Cohen syndrome
Table of Contents
What is cohen syndrome?
- Cohen syndrome is an hereditary syndrome that affects many parts of the body and is characterized by developmental delay, mental disability, microcephaly, hypotonia.
- Cohen syndrome is also called as Pepper syndrome or Cerenkov syndrome or Prominent incisors-obesity-hypotonic syndrome or Norio syndrome.
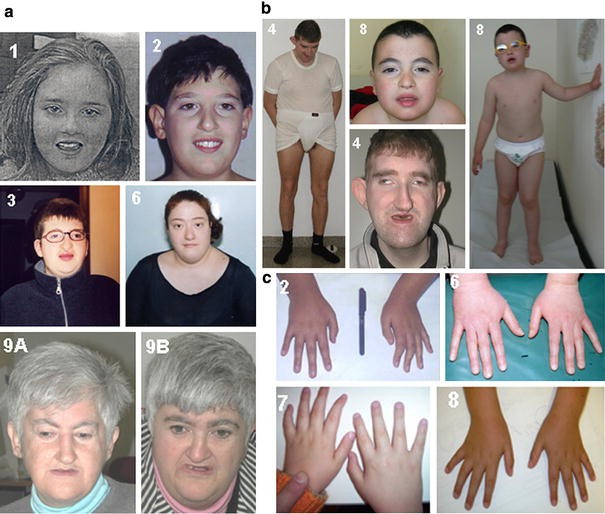
- Other features common in this condition include worsening myopia, breakdown of the light-sensitive tissue at the back of the eye (also known as retinal dystrophy), an unusually large range of joint movement (also known as hypermobility), and distinctive facial characteristic.
- These facial characteristic typically include thick hair and eyebrows, long eyelashes, unusually-down-slanting and wave-shaped, a bulbous nasal tip, a smooth or shortened area amid the nose and the upper lip, and prominent upper central teeth. The combination of the last two facial characteristic results in an open mouth.
What are the symptoms?
- The features of Cohen syndrome very broadly among affected individuals.
- Additional signs and symptoms in certain individuals with this disorder include low levels of white blood cells (also known as neutropenia), overly friendly behavior, and obesity that develops in young children or adolescence.
- When obesity is present, it typically occurs around the body, with the arms and legs remaining slender (called as trance obesity).
- Human beings with Cohen syndrome may also have short hands and feet, and slender fingers.
- This condition is hereditary in an autosomal recessive pattern, which means both copies of the gene in each cell have variants. The parents of an with an single autosomal dominant gene condition each carry one copy of the parented gene, but they typically don’t show signs and symptoms of the cohen syndrome.
What are the frequency?
- The exact occurrence Cohen syndrome is unknown. It has been identified in less than 1,000 people worldwide.
- Most of cases are likely undiagnosed. It is appear frequently in a small Amish community in Ohio, where it affects an approximated 1 in 500 people. It is too more common in Finland
What is the causes of Cohen syndrome?
- This syndrome is caused by pathogenic mutations in the VPS13B gene at chromosomal locus 8q22.
- [1] It has an autosomal recessive transmission with changeable expression.
- [2] Variants in VSP13B also cause Mirhosseini–Holmes–Walton syndrome, which is now contemptible to be the same being as Cohen syndrome.
Cohen syndrome should be suspected in individuals with the following findings 12:
1.Retinal dystrophy appearing by mid-childhood
2.Progressive high myopia
3.Acquired microcephaly
4.Non-progressive intellectual disability and global developmental delay
5.Hypotonia
6.Joint hypermobility
7.Typical Cohen syndrome facial gestalt: thick hair and eyebrows, long eyelashes, wave-shaped
8.palpebral fissures, broad nasal tip, smooth or short phylum, and hypotonic appearance
Short stature
9.Small or narrow hands and feet
10.Truncal obesity appearing in or after mid-childhood
11.Friendly disposition
12.Neutropenia
Cohen syndrome cardinal features 8:
1.Retinal dystrophy and high myopia
2.Microcephaly
3.Developmental delay
4.Joint hypermobility
5.Typical Cohen syndrome facial gestalt
6.Truncal obesity with slender extremities
7.Overly sociable behavior
8.Neutropenia
What is the diagnosis?
