Tennis leg: Cause, Symptoms, Diagnosis, Treatment:
Table of Contents
Introduction
Tennis Leg refers to an acute medial head of the gastrocnemius muscle tear in the older athlete characterized by sudden onset of very severe calf pain and significant disability. The injury is invariably associated with extensive bruising & swelling, & can be mistaken for a deep venous thrombosis. The more common site is the medial head of gastrocnemius, but occasionally the plantaris muscle is involved. Symptoms are a sudden, sharp, or burning pain in the leg, many times accompanied by an audible sound. In more cases, the player is unable to resume play because of the severe pain. Depending on the severity of the injury, recovery may take between a few days & 6 weeks.
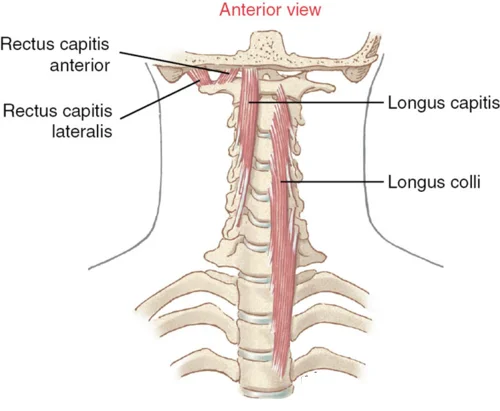
Anatomy
Gastrocnemius muscle
gastrocnemius – in conjunction with soleus muscle, provides primarily plantar flexion of the knee joint and flexion at the ginglymoid joint. plantar flexion provides the knee joint force throughout gait. though it spans over two joints, the gastrocnemius muscle isn’t able to exert its most power on each joint at the same time. If the knee is flexed, the gastrocnemius muscle cannot produce most power at the ankle joint and the other way around.
Origin: proximal to body part surfaces of aspect condyle of the leg bone and medial condyle of the femur
Insertion: tendo calcaneus (Achilles tendon) into mid-posterior or tarsi fibular
Nerve: tibial nerve from the sciatic, nerve roots S1 – S2
Actions: plantar flexes foot, flexes knee
Antagonist: Tibialis anterior muscle
Soleus muscle
soleus – is found at a lower place the gastrocnemius within the superficial posterior compartment of the lower leg. It is main performance is area flexion of the ankle joint and helps the shinbone on the calcaneus limiting forward sway.
Origin: Fibula, medial border of tibia (soleal line)
Insertion: Tendo or tarsi fibular
Nerve: Tibial nerve, nerve roots L5 – S2
Actions: Plantar flexion
Antagonist:Tibialis anterior
Plantaris muscle
plantaris – is located within the posterosuperficial compartment of the calf. Functionally, plantaris isn’t a serious contributor and acts with gastrocnemius muscle as each a flexor muscle of the knee and a plantar flexor of the ankle joint.
Origin: Lateral supracondylar ridge of the femur on top of the lateral head of gastrocnemius muscle
Insertion: Tendo calcaneus (medial aspect, deep to gastrocnemius muscle connective tissue
Nerve: tibial nerve from anterior rami of S1-S2
Actions: Plantar flexes the foot and flexes the knee
Antagonist: Tibialis anterior muscle
Causes of Tennis leg
Age/activity status: Medial calf injuries happen most commonly in middle-aged recreational athletes. This population typically resumes being physically active at an average to high intensity but not on a regular basis, and these individuals are also likely to have maintained an average degree of muscle mass from their more active days.
Deconditioned/un-stretched muscles: The cold and un-stretched muscles that recreational athletes often use to take the part are very likely to rupture when challenged compared with conditioned & stretched muscles.
Previous injury: The athlete with recurrent calf strains is likely to have healed with fibrotic scar tissue, which absorbs forces differently and is thus most likely to result in rupture when the muscle is challenged.
Risk Factors for tennis leg
This injury happens commonly in sports activities (e.g, hill running, jumping, tennis), but it can occur in any activity. A medial calf injury is often seen in the irregular active athlete. Medial calf injuries occur most commonly in men than in women,& these injuries usually afflict athletes and others in the 4th to 6th decade of life. Medial calf injuries are more commonly seen acutely, but up to 20% of affected patients report a prodrome of calf tightness several days before the injury, thus suggesting a potential chronic predisposition.
Sports Biomechanics for Tennis Leg
This condition has been termed “tennis leg” because of its prevalence in this particular sport, but medial calf injury can occur in a variety of sports or other activities. One mechanism that happens is on the back leg during a lunging shot, in which the knee is extended while the foot is dorsiflexed. This activity puts maximal tension on the gastrocnemius muscle as the lengthened muscle is contracted at the “push off,” resulting in a tennis leg injury. This is the normal position of the back leg in a tennis stroke, and it results in the greatest force on the muscle unit; but tennis leg injury can also happen during a typical contraction of ankle plantar flexion, especially if the athlete is pushing or lifting a large weight or force.
Signs and symptoms of tennis leg
- An audible pop when the injury to the medial calf occurred is commonly reported.
