Syndesmotic Ankle Sprain
Table of Contents
What is a Syndesmotic Ankle Sprain?
A Syndesmotic Ankle Sprain, also known as a high ankle sprain, is an injury that affects the syndesmosis, which is a group of ligaments that connect the two lower leg bones, the tibia (shinbone), and the fibula (the thinner bone on the outer side of the lower leg). This type of ankle sprain is different from the more common lateral ankle joint sprain, which affects the ligaments on the outer side of the ankle joint.
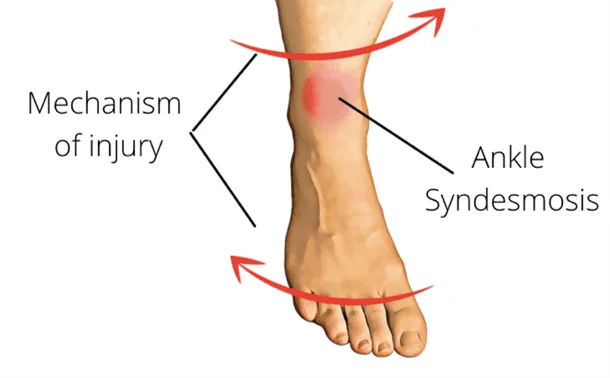
In a syndesmotic ankle sprain, the ligaments of the syndesmosis are stretched, torn, or injured due to excessive force, often caused by twisting or rotational movements of the ankle. This can result in pain, swelling, bruising, and difficulty with weight-bearing and walking. Syndesmotic ankle sprains are typically graded based on their severity, with mild sprains involving minor ligament damage and severe sprains involving significant ligament tears or fractures.
Anatomy
The anatomy of the ankle is intricate and involves several bones, ligaments, tendons, and muscles. Understanding the key anatomical components is important in recognizing the structures affected in a syndesmotic ankle sprain (high ankle sprain). Here’s an overview of the ankle anatomy:
- Tibia: The tibia, also known as the shinbone, is the larger of the two lower leg bones and forms the inner part of the ankle joint.
- Fibula: The fibula is the thinner bone of the lower leg and runs parallel to the tibia, forming the outer part of the ankle joint.
- Talus: The talus is a bone that sits atop the calcaneus (heel bone) and forms the lower part of the ankle joint. talus connects the leg bones (tibia and fibula) to the foot bones.
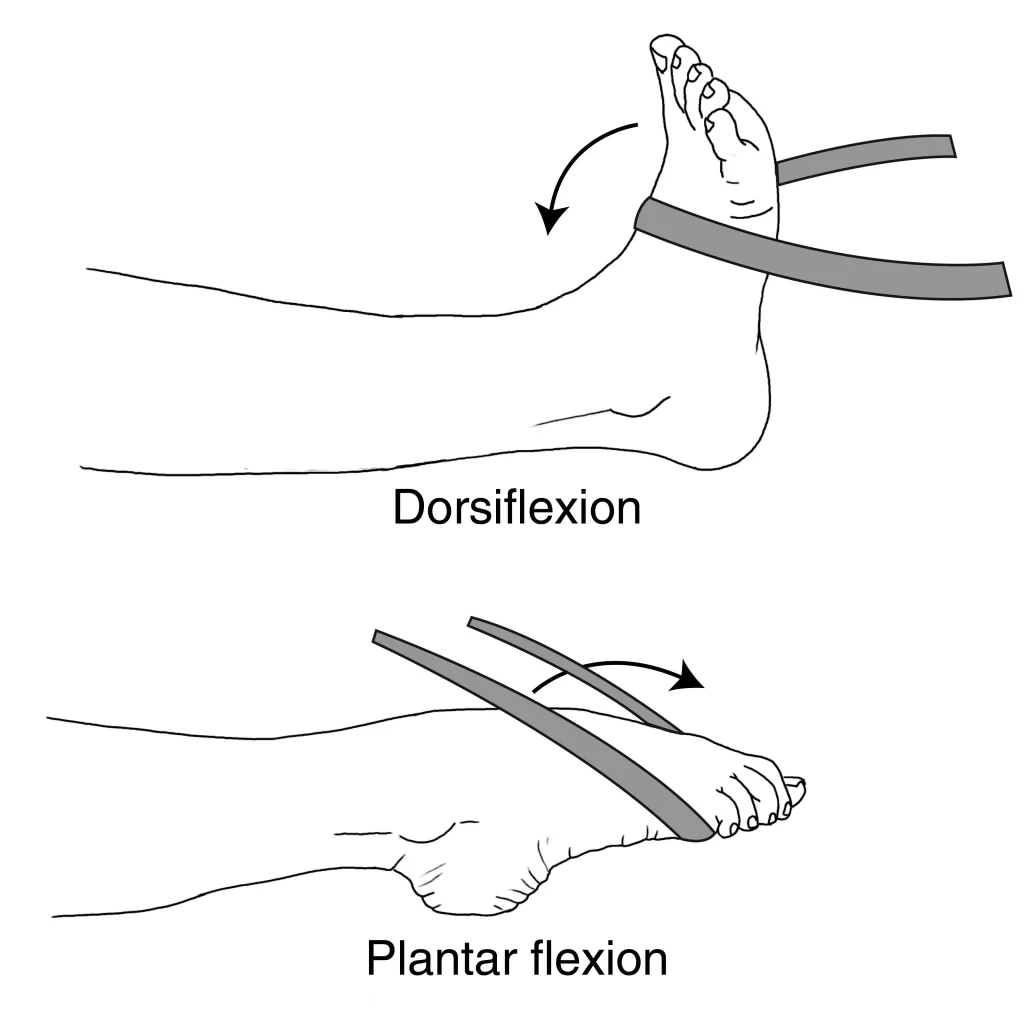
- Ankle Joint: The ankle joint, or talocrural joint, is a hinge joint formed by the tibia, fibula, and talus. The ankle joint allows for dorsiflexion (lifting the foot) and plantarflexion (pointing the foot downward).
