Cervicogenic Headache Physiotherapy Treatment :
Table of Contents
Definition:
Cervicogenic Headache (CGH) is a chronic headache that arises from the atlanto-occipital and upper cervical joints and seen in one or more regions of the head, Neck and/or face.
Introduction:
Cervicogenic headaches can mimic migraines, so it may be difficult to distinguish a cervicogenic headache from a migraine headache. The primary difference is that a migraine headache is rooted in the brain, and a cervicogenic headache is rooted in the cervical spine or base of the skull region.
Some headaches are caused by eyestrain, stress, tiredness, or trauma. Cervicogenic headaches are different because they are caused by problems with the nerves, bones, or muscles in your neck. Although it may feel pain in your head, the pain you feel is referred pain from another location in your body.
CLINICAL ANATOMY :
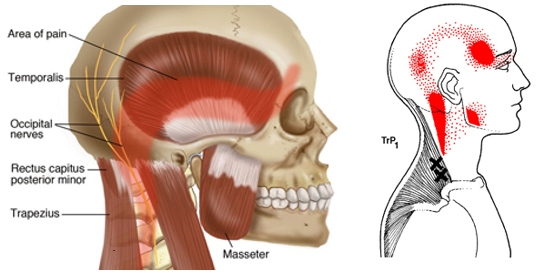
The cervical spine consists of 7 vertebrae, C1 to C7, the cervical nerves from C1 to C8, muscles and ligaments.
The first two vertebrae have a unique shape and function.They form the upper cervical spine.
The upper vertebrae supports the skull (atlas/C1), articulates superiorly with the occiput (the atlanto-occipital joint) . This joint is responsible for 33% of flexion and extension.The design of the atlas allows forward and backward movement of the head. Below the atlas is the axis (C2) that allows rotation.[3] The atlantoaxial joint is responsible for 60% of all cervical rotation. The 5 cervical vertebrae that make up the lower cervical spine, C3-C7, are similar to each other but very different from C1 and C2.

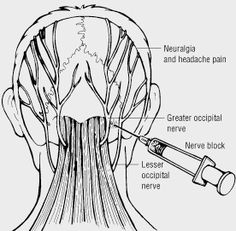
SPINAL NERVES:
Certain spinal nerves structures are involved in many cervicogenic headaches. Spinal nerves are signal transmitters that enable communication between the brain and the body via the spinal cord. At each level of the cervical spine is a set of spinal nerves; one on the left side and one on the right of the spine. C1, C2 and/or C3 may be involved in development of cervicogenic headaches because these nerves enable function (movement) and sensation of the head and neck. Nerve compression can cause inflammation and pain.
PATHO-PHYSIOLOGY :
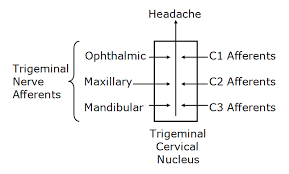
Cervicogenic headaches are a form of referred pain – meaning that although the source of the pain is in the cervical spine, the sensation of pain is felt in the head as a headache. This happens because there are nerves in the upper cervical region (C1, C2, and C3) that have connections to nerves of the head (cranial nerve V via the trigeminal nerve spinal tract).
Although some controversy exists, a vast majority of the literature agrees that the most common cause of cervicogenic headaches is dysfunction from the C2-3 zygapophysial joints (facet joints).12 However, there is also literature to support that cervicogenic headaches can arise from dysfunction in the C2-3 and C3-4 intervertebral discs of facet joints, as well as the atlantoaxial (C1-2) and atlanto-occipital (C0-1) joints.
Which are the Causes of Cervicogenic Headache ?