- The patient complains of calf pain, which additionally radiates to the knee or the ankle. Also, the patient complains of pain with ankle movements.
- The patient complains of a swollen leg that extends down to the foot or ankle, & also the associated color changes of bruising.
- Tenderness is prominent upon palpation in the all medial gastrocnemius muscle, but this tenderness is observed to be exquisitely most painful at the medial musculotendinous junction.
- Palpation of the Achilles tendon might demonstrate an intact tendon.
- The peripheral pulses might be present and symmetric.
- Moderate to severe pain is denoted by passive ankle dorsiflexion (due to stretching of the torn muscle fibers) in the tennis leg, also with active resistance to ankle plantar flexion (due to the firing of the torn muscle fibers).
Diagnosis of tennis leg
Diagnosis of tennis leg needs a diagnostic ultrasound scan as well as a clinical assessment.
A clinical assessment at Complete will include:
1. Clinical interview
To help formulate a hypothesis about tennis leg the clinician will ask a series of questions to understand how and why your pain begins. A medical history will also be taken to rule out another source of your pain including deep vein thrombosis (DVT). Differentially diagnosing a DVT is of critical importance as DVT needs urgent medical assistance, involving anticoagulant medication.
2. Physical assessment
Physical assessment is used to locate the cause of symptoms and why they may have occurred. It includes:
Close observation of the calf muscle for improving heat, swelling, bruising, or calf muscle shape change (indicative of rupture)
Ankle & calf range of movement
Calf strength testing – can you stand on 1 leg or perform a heel raise?
Gentle palpation of the calf complex
Walking assessment.
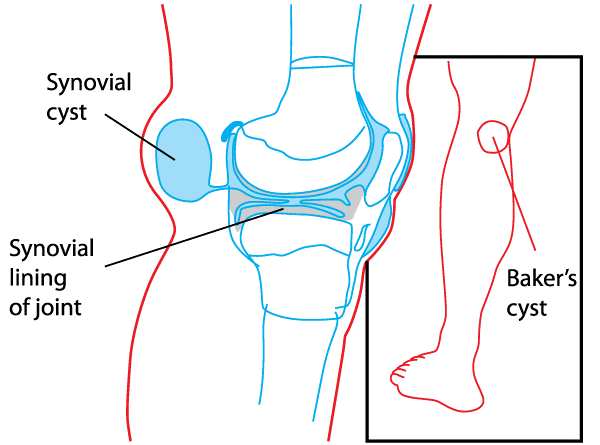
3. Diagnostic musculoskeletal ultrasound scan
Diagnostic musculoskeletal ultrasound imaging is the main imaging modality for a calf muscle tear. It visualizes the injury better than an MRI scan & also provides information related to whether or not there is a large hematoma (fluid collection – see image below) in the calf (a common occurrence in this injury). On 1st appointment at Complete, we will carry out a scan (no extra charge) & will determine whether the fluid might be aspirated (drained) to help with pain levels & the healing of the tear.
Bright et al (2018) describe diagnostic ultrasound as capable of assessing the presence of calf injury, estimating the degree of severity & aid in its management by routinely monitoring the healing process throughout rehabilitation.
Differential diagnosis of tennis leg
- Ankle Osteoarthritis (OA)
- Chronic ankle sprain
- Morton’s neuroma
- Plantar Fasciitis
- Sinus Tarsi Syndrome
- Midfoot Osteoarthritis (OA)
- Gout
- Retrocalcaneal and pre-Achilles bursitis
- Mid-potion Achilles tendinopathy
- Baxter’s nerve
Medical Treatment of tennis leg
Pain management might include analgesics as indicated. Caution might be used with nonsteroidal anti-inflammatory drugs (NSAIDs) during the acute injury phase, as these agents can predispose the patient to increased bleeding and hematoma formation in the starting days after an injury. Theoretically, cyclooxygenase-2 (COX-2) inhibitors may provide pain control without the risk of bleeding in acute injuries, which is a covered with traditional NSAIDs.
Ankle/foot bracing might be used to keep the ankle in a position of maximal tolerable dorsiflexion. Studies have shown an improved rate of healing with this intervention.
Physiotherapy Treatment of tennis leg
Acute Stage Rehabilitation The following action might be taken as fast as possible, certainly within 48 hours.
RICE Principle:
Rest: Don’t push through pain, which can make the problem worse. Avoid walking or running with calf muscle pain.
Ice: Put an ice pack or cold compress on the calf muscles for 20 minutes every two hours. & don’t apply ice directly to the skin.
Compression: Apply a compression wrap & bandage to the calf. compression helps to minimize the swelling & reduce blood flow to the painful area.
Elevation: Lift your leg into an elevated position, preferably above the level of your heart. Support the entire length of your leg with pillows, blankets, or cushions. If sore calves from a muscle cramp or feel a painful knot in the calf muscle, it may help to gently calf.
