Bicipital Tendinitis: Physiotherapy Treatment
Table of Contents
What is a Bicipital Tendinitis?
Bicipital tendinitis is an inflammation or irritation of the upper biceps tendon. Also called the long head of the biceps tendon, this strong, cord-like structure connects the biceps muscle to the bones in the shoulder. Pain in the front of the shoulder and weakness are common symptoms of bicipital tendinitis.
Pain in the front of the shoulder and weakness are common symptoms of biceps tendinitis. They can often be relieved with rest and Physiotherapy Exercises and Proper Pain Relieving medication. Physiotherapists examine the exact source of the pain by assessing the entire shoulder and typically describe a program of activity modification, stretching, and strengthening to resolve pain and return individuals to their desired activities. In severe cases, surgery may be needed to repair the tendon.
Bicipital tendinitis usually occurs along with other shoulder problems. In most cases, there is also damage to the rotator cuff tendon. Other problems that often accompany biceps tendinitis include:
- Arthritis of the shoulder joint
- Tears in the glenoid labrum
- Chronic shoulder instability (dislocation)
- Shoulder impingement
- Other diseases that cause inflammation of the shoulder joint lining
Relevant Anatomy:
Shoulder joint is a ball-and-socket joint that is made up of three bones: the upper arm bone (humerus), shoulder blade (scapula), and collarbone (clavicle).
Glenoid. The head of the upper arm bone fits into the rounded socket in the shoulder blade. This socket is called the glenoid. The glenoid is lined with soft cartilage called the labrum. This tissue helps the head of the upper arm fit into the shoulder socket.
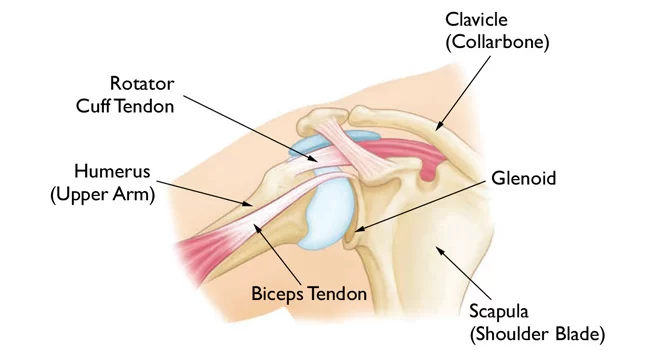
Rotator cuff. A combination of muscles and tendons keeps the arm centered in the shoulder socket. These tissues are called the rotator cuff. They cover the head of the upper arm bone and attach it to the shoulder blade.
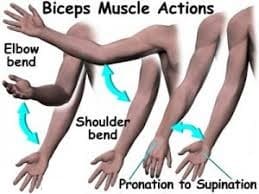
Biceps tendons. The biceps muscle is in the front of the upper arm. It has two tendons that attach it to bones in the shoulder. The long head attaches to the top of the shoulder socket (glenoid).
The short head of the biceps tendon attaches to a bump on the shoulder blade called the coracoid process.
Mechanism of Injury:
As the long head of the biceps tendon rests encased in its synovial sheath within the intertubercular sulcus of the humerus, the transverse humeral ligament covering this sulcus can rupture, causing it to slide back and forth, leading to a wear and tear effect on the long head of the biceps tendon. Repetitive microtrauma (commonly seen in overhead-throwing or racquet athletes) can also lead to inflammation of the tendon. Complete rupture of the tendon can occasionally occur from a state of chronic inflammation or from a traumatic event (such as forceful elbow movements often associated with weightlifting).
Biceps tendonitis has been shown to be associated with rotator cuff tears, particularly those that involve the subscapularis tendon. Additionally, in chronic rotator cuff tears (> 3 months) there most likely will be some degree of macroscopic biceps abnormality. The presence of rotator cuff tears also correlates with biceps tendon dislocations and subluxation.
Overall, biceps tendonitis likely will present with concomitant shoulder pathologies, such as subacromial impingement, rotator cuff tears, instability, or tensile injury. This injury can often lead to rotator cuff injury.
For shoulder pain patients, biceps tendonitis can be one of the numerous etiologies and can accompany other pathologies of the shoulder. the following biomechanical causes for biceps tendinitis are coracoacromial ligament thickening, impingement beneath the coracoacromial arch by a bone spur, and acromial apophysis infusion. These pathologies can lead to biceps tendinitis because of repeated trauma by overuse and improper biomechanical circumstances.