The cause of a cervicogenic headache is often related to excessive stress to the neck. The headache may result from cervical spondylosis, a damaged disc, or whiplash-type movement that irritates or compresses a cervical nerve or sometimes over-activity of neck muscles also cause spasm of Para-spinal neck muscles which also leads to Cervicogenic Headache.
The neck’s bony structures (eg. facet joints) and its soft tissues (eg. muscles) can contribute to the development of a cervicogenic headache.
Medical conditions that can cause cervicogenic headaches are :
- Tumors in Cervical area
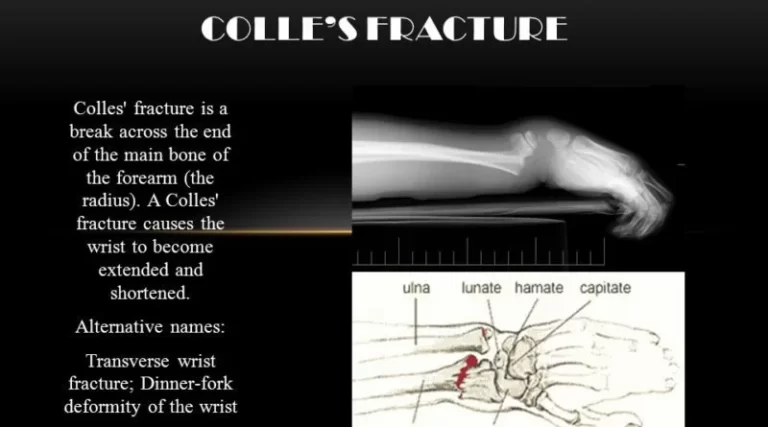
- Fractures
- Infections
- Poor Posture
- Cervical Disc Prolapse
- Arthritis of the upper cervical spine ( Cervical Spondylosis )
- Whiplash or another injury to the neck
SYMPTOMS :
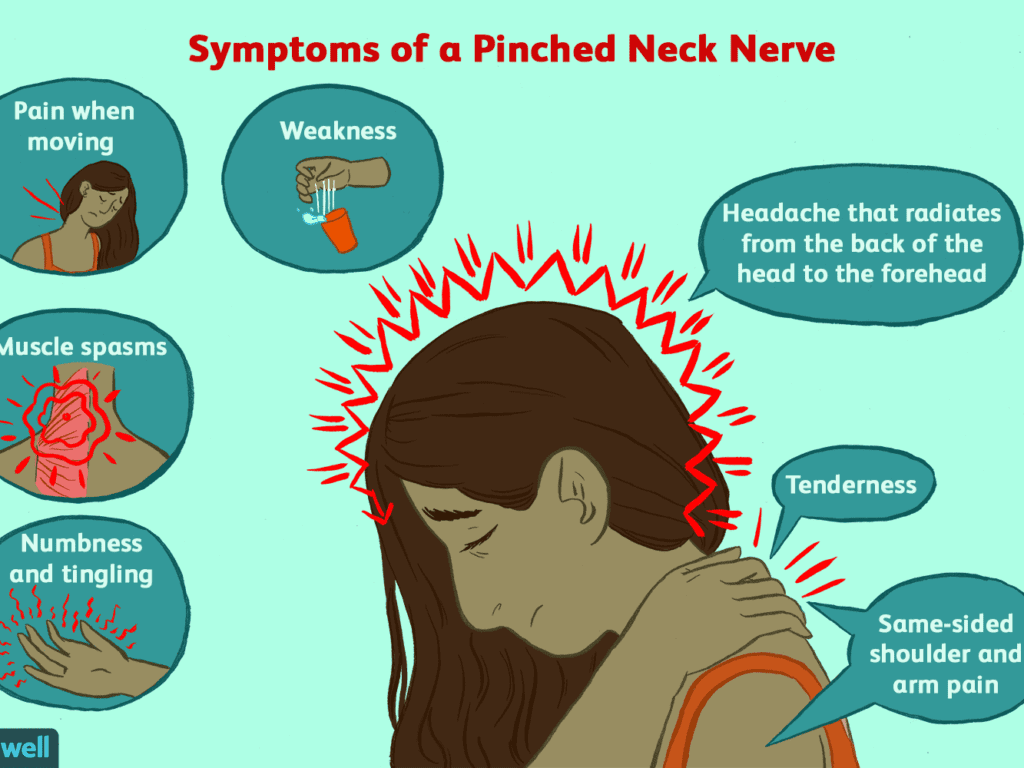
Symptoms of a Cervicogenic headache may include:
- a reduced range of motion in the neck
- pain on one side of the face or head
- pain and stiffness of the neck
- pain around the eyes
- Spasm of Paraspinal Neck Muscles
- Radiating Pain to Upper trapezius upto shoulder and arm area.
- pain in the neck, shoulder, or arm on one side
- pain while coughing or sneezing
- head pain that is triggered by certain neck movements or postures
- throbbing head pain
- sensitivity to light and noise
- Weakness in the deep neck flexors
- Tenderness in Upper Cervical area
- nausea
- blurred vision
- Poor Posture
RISK FACTORS:

