Type 2 Diabetes
Table of Contents
Introduction
Type 2 diabetes, also known as adult-onset diabetes or non-insulin-dependent diabetes, is a chronic metabolic disorder that affects how your body processes glucose (sugar). In this condition, your body becomes resistant to the effects of insulin or doesn’t produce enough insulin to maintain normal blood sugar levels.
Insulin is a hormone produced by the pancreas that helps regulate the amount of glucose in your bloodstream and allows it to enter your cells to be used as energy. When you have type 2 diabetes, your cells don’t respond properly to insulin, leading to elevated blood sugar levels.
Several factors contribute to the development of type 2 diabetes, including genetics, lifestyle choices, and obesity. Obesity and a sedentary lifestyle are significant risk factors for type 2 diabetes. However, not everyone who develops type 2 diabetes is overweight, as other factors such as genetics and age can also play a role.
What is diabetes?
Diabetes is a group of conditions where the body does not produce enough or any insulin, cannot properly utilize the insulin that is produced, or cannot do a combination of both.
When any of these things take place, the body is unable to transfer blood sugar to the cells. This could lead to increased blood sugar levels.
One of the primary energy sources is glucose, which is the type of sugar found in the blood. Because of insulin resistance or insufficiency, blood sugar levels increase. This might affect your health.
Here are the three primary forms of diabetes:
- Type 1 diabetes
- Type 2 diabetes
- Gestational diabetes
What’s the difference between Type 1 vs. Type 2 diabetes?
Type 2 diabetes is not identical to Type 1 diabetes. In Type 1 diabetes, the pancreas fails to produce any insulin. In type 2, the pancreas produces insufficient insulin, and the insulin that does get produced isn’t always effective. Both types are diabetes mellitus variants, which means that they cause hyperglycemia (high blood sugar).
Even though type 2 diabetes is more prevalent in kids, it primarily affects older persons. Type 1 diabetes usually arises in children or young adults, but people of any age can acquire it.
What is type 2 diabetes?
The inability of the body to adequately utilize food-derived energy is a symptom of type 2 diabetes. To aid cells in utilizing glucose (sugar), the pancreas produces the hormone insulin. However, a pancreas produces less insulin over time, and the cells begin to reject it. Too much sugar accumulates in the blood as a result of this. High blood sugar levels are associated with type 2 diabetes, which can result in heart disease, strokes, and even death.
It is a disease that happens when the blood glucose, also called blood sugar, is too high.
Type 2 diabetes results when there is a dysfunction in the body’s ability to control and utilize sugar as fuel. Another name for sugar is glucose. Blood glucose is the main source of energy and comes mainly from the food that we eat. The pancreas produces the hormone insulin, which facilitates the entry of glucose into the cells for utilization as fuel. In type 2 diabetes, the body either produces insufficient insulin or uses it poorly. The result is that too much glucose remains in the blood and not enough gets to the cells. This chronic ailment causes the blood to have an excessive amount of sugar running through it. Eventually, cardiovascular, neurological, and immune system issues might result from excessive blood sugar levels.
In general, type 2 diabetes has two problems:
- Insulin, which is a hormone that controls how quickly sugar enters cells, is not produced by the pancreas in sufficient amounts.
- Additionally, body cells absorb sugar less and have an insulin response also weak.
Despite the fact that both type 1 and type 2 diabetes can manifest in childhood and adulthood, respectively, type 2 diabetes used to be referred to as adult-onset diabetes. In older persons, type 2 diabetes is more prevalent. But as the number of fat youngsters rises, more young people are developing type 2 diabetes.
Middle age and older are the age groups most at risk for this form of diabetes. Earlier, it was referred to as “adult-onset diabetes.” Type 2 diabetes, however, also affects kids and teenagers as a result of childhood obesity.
Type 2 diabetes is the most common. Type 2 diabetes affects around 29 million Americans. Another 84 million people have prediabetes, which is increased blood sugar (or blood glucose), but not yet diabetes.