The inflammation process can initially lead to biceps tendon hyperemia and subsequent swelling of the tendon sheath. In the end stage of chronic inflammation, scarring and adhesion of the biceps tendon in the bicipital groove can occur. These symptoms can be obstacles to activities of daily living, and correct diagnosis and early treatment of biceps tendonitis are vital. The most common are partial ruptures. All the patients were noted to have partial tendon rupture with surrounding granulation, and scar tissue was noted at the time of surgery. Complete rupture of the distal biceps tendon from its insertion at the radial tuberosity is the most common.
There are two main theories explaining the possible predisposition of the distal aspect of the biceps to injury. The first deals with the vascular supply of the distal biceps. Proximally, the biceps brachii receive branches of the brachial artery, but the distal vascular supply comes from the smaller posterior interosseous artery. The second theorized predisposition for distal tendon degeneration involves mechanical impingement of the biceps tendon at the proximal radioulnar joint. With the forearm in a fully pronated position, the distance between the lateral border of the ulna and the radial tuberosity is 48%less than the distance with the forearm fully supinated, thus decreasing the available space for the tendon. Also, with the forearm pronated, the biceps tendon occupied on average 85% of the radioulnar space at the level of the tuberosity.
Bicipital tendonitis may be related to shoulder laxity and instability. proximal end of the biceps may be related to traction overload tendinopathy. The biceps long head acts as a humeral stabilizer as well as a decelerator of elbow extension. When there is an increased translation of the humeral head with activities, more stress is placed on the biceps and ligamentous structures. Activities that include repeated shoulder abduction with external rotation such as throwing may result in impingement of the biceps tendon in the bicipital groove beneath the accordion. Some possible causes of discomfort that have been observed with ultrasound include synovitis or effusion of the bicipital groove, mineralization of the transverse ligament, subluxing biceps tendon, and cyst of the tendon.
Tendonitis can also affect the triceps tendons, although these injuries are much less common than medial and lateral epicondylitis. Tendinopathy at both of these sites can often be treated by rest and avoidance of activities that aggravate the athlete’s symptoms. inflammation of these tendons is often due to overuse and does not cause persistent symptoms. rupture of the bicipital tendon is difficult to diagnose and may often be confused with a strain of the elbow of forearm. the injury commonly presents as an acutely painful condition of the elbow. treatment of this injury is surgical. repair should be performed within 7 to 10 days of rupture.
Causes of Bicipital Tendinitis:
Bicep tendonitis occurs when tendons in the biceps become inflamed. This can sometimes be due to microscopic tears.
Causes of bicep tendonitis can include:
- General wear and tear
- overuse of a tendon in a repetitive motion such as swimming, tennis, and baseball — can also put people at risk for biceps tendinitis.
- repetitive overhead motion may play a part in other shoulder problems that occur with biceps tendinitis. Rotator cuff tears, osteoarthritis, and chronic shoulder instability are often caused by overuse.
- poor posture
- lifting something heavy
- poor technique while playing sports
- injury
- shoulder impingement
Symptoms of Bicipital Tendinitis
The most obvious symptom will be sudden, severe pain in the upper part of the arm or at the elbow, depending on where the tendon is injured.
Other signs that may have torn a biceps tendon can include:
- Sharp pain at the shoulder or elbow.
- sometimes, the pain will radiate down up to the elbow or toward the neck
- A bruise appears on the upper arm or forearm near the elbow.
- May get weakness in the shoulder or elbow while performing any overhead or lifting activities
- May get into trouble while rotating the arm from a “palm down” to a “palm up” position.
- snapping” sound may also be heard while moving the shoulder, or a “catching” or “clicking” sensation may be felt A change in the contour of the front of your bicep in the upper arm (“Popeye muscle”).
- Tenderness may present in the front of the shoulder.
Physiotherapy Examination:
After discussing symptoms and medical history, your doctor will examine your shoulder.
During the examination, your doctor will assess your shoulder for range of motion, strength, and signs of shoulder instability. In addition, he or she will perform specific physical examination tests to check the function of your biceps.
Yergason test:

Yergason test requires the patient to place the arm at his or her side with the elbow flexed at 90 degrees and supinate against resistance. The test is considered positive if the pain is referred to the bicipital groove.
Neers test:
involves internal rotation of the arm while in the forward flexed position. If the patient experiences pain, it is a positive sign of impingement syndrome.
Hawkins test:
the patient flexes the elbow to 90 degrees while the physician elevates the patient’s shoulder to 90 degrees and places the forearm in a neutral position. With the arm supported, the humerus is rotated internally. The test is positive if bicipital groove pain is present.
