Erb’s palsy
Table of Contents
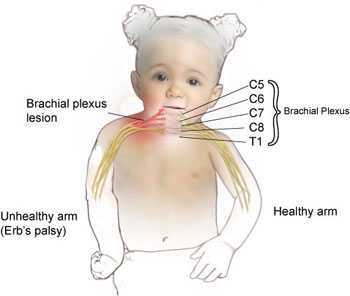
What is Erb’s palsy?
- Erb’s palsy also known as Erb’s Duchenne palsy is a paralysis of the arm(Upper Limb).
- This injury occurs mainly due to injury to the upper group of the arm’s main nerves, The lesion is usually at the junction of the C5 and C6 roots (Erb’s point).
- These Nerve Root form part of the brachial plexus, forming the ventral rami of spinal nerves C5–C8 & One thoracic nerve T1.
- Erb’s palsy occurs most commonly in children, but not exclusively, from shoulder dystocia during a difficult birth.
- According to the nature of the damage, the paralysis can either resolve on its own over months, with necessary physiotherapy treatment or Severe Injury may need surgical intervention.
What is the difference between Klumpke’s palsy & Erb’s palsy?
Anatomy of brachial plexus:
- The brachial plexus is made from five nerves that originate in the spinal cord at the neck.
- The plexus connects these 5 nerves with the nerves that provide sensation to the skin &permit movement in the muscles of the arm & hand.
- There is a brachial plexus have both sides of the body.
- Each of the 5 nerves in the brachial plexus has an important role, such as carrying sensory information from the hand to the brain or powering the muscles. Because each nerve has its own function, the location of the nerve injury within the plexus is give information about outcomes & helps in planning the treatment.
- The brachial plexus has five anatomic sections, & injuries to the brachial plexus can occur in one or more of these areas.
- Spinal nerves
- Trunks
- Divisions
- Cords
- Branches
- These are build-ups of the anterior primary rami of spinal nerves C5,6,7,8 & T1 with contributions from the anterior primary rami of C4 &T2.
- The origin of the plexus may shift one segment either downward or upward resulting in a pre-fixed plexus or post-fixed plexus respectively.
- In a prefixed plexus, the contribution by C4 is more & T2 is often absent.
- In a post-fixed plexus, the contribution by T1 is more, & T2 is always present, C4 is absent, &C5 is less in size.
- The roots join to form trunks are:
- Trunks:
- The upper trunk is made up of C5 and C6.
- The middle trunk is made up of C7
- The lower trunk is made up of C8 & T1
- Divisions (of the trunk)
- Each trunk divides into dorsal & ventral divisions (which ultimately supply the posterior & anterior aspects of
- the limb).
- These divisions join to form cords.
- Cords (it forms 3 cords):
- The Posterior Cord is made by three posterior divisions of the trunks (C5-C8, T1)
- The Lateral Cord is the anterior division from the upper & middle trunks (C5-C7)
- The Medial Cord is a persistence of the anterior division of the lower trunk (C8, T1)
Mechanism of injury in Erb’s palsy:

- The most common cause of Erb’s palsy is excessive lateral traction or stretching of the baby’s head & neck in opposite directions during delivery usually associated with shoulder dystocia.
- This may occur during delivery of the head, the head may have deviated away from the axial plane. There can also be compression of the brachial plexus causing it to stretch & tear.
- Sometimes, pulling on the infant’s shoulder during delivery or excessive pressure on the baby’s raised arm during a breech delivery can lead to brachial plexus injury.
- Two main forces act on the brachial plexus during labor- a natural expulsive force of the uterus, and a traction force applied by the obstetrician.
- Injury to the brachial plexus can happen in many types ways. These include the road traffic accident, contact sports,
- motor vehicle accidents, or during birth.
- Majorly it can be divided into:
- Traumatic :
- e.g. contact sports, motor vehicle accident
- Non-traumatic:
- e.g.obstetric palsy& Parsonage-Turner Syndrome
- The network of nerves is fragile & can be damaged by pressure, stretching, or cutting.
- Stretching can occur when the head & neck are forced away from the shoulder, such as might happen in a fall from a motorcycle. If severe the nerves can avulse or tear out of their roots in the neck.
- Pressure could happen from crushing of the brachial plexus between the collarbone & first rib, or swelling in this area from injured muscles & other structures.
- Such examples of events are caused by one of two mechanisms that remain constant during the injury.
- The two main mechanisms that can occur are traction & heavy impact.
- These two methods disturb the nerves of the brachial plexus & cause the injury.
- Traction:
- Traction, also known as stretch injury, is one of the mechanisms that cause Erb’s palsy.