A chronic medical condition known as type 2 diabetes causes blood sugar levels, or glucose, to rise. This happens because the body cannot react to insulin effectively or is not able to produce enough of it.
Typically, the hormone insulin helps move glucose from the blood to the cells, where it’s used for energy. But with type 2 diabetes, the body’s cells aren’t able to respond to insulin as well as they should. Later stages of the illness could potentially result in inadequate insulin production by the body.
Uncontrolled type 2 diabetes can cause chronically high blood glucose levels, which can lead to a variety of symptoms as well as potentially fatal outcomes.
Type 2 diabetes does not have a treatment. Weight loss, a balanced diet, and exercise can all aid in the treatment of diseases. If diet and exercise are insufficient to control blood sugar, diabetes medications or insulin therapy may be suggested.
Causes of Type 2 Diabetes:
Two issues are the main causes of type 2 diabetes:
Hepatocytes, muscle cells, and fat cells all develop insulin resistance. The cells don’t absorb enough sugar as a result.
The amount of insulin the pancreas can produce is insufficient to maintain healthy blood sugar levels. Exactly why this happens is not known. Key contributing factors include being overweight and being inactive.
How does insulin work?
Insulin is a hormone that comes from the pancreas, a gland that is located behind and below the stomach. Insulin controls how the body utilizes sugar in the following ways:
The pancreas releases insulin in response to blood sugar levels. Sugar can enter the cells because insulin is circulating in the bloodstream.
Sugar levels in the bloodstream decrease.
In response to this reduction, the pancreas makes less insulin.
The function of glucose:
The primary energy source for the cells that make up muscles and other tissues is glucose, a sugar. Examples of how glucose is utilized and controlled include the following:
- Two of the primary sources of glucose are food and the liver.
- Once glucose has been absorbed into the bloodstream, insulin aids in its cellular uptake.
- The liver produces and stores glucose.
- In order to maintain the body’s glucose level within a healthy range when glucose levels are low, the liver converts glycogen that has been stored into glucose.
This method is ineffective in type 2 diabetes. Sugar accumulates in the blood instead of entering the cells. More insulin is released by the pancreas as blood sugar levels rise. Over time, the pancreas’ insulin-producing cells become damaged and are unable to create enough insulin to meet the body’s needs.
The pancreas makes a hormone called insulin. It helps the cells turn glucose, a type of sugar, from the food you eat into energy. People with type 2 diabetes make insulin, but their cells don’t utilize it as well as they should.
The pancreas initially produces more insulin in an effort to get glucose into the cells. But soon it can’t keep up, and the blood becomes thick with glucose.
Usually, a number of factors work together to develop type 2 diabetes. They could consist of:
- Genes: Various DNA fragments that influence how your body produces insulin have been discovered by scientists.
- Weight gain: Being overweight or obese, especially if you carry excess weight around the midsection, can lead to insulin resistance.
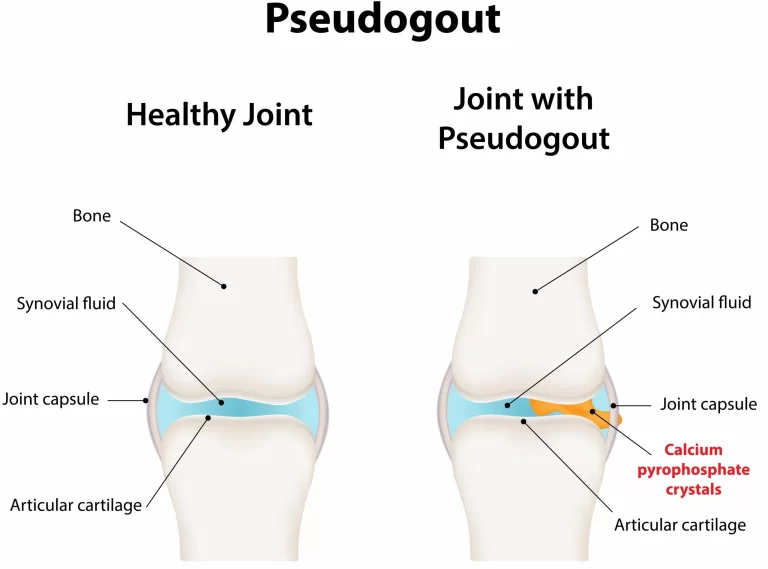
- Metabolic syndrome: People who have insulin resistance frequently also have a number of other health issues, such as high blood pressure, high cholesterol, and excessive triglycerides.