Risk factors that may be involved in headache onset or aggravate cervicogenic headaches include:
- Fatigue
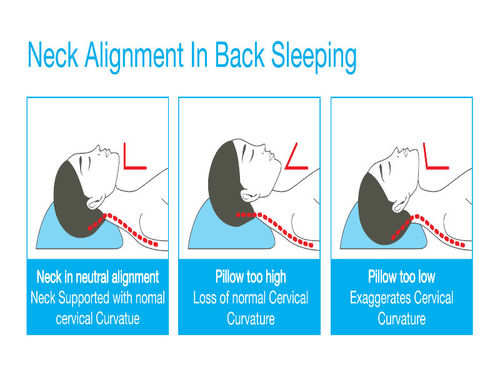
- Sleep difficulties
- Cervical disc problems
- Current or prior neck injuries
- Poor posture (High cell phone use)
- Muscular stress
Differential Diagnosis:
It is important to differentiate from serious pathology such as:
- Vascular Pathologies of the Neck
- Intracranial Pathology
- Cervical Instability
- Cervical Myelopathy
- Occipital neuralgia
Physical Examination:

Pain localized in the neck and occiput, which can spread to other areas in the head, such as forehead, orbital region, temples, vertex, or ears, usually unilateral.
Pain is precipitated or aggravated by specific neck movements or sustained postures.
At least one of the following:
- Resistance to or limitation of passive neck movements
- Changes in neck muscle contour, texture, tone, or response to active and passive stretching and contraction
- Abnormal tenderness of neck musculatur
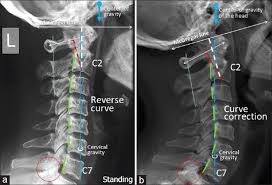
Radiological examination reveals at least one of the following:
- Movement abnormalities in flexion/extension
- Abnormal posture
- Fractures, congenital abnormalities, bone tumors, rheumatoid arthritis, or other distinct pathology (not spondylosis or osteochondrosis)
Flexion-Rotation Test :

others tests are:

- X-ray: Small doses of radiation are used to make pictures of the bones in your neck and spine.
- Computerized tomography (CT) scan: Several X-rays are taken from different angles and put together to show more information than is on a single X-ray.
- Magnetic resonance imaging (MRI) scan: Powerful magnets and radio waves are used to make detailed images of your head, neck, and spine.
Medical Management:
There are several ways to lessen the pain, or get rid of it completely:
- Medicine: Non-steroidal anti-inflammatory (aspirin or ibuprofen), muscle relaxers, and other pain relievers may ease the pain.
- Nerve block: This may temporarily relieve pain and help you better work with physiotherapy.
- Spinal manipulation: This is a mix of physiotherapy, massage, and joint movement. It should only be done by a physiotherapist, a chiropractor, or an osteopath (a doctor who has special training in the way your nerves, bones, and muscles work together).
- Other options: Non-surgical ways to deal with the pain include relaxation techniques, such as deep breathing , yoga, and acupuncture.
Physiotherapy management:

- Cervical spine manipulation or mobilization
- Strengthening exercises including deep neck flexors and upper quarter muscles
- Thoracic spine thrust manipulation & exercise
- C1-C2 Self-sustained Natural Apophyseal Glide (SNAG)shown to be effective for reducing cervicogenic headache symptoms
- active mobilization exercises
- upper cervical spine mobilizations
- passive mobilization with movement
- work-related ergonomic training
- active mobilization with movement
- Thoracic Manipulation Deep Neck Flexor Exercise
Retraining the cervical flexors for anti-gravity function in sitting position:

- The exercise is a controlled eccentric action of the flexors into cervical extension range followed by a concentric action of these muscles to return the head to the neutral upright position. The return to the upright position must be initiated by CCF, rather than a dominant action of sternocleidomastoid.
- The exercise is progressed by gradually increasing the range to which the head is moved into extension as control improves, and introducing isometric holds through range.
Extensors of the Craniocervical Spine:
The patient practices eccentric control of the head into flexion followed by concentric control back to the neutral position in a 4 point kneeling position to train the coordination of the deep and superficial cervical extensors. These exercises are incorporated with re-education of the scapular muscles in these positions and are commenced early in the program. The exercise is progressed by performing alternating small ranges of craniocervical extension and flexion while maintaining the cervical spine in a neutral position. Co-contraction of the neck flexors and extensors.

Co-contraction of the Neck Flexor’s and Extensor’s :
The co-contraction is facilitated with rotation and the exercises are introduced once the patient can activate the deep muscles. The patient uses self-resisted isometric rotation in a correct upright sitting posture. They look into the palm of the hand, providing the resistance to facilitate the muscles and perform the alternating rhythmic stabilization exercises with an emphasis on slow onset and slow release holding contractions, using resistance to match about a 10–20% effort. Retraining the strength of the superficial and deep flexor synergy
Retraining the Strength of the Superficial and Deep Flexors Synergy :

The head lift must be preceded with CCF followed by cervical flexion to just lift the head from the bed. Gravity and head load provide the resistance. Care must be taken that high load exercise is not introduced too early, as it may be provocative of symptoms.
Retraining the Scapular Muscles :