Speed test:
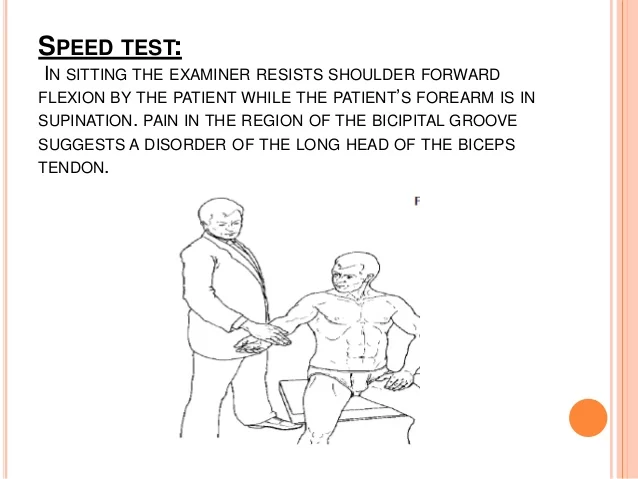
the patient tries to flex the shoulder against resistance with the elbow extended and the forearm supinated. A positive test is a pain radiating to the bicipital groove.
Other tests that may help your doctor confirm your diagnosis include:
- X-ray: Although they only visualize bones, x-rays may show other problems in your shoulder joint.
- Magnetic resonance imaging (MRI) and ultrasound: These images can show soft tissues like the biceps tendon in greater detail.
Different Diagnosis:
Different Diagnosis of Anterior Shoulder Pain
- Acromioclavicular joint pathology
- Adhesive capsulitis
- Cervical spine pathology
- Glenohumeral arthritis
- Glenohumeral instability
- Humeral head osteonecrosis
- Sub-acromial Impingement syndrome
- Rotator cuff tears
- Superior labrum anterior-posterior lesions.
Conservative treatment:
Initial treatment should consist of pain management and reducing inflammation. The mainstays of treatment have included rest and ice, nonsteroidal anti-inflammatory medications such as (NSAIDs), periodic local corticosteroid injections, and corticosteroid injections along the tendon sheath may be indicated.
Physiotherapy Treatment in Bicipital Tendinitis:
This may start with isometric training if the pain is the primary issue progressing into eccentric training and eventually concentric loading as with other forms of tendon rehab. Stretching and strengthening programs are a common component of most therapy programs.
Physiotherapists also use other modalities, including ultrasound, iontophoresis, deep transverse friction massage, low-level laser therapy, and hyperthermia.
The physiotherapist must consider both the patient’s subjective response to injury and the physiological mechanisms of tissue healing; both are essential in relation to a patient’s return to optimal performance.
As a preface to a discussion of the goals of treatment during injury rehabilitation, two points must be made.
First, healing tissue must not be overstressed. During tissue healing, controlled therapeutic stress is necessary to optimize collagen matrix formation, but too much stress can damage new structures and slow the patient’s rehabilitation.
Second, the patient must meet specific objectives to progress from one phase of healing to the next. These objectives may depend on ROM, strength, or activity. It is the responsibility of the physical therapist to establish these guidelines.
The Guide provides two main practice patterns that biceps tendinopathy may fall under:
Pattern 4D: Impaired Joint Mobility, Motor Function, Muscle Performance, and Range of Motion Associated With Connective Tissue Dysfunction
Pattern 4E: Impaired Joint Mobility, Motor Function, Muscle Performance, and Range of Motion Associated With Localized Inflammation
Physiotherapy intervention should include:

- Restoring a pain-free range of motion – Pain-free range can be achieved with such activities as PROM, Active-Assisted Range of Motion (AAROM), and mobilization via manual therapy
- Proper scapulothoracic rhythm.
- Painful activities such as abduction and overhead activities should be avoided in the early stages of recovery as they can exacerbate symptoms.
- A strengthening program consisting of heavy slow loading should begin with an emphasis on the scapular stabilizers, rotator cuff, and biceps tendon.
Exercises to Relieve Pain from Bicipital Tendonitis:
Flexion and Extension:
- Flex and extend the elbow on your injured side by gently bringing the palm of your hand up to the shoulder.
- Be sure to bend the elbow as much as possible. Then straighten your arm and elbow.
- Complete 15 repetitions.
- Rest, and then complete another set of 15 repetitions.
Single Shoulder Flexion:
- Begin by standing with your arms at your side.
- Keeping the injured arm straight, raise it forward and up until it points to the ceiling.
- Hold for about 5 seconds, and then return to the starting position.