- When blood sugar is low, the liver produces and releases excessive amounts of glucose. After a person eats, the blood sugar goes up, and the liver will usually slow down and store its glucose for later. But some people’s livers don’t. They keep cranking out sugar.
- Ineffective cell communication: Cells occasionally send incorrect signals or fail to accurately receive messages. Diabetes can develop as a result of a series of issues that influence the production and utilization of insulin and glucose by your cells.
- Broken beta cells: When the insulin-producing cells release the incorrect quantity of insulin at the incorrect time, the blood sugar level is thrown off. These cells can also be harmed by high blood sugar levels.
Signs and Symptoms of Type 2 Diabetes:
Symptoms of type 2 diabetes often develop gradually. The symptoms of type 2 diabetes can be so mild that a person don’t notice them. Almost 8 million people who have it don’t know it. In fact, a person can live with type 2 diabetes for years and not know it. When symptoms are there, they may involve
- Increased thirst.
- Frequent urination.
- Increased hunger.
- Unintended weight loss.
- Fatigue.
- Blurred vision.
- Slow-healing sores.
- Frequent infections.
- Numbness or tingling in the extremities
- Areas of darkened skin, are usually present in the armpits and neck.
- Being cranky
- Tingling or numbness in the extremities
- Fatigue/feeling worn out
- Wounds that don’t heal
- Yeast infections that keep coming back
- Weight loss without trying
If a person has dark rashes around her neck or armpits, see the doctor. These are called acanthosis nigricans, and they can be signs that the body is becoming resistant to insulin.
Risk factors:
Factors that could raise the risk of type 2 diabetes include:
- Weight: Being obese or overweight carries a significant risk.
- Fat distribution: Storing fat largely in the abdomen as opposed to the hips and thighs indicates a higher risk. Type 2 diabetes is more likely to affect men and women whose waist measurements are over 40 inches (101.6 centimeters) and 35 inches (88.9 centimeters), respectively.
- Inactivity: The fewer active a person is, the greater the danger. Physical activity helps regulate weight, burns up glucose as energy, and makes cells more responsive to insulin.
- Family background: If a parent or sibling has type 2 diabetes, so does the individual.
- Race and ethnicity: Although it’s unclear why, people of certain races and ethnicities — including black, Hispanic, Native American, Asian, and Pacific Islanders — are more likely to develop type 2 diabetes than white people are.
- Blood lipid levels: Low levels of high-density lipoprotein (HDL) cholesterol, or the “good” cholesterol, and high levels of triglycerides are linked to an increased risk.
- Age: Age increases the incidence of type 2 diabetes, especially after age 35.
- Prediabetes: Blood sugar levels that are elevated but not high enough to be classified as diabetes as prediabetes.
- Pregnancy-related risks: The risk of developing type 2 diabetes is more in people who had gestational diabetes when they were pregnant and in those who gave birth to a baby weighing more than 9 pounds (4 kilograms).
- Polycystic ovary syndrome: Having polycystic ovary syndrome — a condition characterized by irregular menstrual periods, excess hair growth, and obesity — elevates the risk of diabetes.
Complications of High blood sugar levels
The following are possible side effects of type 2 diabetes and high blood sugar levels:
- Digestive problems, including gastroparesis.
