Flat feet : Physiotherapy Treatment
Flat feet (also called pes planus or fallen arches) is a postural deformity in which the arches of the foot collapse, with the entire sole of the foot coming into complete or near-complete contact with the ground.
Flat feet (also called pes planus or fallen arches) is a postural deformity in which the arches of the foot collapse, with the entire sole of the foot coming into complete or near-complete contact with the ground. An estimated 20–30% of the general population have an arch that simply never develops in one or both feet.
There is a functional relationship between the structure of the arch of the foot and the biomechanics of the lower leg. The arch provides an elastic, springy connection between the forefoot and the hind foot so that a majority of the forces incurred during weight bearing of the foot can be dissipated before the force reaches the long bones of the leg and thigh.
In pes planus, the head of the talus bone is displaced medially and distal from the navicular bone. As a result, the Plantar calcaneonavicular ligament (spring ligament) and the tendon of the tibialis posterior muscle are stretched, so much so that the individual with pes planus loses the function of the medial longitudinal arch (MLA). If the MLA is absent or nonfunctional in both the seated and standing positions, the individual has “rigid” flatfoot. If the MLA is present and functional while the individual is sitting or standing up on their toes, but this arch disappears when assuming a foot-flat stance, the individual has “supple” flatfoot. This latter condition is often treated with arch supports.However, a recent randomized controlled trial found no evidence for the efficacy of treatment of flat feet in children either from expensive prescribed orthotics (i.e., shoe inserts) or less expensive over-the-counter orthotics.
Three studies (see citations below in Military performance section) of military recruits have shown no evidence of later increased injury, or foot problems, due to flat feet, in a population of people who reach military service age without prior foot problems. However, these studies cannot be used to judge possible future damage from this condition when diagnosed at younger ages. They also cannot be applied to persons whose flat feet are associated with foot symptoms, or certain symptoms in other parts of the body (such as the leg or back) possibly referable to the foot.
People with flat feet, also known as fallen arches, have either no arch in their feet or one that is very low.
There is usually a gap beneath the inner part of the foot when a person stands, as the arch raises off the ground slightly.
Flat feet only need treatment if they cause discomfort, indicate an underlying disorder, or lead to pain elsewhere in the body. Some people appear to have a very low arch or no arch without ever experiencing problems.
When flat feet do cause symptoms, simple devices and exercises can help to minimize the discomfort.
Read on to learn more about the causes, symptoms, and treatment of flat feet.
People with flat feet have a very low arch or no arch, meaning that one or both of their feet may be flat on the ground.
A human foot has 33 joints, which hold 26 different bones together. It also has over 100 muscles, tendons, and ligaments.
The arches provide a spring to the step and help to distribute body weight across the feet and legs. The structure of the arches determines how a person walks. The arches need to be both sturdy and flexible to adapt to stress and a variety of surfaces.
When people have flat feet, their feet may roll to the inner side when they are standing and walking. This is known as overpronation, and it may also cause the feet to point outward.
Many people with flat feet have no symptoms, but others will experience a variety of symptoms that generally depend on the severity of the condition.
Table of Contents
Flat feet symptoms :
The most common symptom of flat feet is pain in the feet. This can occur as a result of strained muscles and connecting ligaments.
Abnormal stresses on the knee and hip may result in pain in these joints. These stresses are likely if the ankles turn inward.
Pain most commonly affects the following parts of the body:
inside ankle, alongside possible swelling
- arch of the foot
- calf
- knee
- hip
- lower back
- lower legs
- One or both feet may also feel stiff.
Flat feet can also cause an uneven distribution of body weight. This may result in shoes wearing down unevenly or more quickly than usual, especially on one side, which can lead to further injuries.
Causes :
Common causes of flat feet include:
genetic factors, as flat feet can pass from parents to children in the genes
weak arches, meaning that the arch is visible when a person sits but the foot flattens onto the ground when they stand
foot or ankle injury
arthritis or rheumatoid arthritis
damage, dysfunction, or rupture of the posterior tibial tendon
nervous systems or muscle diseases, such as cerebral palsy, muscular dystrophy, or spina bifida
Another condition that might cause flat feet is tarsal coalition. This condition causes the bones of the foot to fuse together unusually, resulting in stiff and flat feet.
Pediatricians usually diagnose this condition during childhood.
People are more likely to develop flat feet if they have obesity or diabetes. Flat feet are also more common during pregnancy.
Flat feet can develop with age too. Daily use of the feet can cause the posterior tibial tendon to weaken. This tendon is the primary support structure for the foot arch.
The tendon can become inflamed, called tendonitis, or tear after overuse. Damage to the tendon may cause the foot arch to flatten.
Flat feet can also occur as a result of a developmental fault that occurs during childhood or that develops with age or after pregnancy.