- The nerves of the brachial plexus are damaged due to the forced pull by the broadening of the shoulder & neck.
- Traction occurs from more severe movement and causes tension or pull among the nerves.
- Impact :
- Heavy impact to the shoulder is the second most common mechanism of causing Erb’s palsy.
- According to the severity of the impact, lesions can happen at all nerves in the brachial plexus.
- The location of impact also affects the severity of the injury &depending on the location, the nerves of the brachial plexus may be avulsed or ruptured.
- Such forms of impact affect the injury to the brachial plexus is a shoulder dislocation, clavicle fractures, hyperextension of the arm& forearm, & sometimes delivery at birth.
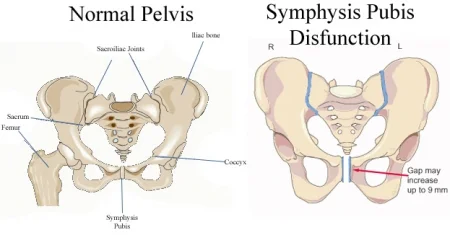
- During the delivery of a baby, the shoulder of the baby is against the pelvic bone of the mother. During this process, the brachial plexus can receive more damage resulting in Erb’s palsy.
Erb’s Palsy Site of injury:
- The site of the upper trunk of the brachial plexus is called Erb’s point. Six nerves meet here. Injury to the upper trunk leads to Erb’s palsy.
- The two conditions are similar in that they’re both injuries that occur to the brachial plexus.
- The nerve damage in Erb’s palsy happens to the upper nerves & affects your arm.
- The nerve damage in Klumke’s palsy happens to the lower trunk.
- The lower brachial plexus nerves affect the muscles in the forearm & the hand.
- Sometimes the hand will have a clawed finger.
- Klumpke’s palsy is also called as Klupmke-Dejerine palsy or paralysis.
Causes of injury:
- Undue separation of the head from the shoulder, which commonly occurs in Birth injury, Fall on the shoulder, During anesthesia
- Nerve roots involved:
- Mainly C5
- Partly C6.
- Muscles paralyzed:
- Mainly biceps, deltoid, brachialis & brachioradialis.
- Partly: supraspinatus, infraspinatus & supinator
- Deformity:
- Arm: Hangs by the side, adducted & medially rotated
- Forearm: Extended & pronated
- The deformity is known as “Policeman’s tip hand” or “Porter’s tip hand”.
- Disability:
- Abduction & external rotation of the arm (shoulder)
- Flexion & supination of the forearm.
- Biceps & supinator jerks are lost.
- Sensations are lost over the lower part of the deltoid
Causes of Erb’s palsy:
- Breech birth: Babies born feet-first are at more risk of Erb’s palsy because their arms are raised and more easily get injured from high pressure.
- Gestational diabetes: If blood sugar is not maintained, the babies have more weight making delivery very difficult.
- Use of birthing tools/improper delivery: During a complicated delivery, a baby may be pulled forcibly & quickly from the birth canal, causing injury to the shoulder & neck.
- Small maternal size/Large infant: Delivery becomes more problematic if the infant has larger than normal or if the mother is particularly petite.
- Second stage of labor lasting over an hour: A long-lasting “pushing” stage may put an infant at more risk of Erb’s palsy.
- Injury: Trauma to the arm or the shoulder leads to Klumpke’s palsy.
- Cancer: A history or risk factor for cancer have more risk of Erb’s palsy.
What causes Erb’s palsy occurs (brachial plexus injuries) in adults?
- Traffic accidents, most often those involving motorcycles, are the most common cause of brachial plexus injuries or Erb’s palsy in teenagers & adults.
- Other causes of these injuries include knife or gunshot wounds, industrial accidents, and accidents related to contact sports like football, surgical complications, or tumors. These types of injuries are more likely to occur in men.
What are the signs & symptoms of Erb’s palsy?
- Erb’s palsy affects the shoulder, arm, and elbow. In general, hand muscles aren’t affected, but hands may experience tingling or
- numbness.
- Signs & symptoms of Erb’s palsy include:
- Immediate symptoms of Erb’s Palsy:
- Since the damage that leads to Erb’s palsy usually occurs during birth, the results are mostly seen immediately. This means that treatment can start immediately to give a newborn the best prognosis.
- Paralysis of one arm, it may be partial or complete
- Weakness in one arm
- Numbness in one arm
- The arm hangs by the side
- Shoulder in internal rotation, Elbow in extension & the forearm pronated with the Palm facing backward.
- Loss of feeling in the arm
- Partial or total paralysis of the arm
- Poor reflexes:
- Babies are born with certain inherent reflexes. A decrease or loss of the normal reflexes in one arm may be a sign of Erb’s palsy.