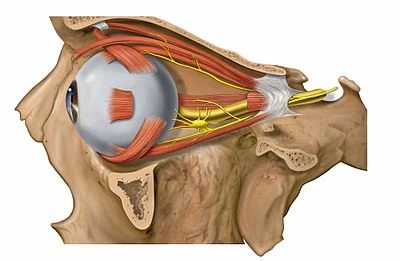
- Eye problems, including diabetes-related retinopathy.
- foot problems, including leg and foot ulcers.
- Gum disease and other mouth problems.
- Hearing loss.
- Heart disease.
- Kidney disease.
- liver problems, including nonalcoholic fatty liver disease.
- peripheral neuropathy (nerve damage).
- Sexual dysfunction.
- Skin conditions.
- Stroke.
- Urinary tract infections and bladder infections.
Diabetes-related ketoacidosis (DKA) is a disease that only very rarely results from type 2 diabetes. The disease DKA, which can be fatal, makes the blood acidic. Type 1 diabetics are more likely to experience DKA.
Diagnosis:
A1C test: Type 2 diabetes is usually diagnosed with the glycated hemoglobin (A1C) test. This blood test shows the average blood sugar level for the last two to three months. The results are interpreted as follows:
- Below 5.7% is normal.
- 5.7% to 6.4% of the population is diagnosed with prediabetes.
- Diabetes is diagnosed when two tests show a 6.5% or higher level.
If the A1C test is not available, or if a person has certain conditions that interfere with an A1C test, the health care provider may use the following tests to diagnose diabetes:
Random blood sugar test: Random blood sugar test: The measurement of blood sugar is expressed in millimoles of sugar per liter (mmol/L) or milligrams of sugar per deciliter (mg/dL) No matter when a person last ate, a level of 200 mg/dL (11.1 mmol/L) or higher suggests diabetes, especially if the individual also exhibits signs of diabetes like severe thirst and frequent urination.
Fasting blood sugar test: For a fasting blood sugar test, a blood sample is obtained when you haven’t eaten anything all day. A fasting blood sugar test is another name for this. On an empty stomach, it monitors blood sugar levels. For eight hours before to the test, nothing but water may be consumed by the subject. The findings are explained as follows:
- The normal value is Less than 100 mg/dL (5.6 mmol/L). A blood sugar level of 100 to 125 mg/dL (5.6 to 6.9 mmol/L) is referred to as prediabetes.
- When two independent tests reveal 126 mg/dL (7 mmol/L) or higher, diabetes is suspected.
Oral glucose tolerance test: Used less frequently than the others, with the exception of during pregnancy.A patient will be required to go without food for a predetermined period of time before drinking a sweet beverage at their doctor’s office. This checks the blood glucose before and 2 hours after a person drinks something sweet to see how the body handles the sugar. After that, every two hours, blood sugar levels are tested. The results are interpreted as follows:
- After two hours, a level of less than 140 mg/dL (7.8 mmol/L) is regarded as healthy.
- Blood sugar values between 140 and 199 mg/dL (7.8 and 11.0 mmol/L) are considered prediabetic.
- A reading of 200 mg/dL (11.1 mmol/L) or above after two hours signified diabetes.
Screening test
The American Diabetes Association advises routine type 2 diabetes screening using diagnostic testing in all persons age 35 and older and in the following populations:
- Individuals under the age of 35 who are overweight or obese and have one or more diabetes risk factors.
- Pregnant women with gestational diabetes.
- Individuals with prediabetes who have received a diagnosis.
- Children who are overweight or obese, have a family history of type 2 diabetes, or who otherwise pose a risk.
Treatment of Type 2 Diabetes:
Management of type 2 diabetes contains:
- Healthy eating
- Regular exercise
- Weight loss
- Possibly, diabetes medication or insulin therapy
- Blood sugar monitoring
All of these actions increase the likelihood that blood sugar will remain at a healthy level. And they could aid in delaying or avoiding difficulties.