Risk factors
Factors that can increase your risk of flatfeet include:
Obesity
Injury to your foot or ankle
Rheumatoid arthritis
Aging
Diabetes
Complications :
bunion diagram
Flat feet can lead to bunions.
People with other foot, ankle, or lower leg problems may find that flat feet can contribute to them or make symptoms worse.
Examples include:
Achilles tendonitis
arthritis in the ankle or ankles
arthritis in the foot or feet
bunions
hammertoes
plantar fasciitis, an inflammation of the ligaments in the soles of the feet
posterior tibial tendonitis
shin splints
Flat feet can affect the alignment of the body when a person is standing, walking, or running. As a result, they can increase the likelihood of pain developing in the hips, knees, and ankles.
Flat feet in children :
Children may sometimes appear to have flat feet when the arch is still forming.
Children and infants may often appear to have flat feet.
In fact, the arch is usually present but still forming. In time, the arch should develop normally. The extra fat on an infant’s foot may hide the arch.
Having feet that appear flat during early childhood does not mean that a person will always have flat feet.
However, if a child has flat feet as a result of incorrect bone development or another condition, such as spina bifida, a doctor will often need to treat the underlying cause.
Diagnosis :
People with flat feet who do not experience pain or other symptoms do not usually need to consult a doctor.
However, anyone with the following symptoms should seek medical advice:
flat feet that have only developed recently.
pain in the feet, ankles, or lower limbs.
symptoms that do not improve with supportive, well-fitted shoes.
one or both feet becoming more flat
the feet feeling rigid, stiff, heavy, and unwieldy
Most qualified healthcare professionals can diagnose fallen arches by examining the feet and observing the individual as they stand and walk.
A doctor will also look at the person’s medical history. In some cases, they may order an X-ray, CT scan, or MRI scan.

Exercises :
A podiatrist or physical therapist may recommend specific exercises to manage the symptoms of flat feet or prevent them from developing.
Heel cord stretching
A tight Achilles tendon will encourage the foot to roll inward. The aim of heel cord stretching is to stretch the Achilles tendon and posterior calf muscles.
Stand facing a wall and place one hand on the wall at eye level.
Place the leg that needs stretching approximately one step behind the other leg, and plant the heel firmly on the ground.
Bend the knee of the front leg until you feel a stretch in the back leg.
Hold for 30 seconds and then rest for 30 seconds. Repeat nine more times.
It is essential to avoid arching the back and to keep it straight.
Perform this exercise twice a day.

The golf ball roll
Sit on the chair with your feet firmly on the ground. Place the golf ball under the foot, and roll it forward and back under the arch of the foot for 2 minutes to stretch the plantar fascia ligament.
Treatment
Some people with flat feet may automatically align their limbs in a way that prevents symptoms. People who are not experiencing symptoms do not usually require treatment.
If flat feet are causing pain, then supportive, well-fitted shoes can help. Extra-wide-fitting shoes can provide relief.
Fitted insoles and orthotics or custom-designed arch supports may relieve pressure on the arch and reduce pain if the feet roll too far inward. However, these products only treat the symptoms and do not provide long-lasting benefits.
People with posterior tibial tendonitis might also benefit from inserting a wedge into their footwear along the inside edge of the orthotic. This should relieve some of the load that the body places on the tendon tissue.
Wearing an ankle brace may also be beneficial until the inflammation reduces.
Doctors may advise some people to rest until their symptoms improve and to avoid activities that might aggravate the foot or feet.
A person with arthritis or a ruptured tendon might find that a combination of an insole and pain relievers can minimize their symptoms. If these do not work, surgery may be necessary.
Some bones do not develop properly in childhood, which can result in flat feet from birth continuing into adulthood. In these rare cases, surgical intervention may be necessary to separate fused bones.
When obesity is the cause of flat feet, losing weight might improve the symptoms.
Adults
Flat feet can also develop as an adult (“adult acquired flatfoot”) due to injury, illness, unusual or prolonged stress to the foot, faulty biomechanics,or as part of the normal aging process. This is most common in women over 40 years of age. Known risk factors include obesity, hypertension and diabetes.Flat feet can also occur in pregnant women as a result of temporary changes, due to increased elastin (elasticity) during pregnancy. However, if developed by adulthood, flat feet generally remain flat permanently.
If a youth or adult appears flatfooted while standing in a full weight bearing position, but an arch appears when the person plantarflexes, or pulls the toes back with the rest of the foot flat on the floor, this condition is called flexible flatfoot. This is not a true collapsed arch, as the medial longitudinal arch is still present and the windlass mechanism still operates; this presentation is actually due to excessive pronation of the foot (rolling inwards), although the term ‘flat foot’ is still applicable as it is a somewhat generic term. Muscular training of the feet is helpful and will often result in increased arch height regardless of age.