- Complete another set with between 8 and 12 raises, holding each raise for 5 seconds.
Biceps Stretch:
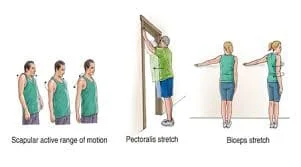
- Face a wall, standing about 6 inches away.
- With your palm down, raise the arm on your injured side and touch the thumb side of your hand to the wall.
- Make sure your arm is straight, and then turn your body away from your raised arm until you feel a stretch in the biceps.
- Hold this stretch for about 15 seconds.
- Rest, and then complete 2 more reps.
- Reclining External Rotation
Prevention:
- Avoid overhead activities
- Avoid repetitive movements
Surgical Treatment
In case that noninvasive treatments are ineffective in improving your condition, your physician may recommend surgery. The operation will probably be done arthroscopically by your healthcare professional. This means that an arthroscope (a small camera) will be put into your shoulder joint in order to capture pictures. These images will be used to guide the use of tiny surgical tools during the treatment.
Surgical options might consist of:
- Biceps tenodesis: Your bicep will be surgically removed, and the tendon that remains will be sewn back to your humerus, the bone in your upper arm.
- Tenotomy: Your injured biceps tendon will be released from its attachment by your surgeon.
What is the duration of healing for Bicipital Tendinitis?
The length of time it takes to recover from biceps tendonitis depends on how severe your condition is and how you manage it. In a few weeks, your condition should become better with noninvasive therapy.
Your recovery period will be longer if you require surgery. Depending on the procedure, your doctor may advise you to wear a sling for one to four weeks. Additionally, you’ll require physical therapy or another kind of rehabilitation. The entire healing process might take three or four months.
Prognosis
Your shoulder region will hurt and feel painful if you have biceps tendonitis. In a few weeks, if conservative treatments such as ice packs, painkillers, and rest don’t help you feel better, your doctor could suggest surgery.
Results from surgery for biceps tendonitis are often favorable. Your arm should be pain-free and able to move through its entire range of motion. You might need to restrict your activities following surgery if you perform sports that require a lot of overhead motions.
When should I visit my medical professional?
Many cases of biceps tendonitis can be resolved with basic treatment, such as rest, ice, and NSAIDs, in a few of weeks. However, you should consult your healthcare professional for additional therapy if your pain prevents you from carrying out your regular daily activities and self-care hasn’t made a difference in your condition.
Additionally, if pain persists in interfering with your ability to do overhead motions during sports, you should consult your physician. Additionally, give your provider a call if you develop a bulge in your upper arm or feel any sudden, acute sensations.
Summary
Hurt! Has the pain in your shoulder/upper arm started recently? It’s possible that you have biceps tendonitis. This painful condition indicates that your upper biceps tendon is inflamed. It may result from misuse or general wear and tear. If you play sports, it can be as a result of the repeated movements you do on the court or field. It’s time for a vacation. Your illness could improve with rest and ice, but if it persists or worsens, you should visit your doctor for treatment to go back to your normal self.
FAQs
Non-Surgical Treatment
Relax: Avoiding painful activities is the first step toward healing.
Ice: To keep swelling down, apply cold packs many times a day for 20 minutes at a time.
NSAIDs, or nonsteroidal anti-inflammatory medicines, are…
Steroid injections
Physiotherapy.
It’s recommended to use the previously mentioned sleeping positions to fall asleep on your back or the side that isn’t impacted by bicep tendonitis. As part of your bedtime practice, you may also include mild shoulder stretches, but be careful not to overextend yourself.
It takes around six weeks for mild occurrences of tendinitis to recover on their own. It’s time to contact a specialist or orthopedic practitioner if this doesn’t happen. A doctor will ask you questions regarding the location, duration, and intensity of your pain during your session.
The purpose of Yergason’s test is to detect specific injuries to the biceps tendon, particularly those that impact the tendon’s long head, through a physical examination. It can also help in the diagnosis of biceps tendonitis, SLAP tears, and tears in the transverse humeral ligament.
Ice packs or cold packs might help lessen pain and swelling.
NSAIDs, or nonsteroidal anti-inflammatory medications. Aspirin and ibuprofen are two examples of medications that might reduce pain and edema.
Rest
Physical therapy
Steroid injections
Bicep tendonitis types
Distal bicep tendonitis is the term for inflammation seen close to the tendon that joins the biceps muscle to the elbow.
Proximal bicep tendinitis is the name for inflammation at the tendon’s origin where the biceps muscle and shoulder unite.






7 Comments