Retraining scapular orientation in posture correction strategy is to have the patient move the coracoids upward and the acromion backward, which results in a slight retraction and external rotation of the scapula. The aim is to facilitate the coordinated action of all parts of trapezius and serratus anterior, allowing lower trapezius to slightly depress the medial border of the scapula, consequently lengthening (and relaxing) the levator scapulae.
Once the patient learns correct scapular orientation, Training the endurance capacity of the scapular stabilizers Repeated repetitions of 10 second holds of the corrected scapular position encourages early endurance retraining. The endurance of the middle and lower trapezius muscles is also trained by performing an exercise in the prone lying position against the effects of gravity.
Retraining scapular control with arm movement and load This is important when activities such as computer or deskwork aggravate pain. The patient is encouraged to maintain their newly learned scapular position while performing small range (+/- 60 degrees) arm movements, or during, for example, work at a computer. Scapular control in association with control of cervicothoracic postural position is also trained for functional activities such as lifting and carrying.
Upper Quarter Strengthening Exercises
- Lower Trapezius Strengthening
- Middle Trapezius Strengthening
Adding upper quarter exercises for patients with cervical dysfunction is important in order to integrate ‘global’ muscles that have connections to the cervical spine through anatomical chains (most notably those connecting the axial and appendicular skeletons).
Re-education of Posture :
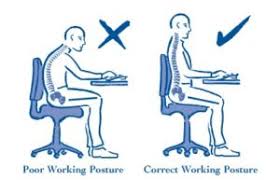
Posture is an indirect measure of the functional status of the neuromuscular system. Postural position is trained in sitting and is corrected from the pelvis. The second aspect of re-education of postural position is the correction of scapular position. Maintenance of a correct scapular position with appropriate muscle coordination has the added benefit of inducing reciprocal relaxation in muscles such as levator scapulae, which reduces muscular pain in the area.
Sensori-motor Training :

Because CGHs are thought to be a dysfunction of the sensorimotor system.Sensorimotor exercises include progressive exercise on unstable surfaces to promote reflexive stabilization and postural stability. Unstable surfaces such as exercise balls or foam pads can be used to add challenge to the cervical spine as well as the whole-body for stabilization exercises. These final stages of the rehabilitation program for CGH patients can be progressed toward functional activities to return the patient to full participation.
Trigger Point Therapy :

This is composed of different manual approaches, for example, compression, stretching, or transverse friction massage. Pressure release over the sternocleidomastoid muscle Trigger Point is applied and pressure is progressively applied and increased over the Trigger point until the finger encountered an increase in tissue resistance (tissue barrier). This pressure is maintained until the therapist sensed a relief of the taut band. At that moment, the pressure is increased again until the next increase in tissue resistance. Stretching of the taut band muscle fibers is also important. This technique has been found to be effective for lengthening the trigger point in the muscle and the associated connective tissue. The therapist apply moderate slow pressure over the Trigger point and slides the fingers in the opposite directions. Trigger point manual therapy is applied slowly and is performed without inducing pain to the patients.
(Myofascial) Mobility, Strength, Stability and Postural Exercises :

These technics were primarily post isometric relaxation procedures (A), myofascial mobilization (B) and selected elements of McKenzie therapy. Exercises were mainly applied to the muscles with Trigger points, showing the pathological increase in rEMG amplitude. When relaxation of painful, tensed muscles is achieved, the next step of treatment include strengthening exercises of the same muscles. All of them are supervised by a physiotherapist. Exercises intensity shall not increase the pain sensation in the cervical spine, shoulder and girdle muscles. They aren’t supposed to evoke the headache.
There are isometric exercises with the gradual loading increase and dynamic exercises. Elastic Thera bands are commonly used during these exercises. Additionally, the self-control exercises of the correct body posture are carried out in front of the mirror relying on the visual feedback.
Prevention Measure :
- Avoiding postures or movements that provoke the pain to start
- Maintaining a good posture while sitting or driving—by sitting tall with shoulders back and without protruding the head forward
- Using a neck brace can be helpful while sitting upright or sleeping in a chair
- Using a supporting travel pillow (similar to a neck brace) on the plane or bus to avoid excessive side-bending or flexion
- Avoiding tummy-sleeping posture
- Finding the right pillow to prevent the head from being too high or too low when sleeping.






i have also taken Physiotherapy treatment and exercise for cervicogenic headache, i have taken nearly 12 session.
Superb article! educative and helpful piece of content many. Keep updating the good article like this. Please add me to your email list so next time if you publish an article like this then I will keep updated about that post.