This predictable movement is called the Moro reflex& it should be symmetrical. - Positioning the arm abnormality:
- Another sign of Erb’s palsy, mostly seen in newborns, is an awkward positioning of the affected arm. The infant may hold its arm extended downward & rotated in toward the body, which does not appear normal. This abnormal positioning of the arm is readily apparent &most commonly seen in these cases, but any placement of the arm seems unnatural and could indicate Erb’s palsy.
- Poor grip strength:
- Damage to the brachial plexus affects a baby’s ability to grip objects. If you put something in a baby’s hand, like your finger, it should be able to grasp it & hold on pretty tightly. A symptom of Erb’s palsy is a grip in one hand with a weaker or no grip in the other. This is a relatively easy test & one that can quickly indicate nerve damage.
- Loss of sensation:
- A newborn cannot tell that it has no feeling in sensation or cannot move one arm, but these are main symptoms of Erb’s palsy. This is why it is important to find other, more noticeable symptoms so that the condition can be detected early & treated.
- Lack of movement:
- One of the first signs that a doctor or new parent may find in an infant is a lack of movement or weakness in the affected arm. Although motor control is mild in newborns, infants move their arms around right after birth. If one arm is moving &the other is not, it is likely a sign of Erb’s palsy. The lack of movement may be mild or excessive, ranging from a limited range of movement at the shoulder to no movement at all.
- Injury to the 5th cervical root alone results in weakness or the loss of shoulder: abduction & external rotation, elbow flexion, and, Forearm supination &the involvement of the sixth cervical root leads to the loss of wrist extension.
Symptoms of Erb’s Palsy in Adults & Children:
- Most cases of Erb’s palsy are in seen newborns & are generally due to difficulties associated with childbirth.
However, damage to any part of the brachial plexus can happen later in life from other types of injuries or accidents. Car accidents, sports injuries, & even tumors can cause damage to the brachial plexus. - Symptoms of this may include:
- A burning sensation like an electric shock that goes down the arm
- weakness or numbness in the arm
- paralysis
- pain
- The limpness of the shoulder, arm & elbow.
- The child cannot lift the arm away from the body or bend her elbow.
- Numbness or tingling in your arm or hand. These are also called “stingers & burners”.
- A hand position is called ‘the waiter’s tip’ position.
- The palm of your hand points toward the back, & the fingers curl.
Diagnosis of Erb’s palsy:
- A thorough history & physical examination with a focus on neurologic examination are used to confirm the diagnosis.
- History- to gather information about pregnancy complications either by maternal obesity, gestational diabetes, fetal macrosomia, prolonged second-stage labor, shoulder dystocia, and use of assistive techniques-forceps to aid delivery.
- Physical examination- most often shows the mild or absent movement of the affected arm.
- Neurologic examination– Detect muscle power, sensation, reflexes- Moro reflex is absent on the affected arm.
Investigations of Erb’s palsy:
- X-rays of the chest – to diagnose the clavicular or humeral fracture
- MRI of the shoulder– may demonstrate shoulder dislocation; the presence of pseudomeningoceles indicates avulsion injury of the affected spinal roots
- CT Scan of the shoulder- may detect shoulder dislocation; the presence of pseudomeningoceles indicates avulsion injury of the affected spinal roots
- EMG/Nerve conduction studies- These tests measure how well individual nerves can give an electrical signal from the spinal cord to the muscles. presence of fibrillation potentials indicates denervation.
Differential diagnosis of Erb’s palsy:
- Klumpke’s injury
- Clavicular fracture
- Cervical ribs
- Osteomyelitis of the humerus or clavicle
- Septic arthritis of the shoulder
Complications of Erb’s palsy:
- Decreased strength and stamina
- Abnormal movement and function of joints
- Muscular atrophy
- Impaired bone growth
- Osteoarthritis
- limb length discrepancy
- Impaired balance& coordination
- Distal ulnar nerve entrapment
- Thoracic outlet syndrome
- Apical lung tumor
- Neurofibroma
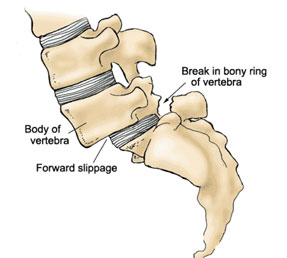
- Disc herniation
- Shoulder impingement
- Clavicular or vertebral fracture
- Others
How can reduce the risk of the newborn having Erb’s palsy?
- There are some risk factors related to shoulder dystocia (a baby’s shoulder being stuck inside the mother’s pelvis, which is related to Erb’s palsy).