Healthy eating:
There’s no specific diabetes diet. However, it’s essential to focus on diet:
- A routine for healthy snacks and dinners.
- Reduced serving sizes.
- More whole grains, nonstarchy veggies, and fruits that are high in fiber.
- Less sugar, starchy veggies, and refined carbohydrates.
- Reasonable portions of low-fat dairy, meat, and seafood.
- Oils that are good for cooking, such canola or olive.
- Fewer calories.
A healthcare provider may suggest seeing a registered dietitian, who can help :
-Identify healthy food choices.
-Plan well-balanced, nutritional meals.
-Develop new habits and address barriers to changing them.
-To maintain more stable blood sugar levels, keep a trace of carbohydrate intake.
Physical Exercise in Type 2 Diabetes
Exercise is crucial for keeping a healthy weight or decreasing weight. It also helps manage blood sugar. Talk to the health care provider before beginning or changing the exercise program to ensure that activities are safe for you.
Aerobic exercise: Pick an aerobic activity you enjoy doing, like biking, running, swimming, or walking. Adults should strive for 150 minutes or more of weekly moderate aerobic exercise, or 30 minutes or more, on most days.
Resistance workout: Your strength, balance, and capacity to carry out daily tasks more readily all grow with resistance training. Resistance training includes weightlifting, yoga, and calisthenics. Type 2 diabetic adults should aim to complete two to three bouts of resistance training per week.
Try to stay active: To help control blood sugar levels, long periods of inactivity, such as working at a computer, might be broken up. Every 30 minutes, spend a few minutes standing up, moving around, or engaging in mild exercise.
Weight loss
Weight loss results in better maintenance of blood sugar levels, cholesterol, triglycerides, and blood pressure. When someone loses even 5% of their body weight, these things may start to improve for them if they are overweight. However, the health benefits increase as a person loses more weight. Up to 15% of the body weight may be lost in rare circumstances.
You can set realistic weight-loss goals with assistance from a healthcare professional or dietician, who will also urge you to make necessary lifestyle adjustments.
Monitoring the Blood sugar
To ensure that their blood sugar levels stay within their goal range, a person will receive advice from a healthcare professional on how frequently to monitor their blood sugar levels. One daily check is required, as well as checks before and after any exercise. When taking insulin, a person may need to check their blood sugar several times per day.
A blood glucose meter, a compact home appliance that measures the quantity of sugar in a drop of blood, is typically used for monitoring. To share with your medical staff, keep a record of your measurements.
A sensor inserted under the skin is used by a continuous glucose monitoring device to record glucose levels every few minutes. The system can provide alarms when levels are too high or low and information can be relayed to a mobile device like a phone.
Diabetes medications:
A healthcare professional may recommend insulin therapy or prescription diabetic drugs that lower glucose levels if a patient is unable to maintain the target blood sugar level with diet and exercise. The following are some type 2 diabetic medications.
Metformin (Fortamet, Glumetza, and other brands) is frequently the first course of treatment for type 2 diabetes. It primarily works by reducing the amount of glucose produced by the liver and increasing the body’s sensitivity to insulin, allowing it to use the hormone more efficiently.
Some people need to take supplements if they have a B-12 deficit and feel symptoms. Additional negative effects that might get better with time include:
- Nausea.
- Abdominal pain.
- Bloating.
- Diarrhea
Sulfonylureas help the body secrete more insulin. Examples include glimepiride (Amaryl), glipizide (Glucotrol XL), and glyburide (DiaBeta, Glynase).
Possible side effects involve:
- Low blood sugar.
- Weight gain.
Glinides stimulate the pancreas to secrete more insulin. They’re faster-acting than sulfonylureas. But the duration of their bodily effects is less. Examples include repaglinide and nateglinide. Possible side effects involve:
- Low blood sugar.