Pathophysiology
Research has shown that tendon specimens from people who suffer from adult acquired flat feet show evidence of increased activity of proteolytic enzymes. These enzymes can break down the constituents of the involved tendons and cause the foot arch to fall. In the future, these enzymes may become targets for new drug therapies
Diagnosis
Many medical professionals can diagnose a flat foot by examining the patient standing or just looking at them. On going up onto tip toe the deformity will correct when this is a flexible flat foot in a child with lax joints. Such correction is not seen in adults with a rigid flat foot.
An easy and traditional home diagnosis is the “wet footprint” test, performed by wetting the feet in water and then standing on a smooth, level surface such as smooth concrete or thin cardboard or heavy paper. Usually, the more the sole of the foot that makes contact (leaves a footprint), the flatter the foot. In more extreme cases, known as a kinked flatfoot, the entire inner edge of the footprint may actually bulge outward, where in a normal to high arch this part of the sole of the foot does not make contact with the ground at all.
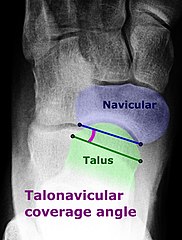
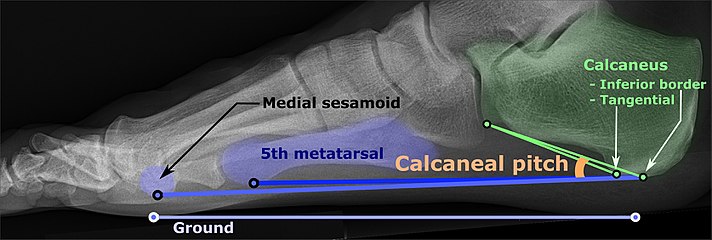
On plain radiography, flat feet can be diagnosed and graded by several measures, the most important in adults being the talonavicular coverage angle, the calcaneal pitch, and the talar-1st metatarsal angle (Meary’s angle).The talonavicular coverage angle is abnormally laterally rotated in flat feet.It is normally up to 7 degrees laterally rotated, so a greater rotation indicates flat feet. Radiographies generally need to be taken on weightbearing feet in order to detect misalignment.
Treatment
Most flexible flat feet are asymptomatic, and do not cause pain. In these cases, there is usually no cause for concern. Flat feet were formerly a physical-health reason for service-rejection in many militaries. However, three military studies on asymptomatic adults (see section below), suggest that persons with asymptomatic flat feet are at least as tolerant of foot stress as the population with various grades of arch. Asymptomatic flat feet are no longer a service disqualification in the U.S. military, but symptomatic flat feet are cause for disqualification during the enlistment process.[citation needed]
In a study performed to analyze the activation of the tibialis posterior muscle in adults with pes planus, it was noted that the tendon of this muscle may be dysfunctional and lead to disabling weightbearing symptoms associated with acquired flat foot deformity. The results of the study indicated that while barefoot, subjects activated additional lower-leg muscles to complete an exercise that resisted foot adduction. However, when the same subjects performed the exercise while wearing arch supporting orthotics and shoes, the tibialis posterior was selectively activated. Such discoveries suggest that the use of shoes with properly fitting, arch-supporting orthotics will enhance selective activation of the tibialis posterior muscle thus, acting as an adequate treatment for the undesirable symptoms of pes planus.
Rigid flatfoot, a condition where the sole of the foot is rigidly flat even when a person is not standing, often indicates a significant problem in the bones of the affected feet, and can cause pain in about a quarter of those affected. Other flatfoot-related conditions, such as various forms of tarsal coalition (two or more bones in the midfoot or hindfoot abnormally joined) or an accessory navicular (extra bone on the inner side of the foot) should be treated promptly, usually by the very early teen years, before a child’s bone structure firms up permanently as a young adult. Both tarsal coalition and an accessory navicular can be confirmed by X-ray. Rheumatoid arthritis can destroy tendons in the foot (or both feet) which can cause this condition, and untreated can result in deformity and early onset of osteoarthritis of the joint. Such a condition can cause severe pain and considerably reduced ability to walk, even with orthoses. Ankle fusion is usually recommended.
Treatment of flat feet may also be appropriate if there is associated foot or lower leg pain, or if the condition affects the knees or the lower back. Treatment may include foot gymnastics or other exercises as recommended by a podiatrist or physical therapist. In cases of severe flat feet, orthoses should be used through a gradual process to lessen discomfort. Over several weeks, slightly more material is added to the orthosis to raise the arch. These small changes allow the foot structure to adjust gradually, as well as giving the patient time to acclimatise to the sensation of wearing orthoses. In some cases, surgery can provide lasting relief, and even create an arch where none existed before; it should be considered a last resort, as it is usually very time consuming and costly. A minimally-invasive surgical intervention involving a small implant is also available. The implant is inserted into the sinus tarsi and prevents the calcaneus and talus from sliding relative to each other. This prevents the sinus tarsi from collapsing and thus prevents the external symptom of the fallen arch from occurring.





16 Comments