- These factors include:
- High infant birth weight & gestational parent with obesity or overweight.
- Gestational parents have diabetes (either diabetes that was there before pregnancy or gestational diabetes).
- A previous pregnancy involving shoulder dystocia.
- Being pregnant with more than one baby.
- Take medicines like oxytocin or an epidural during labor.
- Breech birth position of the baby (your baby isn’t head-first in the birth canal).
How can an adult decrease their risk for Erb’s palsy?
- You can decrease your risk of developing a brachial plexus injury by wearing protective equipment if you want to participate in contact sports or riding motorcycles.
Treatment of Erb’s palsy:

- Because most newborns with Erb’s palsy recover on their own, the doctor will re-examine the child frequently to see if the nerves are recovering. Nerves grow & recover very slowly; it may take up to 2 years for a complete recovery.
- Nonsurgical Treatment:
- Daily physical therapy is the best treatment method for Erb’s palsy. Because a baby can’t take the affected arm all alone, parents must take an active role in keeping the joints activated & the functioning muscles fit. The physical therapist will teach you how to do exercises with the baby to maintain your baby’s arm in good condition.
- Daily physical therapy & range of movement exercises, done as often as possible during the day, begin when a baby is about 3 weeks old. The exercises will maintain the range of motion in the shoulder, elbow, wrist, & hand. This will avoid the joint from becoming permanently stiff, a condition called “joint contracture”.
- Surgical Treatment:
- If there is no change over the 1st three to six months, your doctor may suggest surgery on the nerves to improve the potential outcome.
- Microsurgery:
- In microsurgery, surgeons often use high-powered microscopes & small, specialized instruments. Nerve surgery does not restore full, normal function, and is usually not helpful for older infants.
- Tendon transfers: To assist the muscles that are affected by nerve damage provide work better. To improve the ability to raise the arm, a functioning tendon is moved from its normal attachment in the body & reattached in the shoulder area.
- Muscle transfer: A less important muscle or tendon is removed from other parts of the body and attached to the injured arm if the muscles there are damaged.
- Nerve graft. Depending upon the nerve injury, repair a rupture by “splicing” a donor nerve graft from another nerve of the child.
- Nerve transfer. In such cases, it may be possible to restore some function in the arm by using a nerve from another muscle as a donor. Nerves recover very slowly, it may take more months, or even years, for nerves repaired at the neck to reach the muscles of the lower arm & hand. After surgery, your physical therapist will give rehabilitation exercises to perform at home to improve your baby’s strength & range of motion.
- Other Procedures:
- Other surgical options for treating Erb’s palsy may include:
- Release of joint contractures
- Thickened soft tissues around the shoulder & elbow joints can be released to allow more motion.
Medical treatment of Erb’s palsy:
- Treatment of Erb’s injury in babies and children is heavily dependent on the severity of the injury.
- Medications:
- Erb’s palsy often causes pain & burning sensation. Physicians mostly prescribe medications to relieve these mild Erb’s palsy pain, including topical ointments and prescription medicines.
- Immobilization:
- The affected arm may be immobilized across the body for seven to ten days.
- For minimal cases, gentle massage of the arm and range-of-motion exercises may be suggested.
- For ruptured nerves (avulsion & rupture injuries), symptoms may improve with surgery.
Physiotherapy treatment of Erb’s palsy:
- During the first six months treatment is focusing on the prevention of fixed deformities. Exercise therapy should be administered daily to maintain range of motion & improve muscle strength.
- Parents must be taught to take an active role in maintaining ROM; keeping the functioning muscles fit.
- Exercises should include bimanual or bilateral motor planning activities. Initial treatment in the first one to two weeks after birth will consist of careful handling is required; extremes of motion are avoided for the first, one to two weeks to allow for the initial inflammatory response to the injury to calm.
Aims of physiotherapy treatment :
- Physical therapy also keeps muscles and joints working smoothly; decreases stiffness in joints such as the shoulder, wrist & elbow.
- To improve flexibility
- To improve strength and dexterity
- Development of muscle strength, flexibility, stamina, and coordination.
- Maintaining range of motion via passive movements, stretching, splinting and positioning, and protection of denervated dermatomes.
- Functional training & adoption of adaptive devices if required.
- Pain control via acupuncture and TENS.
- Sensory stimulation gives to increased awareness of the arm.
- Electrical Stimulation is also useful for weak muscles.
- Exercises to improve range of motion in the joints to prevent stiffness & pain.
- Managing chronic edema via education, compression garments & massage therapy.
- Physiotherapy interventions like constraint-induced movement therapy, kinesiotape, electrotherapy, and the use of splints or orthotics have been beneficial for the affected upper limb.