Once the worst pain and swelling have subsided (after 1 to 2 days), start to build up the training load. During this period, pain is a signal to rest. Do not cross the pain threshold, as this will slow down the healing process. The training load is built up in three steps. These are described below, with several tips:
Step 1. Improvement of General Condition
If the pain permits, you may put weight on the foot, if necessary using elbow crutches during the 1st week. The foot should be used in a normal fashion.
A heel lift (with shock absorption) in both shoes for 1 to 2 weeks may help to ease the load on the calf muscles during walking. ‘Viscoheels’ are very useful for these causes.
Stretching the long calf muscles: Step forward with the unaffected leg, and remain with the heel of the back leg on the floor. The knee of the affected leg remains straight. Shift the weight of the back leg to the front leg and press the heel of the back leg softly into the floor. Rest with hands on a stationary object. The stretch is perceived high up in the calf. Hold the stretch for 15 to 20 seconds without bouncing, followed by a rest period of 10 to 20 seconds & Repeat 3 times.
Stretching the short calf muscles. begin from the same position as described above, but now bend the knee of the hind leg, while keeping the heel on the floor. The stretch is perceived as low in the calf. Again, grasp the stretch for 15 to 20 seconds (no bouncing), followed by 10 to 20 seconds of rest,& repeat 3 times.
Strengthening the foot muscles. Sit on a chair. Write the alphabet in the air with the foot of the injured leg. double up a towel by grasping it with the toes of the injured leg. Perform this for 15 to 20 seconds, followed by 10 to 20 seconds of rest, & repeat 10 to 20 times.
Swimming or cycling for 30 minutes every day improves the blood flow to the calf muscles and improves the recovery after a tennis leg injury.
Step 2. Build-up
As soon as each of the exercises can be done and walking is possible without pain, a return to tennis and other sports can be considered.
Start by strengthening the calf muscles. leisurely rise onto your toes and hold this position for 10 to 20 seconds. Then return to the starting position. do this exercise with both feet at the same time, then when leaning on the injured leg only. If working body weight is too painful or difficult, elastic tubing may be used to work the plantar flexors (i.e. press the toes and forefoot down against the resistance of the elastic tubing). Take small, fast steps on the spot, alternating the left and the right leg.
If this moves well, you can begin jogging. Start with an easy jog, then include some sprints and straight running, followed by fast turns, starts, and stops.
Finally, you can include jumping exercises.
Step 3. Return to Play
A return to the tennis court might now be possible. Start against the practice wall or with mini tennis & slowly increase the distance to the wall or your opponent on the court. Make sure to position yourself well for the ball by taking small steps.
In this phase, you can also add volley exercises.
slowly (over the course of 1 to 2 weeks) include more exercises that involve moving longer distances toward the ball. Next, add low volleys, followed by overheads and services.
As soon as you can hit a smash with footwork without problems, you are ready to start playing points, games & or a practice match.
Once you have played practice matches for 2 weeks in succession without problems, you can start playing matches again.
How to prevent tennis leg?
Reduce the risk for tennis leg by following points:
Prepare: The best way to prevent tennis leg and muscle strains is to sufficiently warm-up prior to the playing. I know no one likes to give the time to warm-up, but it is critical for injury prevention. Get to the court early to perform dynamic warm-up. A 5-7 minutes dynamic warm-up is perfect within 15 minutes of match time. This includes movements to help lengthen muscles to prepare for tennis and increases your heart rate and body temperature so body is warm, which may help decrease risk for injury. Once you compete dynamic warm-up, grab racket and start hitting.
Recover: Immediately following match, stay on the court to stretch arms and legs. They just did a lot of work so help the muscle cool down so aren’t stiff or sore the next day. Stretching helps maintain flexibility and joint mobility. Hold each stretch for about 30 seconds. A few of stretches are best done on the floor, so it is ideal to throw a yoga mat down and finish stretching in the club house or locker room. Cool-down stretching might be done within 30 minutes of coming off the court, so do this prior to shower & change clothes.
Roll it out: Foam rolling is a great way to stretch and massage muscles and fascia after you play.The combining this with stretching. Roll all muscle for about 30 seconds.
Repair: At the last of day, take a warm bath with 1-2 cups of Epsom salts for about 15 minutes. The magnesium sulfate in the Epsom salts is soothing for sore, tight and tired muscles & diminishes pain & muscle tension promoting more restful sleep. So, take bath prior to bedtime.
Protect: If you have expertise a calf muscle strain or Tennis leg, consider applying a compression sleeve around the lower leg. During the cool weather months, adapt clothing to the weather conditions. It may be benefit to wear pants, running tights, or compression gear to keep legs warm. Well-warmed muscles are better able to withstand pulling & traction forces than cold muscles.
Massage: Every some weeks, consider investing in a deep tissue or sports massage to help increase circulation & repair tired, sore, tight muscles. Massage helps to on-court performance, so make time for it.
Cross train: Cycling, running, Pilates & yoga as great ways to cross train for tennis, which build strength & flexibility and will help reduce risk of muscle trains & tears.





4 Comments