- Cohen syndrome is diagnosed by the clinical examination but is often difficult due to difference in expression.
- Ocular complications, very rare conditions are listed as optic atrophy, microphthalmia, and pigmentary chorioretinitis, hemeralopia (also known as decreased vision in bright light), myopia, strabismus, nystagmus and iris/retinal coloboma.
- General appearance is the obesity with thin or elongated arms and legs.
- Micrognathia, short phylum and high vaulted palate are common. Changeable intellectual disability with the occasional seizure and deafness also is characteristic of Cohen syndrome.
How is Cohen syndrome treated?
- There is not any treatment for Cohen syndrome, but early intervention with physical, occupational, and speech therapy can address symptoms like as,
- joint laxity
- clumsiness
- developmental delays
- Children with nearsightedness need glasses, while those with retinal degeneration useful effect from training for the visually impaired.
- In order to cure recurrent infections, people with Cohen syndrome should be monitored throughout their inhabit for a low white blood cell count.
- The treatment is straight toward the specific symptoms that are apparent in each individual.
- Treatment may need the coordinated efforts of a team of specialists.
- Pediatricians, pediatric neurologists, orthopedists, ophthalmologists, psychiatrists, speech pathologists, and other doctors may need to systematically and comprehensively plan an affected child’s treatment.
- Genetic counseling is better for affected individuals and their families.
- Treatment options that may be used to treat individuals with the Cohen syndrome are compounded and varied.
- The exact treatment plan will need to be highly individualized.
- Decisions concerning the use of specific treatments should be made by physicians and further members of the health care team in careful consultation with an affected child’s parents or with an adult patient based upon the specifics of his/her case a thorough discussion of the potential benefits and risks, having possible side effects and long-term effects; patient preference; and other suitable factors.
- Early developmental intervention is necessary to ensure that affected children reach their potential.
- Most affected children will useful from occupational, physical and speech therapy.
Physical therapy important for the prevent symptoms.
Like, hypotonic prevent by the exercises.
We have to prevent hypotonic by the ROM exercises.
We have to increase ROM by the repetitive passive exercise, active exercise, gait training, and balance training, etc.
As a physiotherapist, we have to prevent pain and inflammation.
- Various methods of rehabilitative and behavioral therapy may be advantagable.
- Additional medical, social &/or vocational services including special remedial education may be
- obligatory.
- Psycho-social support for the entire family is important as well.
- Specific treatments for this disease include spectacles or eyeglasses to help with vision.
- In later years, low vision training as useful in individuals with visual impairment.
- Recurrent infections can be handled with standard therapies including antibiotics.
- In some examples, neutropenia may be treated with the administration of granulocyte-colony stimulating factors.
- G-CSF is a manufactured form of the natural hormones that stimulate the bone marrow to produce neutrophils.
- G-CSF is growing the number of neutrophils generated by the bone marrow.
What Is the Prognosis for a Person with Cohen Syndrome?
- The correct effect of Cohen syndrome on one’s lifespan is unclear.
- Some people with the disease are noted to be alive in their fifties.




My youngest daughter was just diagnosed with Cohen syndrome > she was a destress birth 07-02-1983
Didnt know what caused her disabilities till several weeks ago. Her saliva test results came back with the
results of Cohen. She is moderate with her disabilities, Eyes ,Teeth ,Height , Feet, lax mussels, and learning disabilities. She retains what she wants to place her own values on.
With optic nerve damage due to Oxygen deprivation at birth and retinitis Pigmatoses her vision is limited. Over the last year it remains stable.
Would be interested to know if there are any study’s or further research anywhere ,