Techniques of physiotherapy treatment:
- Passive and active stretching:
- A physical therapist will assist the child’s arm; the child in performing gentle stretches to improve joint flexibility (range of motion)& prevent or delay contractures (tightening) in the arm.
- Improving strength:
- The physical therapist will teach; your child exercises and play activities to maintain or increase your arm strength. The therapist will identify games; fun tasks that promote strength without asking the baby to work too hard. As your child improves &; grows, your physical therapist will identify new games; activities that will continue to strengthen the arm &; hand.
- Thermotherapy:
- Thermotherapy can be applied before the exercises to decrease stiffness.
- NMES:
- Electrical stimulation can be given as an adjunct with the exercises to re-educate the muscles & nerves.
- Splinting:
- An airplane splint or abduction splint can be used to avoid a soft tissue contracture.
- Massage:
- Mild & gentle massage is given to the affected arm to increase circulation, sensory stimulation, & decrease tightness.
- PROM exercises:
- Passive range of motion exercises is useful to prevent the formation of contractures. The exercises are useful to maintain the range of movement in the joints to prevent stiffness and pain. Involved muscle groups can be exercised & re-educated.
- PNF technique:
- The involved muscles are activated by assisted active movements with sensory stimulus. Bilateral symmetrical PNF patterns may be used to achieve irradiation from the normal contralateral limb or the surviving strong muscles of the affected limb.
- Strengthening exercises:
- Strengthening exercises with weights & resistance can be used for muscle strengthening.
- Hydrotherapy exercises:
- These exercises help to build up the joint movement and strength by assisting in the motion and also using water resistance for strengthening.
- Other activities:
- Crawling, climbing, swimming, & throwing activities can be included in the treatment session.
- Use of modalities:
- A physical therapist uses a variety of intervention techniques (modalities) to increase muscle function & movement.
- Electrical stimulation is given to carefully simulate the nerve signal to the muscle. Flexible tape can be applied over such muscle areas to assist in proper muscle movement or provide relaxation.
- Constraint-induced movement therapy (CIMT) is applied to the nonaffected arm to gently limit its use & encourage the use of the affected arm. A physical therapy session in the pool may help with stretching & strengthening. Repetitive training of the affected arm is increased, using age-appropriate tasks, such as building a tower, finger painting, or picking up and eating small bites of food.
- Improving developmental skills:
- A physical therapist will help a child learn motor skills, like putting the child’s weight on the injured limb, sitting up with arm support, and crawling. physical therapists will give a personalized plan of care that is appropriate based on your child’s specific needs.
- Fostering physical fitness: A physical therapist will help you determine the exercises, diet, and community involvement that will provide good health throughout childhood. the physical therapist will continue to work with you & your child to determine any adaptations that may be needed, so that child can participate fully in family life and society.
Teach the parents how to handle the patient?
- Teach the parents and caretakers to grip the child with gentle care. playing with a child so improves motor as well as sensory function.
- The clothes are comfortable for the child.
- When the child is crying handle with peacefully & calmly.
- Avoid picking a child up under the armpit or arm. This can compress or stretch the brachial plexus & cause further injury.
- Placing a child on side-lying or on the back, with the affected limb is up, to avoid compression of the injured limb. Put the affected hand into the sleeves before the unaffected hand. This will help to neglect extreme movement at the shoulder &arm; will help make dressing quicker & easier.
Home exercises for Erb’s palsy:
- Encourage the parents to carry out specific exercises with their child two to three a day in the comfort of their own home although the exercises can be carried out anywhere appropriate & comfortable.
- The Home Exercise Programme focuses on the following:
- Improve movement at the joints.
- Ensuring that the joints of the affected limb, especially the shoulder, elbow, and wrist keep their full range of movement & avoid excessive shortening of the muscles is also known as a contracture. This will include assisted, passive &active exercises.
- Increase the strength of muscles in the affected limb.
- Improving the child’s awareness of the arm through tactile touch & contact.
- Teach parents, carer takers &the child how to handle the affected limb & how to position it for both comfort, prevention of complications, and practicality.
Prevention of Erb’s palsy:
- The risk of Erb’s palsy can be decreased by:
- Advanced planning: If the baby is larger than normal or in the incorrect position in the weeks leading up to the due date, advanced planning by the obstetrician to prevent Erb’s palsy should include ensuring qualified doctors are present in the delivery room, proper use of birthing instruments&extractors; induction of labor or Cesarean delivery if several risk factors are identified.
- Maternal healthcare: Good maternal healthcare during pregnancy, including avoidance or control of diabetes, can use to prevent Erb’s palsy.



3 Comments