- Weight gain.
Thiazolidinediones: The body’s tissues become more responsive to insulin when given thiazolidinediones. The medication pioglitazone (Actos) is an illustration of this. Possible side effects involve:
- Risk of congestive heart failure.
- Risk of bladder cancer (pioglitazone).
- Risk of bone fractures.
- Weight gain.
DPP-4 inhibitors reduce blood sugar levels, but they often have very little of an effect. Sitagliptin (Januvia), saxagliptin (Onglyza), and linagliptin (Tradjenta) are a few examples. Possible side effects involve:
- Risk of pancreatitis.
- Joint pain.
GLP-1 receptor agonists: By delaying digestion, injectable medications called GLP-1 receptor agonists help lower blood sugar levels. Some of them may reduce the risk of heart attack and stroke, and they are usually used in conjunction with weight loss. Examples include semaglutide (Rybelsus, Ozempic, and Wegovy), liraglutide (Saxenda, Victoza), and exenatide (Byetta, Bydureon Bcise). Possible side effects involve:
- Risk of pancreatitis.
- Nausea.
- Vomiting.
- Diarrhea.
SGLT2 inhibitors interfere with the kidney’s ability to clean the blood by preventing glucose from being released back into the bloodstream. As a result, urine contains no glucose. These drugs may reduce the risk of heart attack and stroke in people who have a high risk of contracting specific conditions. Possible side effects involve:
- Vaginal yeast infections
- Urinary tract infections
- Low blood pressure.
- High cholesterol.
- Risk of gangrene.
- Risk of bone fractures (canagliflozin).
- Risk of amputation (canagliflozin).
In addition to diabetic meds, a doctor may also recommend blood pressure and cholesterol-lowering drugs, as well as low-dose aspirin to help prevent heart and blood vessel damage.
Insulin Therapy:
Certain type 2 diabetics require insulin therapy. Today, insulin therapy may be recommended earlier if blood sugar targets are not achieved by lifestyle changes and other treatments, as opposed to the past when it was only used as a last choice.
The time it takes to start working and how long it takes to have an effect vary between different forms of insulin.For instance, long-acting insulin is designed to work continuously during the day or overnight to keep blood sugar levels stable. At mealtimes, short-acting insulin is typically administered.
Your doctor will decide which type of insulin is best for you and when to administer it. The kind of insulin you take, how much you take, and when you take it may change depending on how stable your blood sugar levels are. Injections are used to give the majority of insulin types.
The dangers of low blood sugar, or hypoglycemia, diabetic ketoacidosis, and excessive triglycerides are among the side effects of insulin.
Weight-loss surgery
The digestive system’s structure and functionality are altered by weight-loss surgery. You could manage type 2 diabetes, your weight, and other obesity-related diseases with the help of this operation. There are numerous surgical techniques. Limiting the amount of food people can eat, they all assist people in losing weight. Additionally, some operations restrict how much nutrition the body may absorb.
A thorough therapeutic approach may include multiple components, including weight loss surgery. Guidelines for food and nutritional supplements, exercise, and mental health care are also included in the treatment.
In general, persons with type 2 diabetes with a body mass index (BMI) of 35 or higher may be candidates for weight-loss surgery. Weight and height are inputs into the BMI formula, which estimates body fat. Surgery may be an option for someone with a BMI under 35, depending on the degree of diabetes or the existence of other medical issues.
Using weight and height, the BMI formula calculates an estimate of body fat. Surgery may be an option for someone with a BMI under 35, depending on the degree of diabetes or the existence of other medical issues.
Surgery for weight loss necessitates a lifetime commitment to behavioral adjustments. Osteoporosis and dietary deficits are potential long-term negative effects.
Pregnancy
Pregnant women with type 2 diabetes frequently need to modify their treatment regimen and adhere to a low-carb diet. Several women require insulin medication when pregnant. They might also have to stop taking other medications, such as blood pressure ones.
