasive – no incisions, holes in the skull, or electrodes in the brain – and therefore has brought down the risk of infection and blood clots.
- Precise targeting lowers the damage to the non-targeted healthy brain.
- As compared to deep brain stimulation, focused ultrasound is a single treatment, and does not need any subsequent procedures/visits to replace batteries, repair broken wires, or adjust simulator settings.
- It also does not include the collateral damage to healthy and wealthy tissue or the risk of infections associated with implanting a foreign body.
Treating Underlying Pathology
- Preclinical studies recommend focused ultrasound’s potential to reinstitute the function in Parkinson’s models.
- Focused ultrasound may for the moment open the blood-brain barrier (BBB) to increase the delivery of:
- Genes
- growth factors
- stem cells
- other neuroprotective and/or neurorestorative drugs
- Anti-alpha synuclein antibodies.
FAQ-
In clinical studies, permanent unsteadiness was reported in up to 10% of the patients. Little side effects, like headache, pain, and
dizziness: Some patients may experience warmth, pain, or dizziness lasting only for a few seconds during the procedure. These
effects are not experienced after the procedure.
Focused ultrasound typically reduces the symptoms immediately. It does not essential adjustment, programming, or additional
procedures. But it is irrevocable and permanent. Possible side effects may include headache, numbness and tingling, imbalance or
gait changes, and others.
To ensure patient safety, focused ultrasound uses an MRI thermal imaging system that estimates the temperature changes in the
skull. This new procedure allows doctors to perform a safe and effective non-invasive therapy with tiny to no harm to the
surrounding tissue and with minimal side effects.
Focused ultrasound is a rapidly evolving, noninvasive, therapeutic technology with the potential to increase the quality of life and
decrease the cost of care for patients with neuropathy.
Mechanical stress can be used to stimulate peripheral nerve regeneration while neurorehabilitation. Therapeutic ultrasound (US)
is a favorable treatment that promotes nerve regeneration.