A disorder called diabetic retinopathy, which affects the eyes, is more likely to occur during pregnancy. This problem could occasionally worsen while a woman is pregnant. Every trimester of your pregnancy and for a year after giving birth, if you’re pregnant, you should see an ophthalmologist. Alternatively, as often as your doctor advises.
Diet for type 2 diabetes
Diet plays a crucial role in preserving optimum heart health and blood sugar levels that are within safe limits.
Nearly everyone should adhere to the diet recommended for those with type 2 diabetes. It all comes down to these crucial actions:
- Various foods that are rich in nutrients and low in empty calories should be chosen.
- Practice controlling your portion sizes and quitting when you’re full.
- Read food labels carefully to see how much sugar or carbohydrates a serving size could contain.
- Foods and beverages to limit
If a person has been diagnosed with type 2 diabetes, or even if they are trying to avoid diabetes and manage their weight, there are certain foods and beverages that a person should limit if possible. These include:
- Red meat and full-fat dairy products are examples of foods high in saturated or trans fats.
- Processed meats (including hotdogs and salami)
- Margarine and shortening
- Refined baked goods (such as white bread and cake)
- Snacks with a lot of sugar and processing (packaged cookies and some cereals)
- Sugary drinks (includes regular soda and some fruit juices)
- While no one food, enjoyed every so often, should knock you off the healthy path, it’s a good idea to talk with the doctor about dietary restrictions based on blood sugar levels. After consuming these items, some people may need to check their blood sugar levels more carefully than others.
Foods to select
If you have type 2 diabetes, carbs are not necessarily off-limits. You can get energy and fiber from healthy carbohydrates. Several possibilities are:
- Whole fruits
- Non-starchy vegetables (like broccoli, carrots, and cauliflower)
- Legumes, like beans
- Whole grains, like oats or quinoa
- Sweet potatoes
Fat is not off the table, either. Instead, it comes down to picking the proper kinds of fat. The following foods contain heart-protective omega-3 fatty acids:
- Tuna
- Sardines
- Salmon
- Mackerel
- Halibut
- Cod
- Flax seeds
Healthy monounsaturated and polyunsaturated fats can be found in a variety of foods, including:
- Oils, like olive oil
- Nuts, like almonds, pecans, and walnuts
- Avocados
Talk with the doctor about personal nutrition goals. They might advise you to get in touch with a dietitian who is knowledgeable about the best meals for diabetics. Together, you can create a diet strategy that tastes wonderful and fits your lifestyle requirements.
FAQs:
Can type 2 diabetes be treated completely?
Type 2 diabetes does not have a treatment. Weight loss, a balanced diet, and exercise can all aid in the treatment of diseases. If diet and exercise are insufficient to control blood sugar, diabetes medications or insulin therapy may be suggested.
Does type 2 diabetes last for life?
People with diabetes can live longer by meeting their treatment goals. Under extreme circumstances, the lifespan may be increased by three years or even up to ten years. In type 2 diabetics, the life expectancy, or the number of years one should plan to live, is 6 years lower than in non-diabetics at age 50.
Does type 2 diabetes require insulin?
People with type 2 diabetes don’t necessarily need to take insulin immediately away; type 1 diabetics typically do. The likelihood that someone with type 2 diabetes may need insulin increases with time. Insulin is a tool for controlling blood glucose levels, just as it is in type 1 diabetes.
At what sugar level is insulin required?
If the initial fasting plasma glucose is greater than 250 or the HbA1c is greater than 10%, insulin therapy will frequently need to be begun.
Is insulin safe for kidneys?
Insulin has minimal to no impact on renal hemodynamics, glomerular filtration rate, or albumin permeability in healthy people.In patients with non-insulin-dependent diabetes, hyperinsulinemia increases the excretion of albumin in the urine only in some cases.




21 Comments