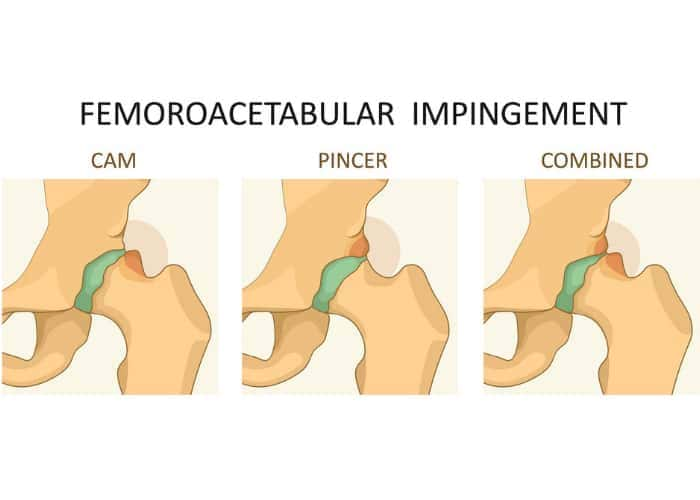
- Syndesmosis: The syndesmosis is a group of strong ligaments that connect the tibia and fibula bones at their upper ends, just above the ankle joint. These ligaments include the anterior tibiofibular ligament, posterior tibiofibular ligament, and interosseous ligament.
- Lateral Ligaments: On the outer side of the ankle, there are three primary lateral ligaments: the anterior talofibular ligament (ATFL), calcaneofibular ligament (CFL), and posterior talofibular ligament (PTFL). These ligaments stabilize the ankle against excessive inversion (inward rolling) of the foot.
- Medial Ligaments: On the inner side of the ankle, the primary medial ligament is the deltoid ligament. It provides stability and resists excessive eversion (outward rolling) of the foot.
- Achilles Tendon: The Achilles tendon is the largest and strongest tendon in the ankle area. The Achilles tendon connects the calf muscles (gastrocnemius and soleus) to the heel bone (calcaneus) and is crucial for plantar flexion.
- Peroneal Tendons: These tendons run along the outer part of the ankle and are responsible for ankle stability and eversion of the foot.
- Muscles: Numerous muscles in the lower leg and foot play a role in ankle movement and stability. The major ones include the gastrocnemius, soleus, tibialis anterior, peroneus longus, and peroneus brevis.
Causes of Syndesmotic Ankle Sprain
Syndesmotic ankle sprains are often caused by a combination of factors, including:
- Twisting or rotating the ankle: Sudden and forceful twisting or rotating motions of the ankle can cause the syndesmotic ligaments to stretch or tear.
- Impact or trauma: A direct impact to the ankle, such as during a car accident or sports collision, can also lead to this type of sprain.
- Landing from a height: Athletes who jump and land forcefully, like basketball or volleyball players, are at increased risk due to the impact when landing.
- Uneven terrain: Walking, running, or playing on uneven surfaces can increase the risk of twisting the ankle and causing a syndesmotic sprain.
- Overpronation: Individuals with excessive inward rolling of the foot (overpronation) may be more prone to syndesmotic sprains.
- High-impact sports: Activities that involve sudden changes in direction, such as football, soccer, and skiing, can increase the likelihood of this type of ankle injury
- Plantarflexion and external rotation: This specific ankle position, where the foot is pointed downward and rotated outward, can increase the risk of syndesmotic injuries, especially during athletic activities.
- Previous ankle injuries: Individuals who have had prior ankle injuries, including syndesmotic sprains, may be more susceptible to re-injury due to weakened ligaments and altered biomechanics.
- Inadequate footwear: Wearing improper or ill-fitting footwear during sports or activities can decrease ankle stability and increase the risk of sprains, including syndesmotic ones.
- Fatigue or muscle weakness: Weak ankle or calf muscles, as well as overall fatigue, can lead to poor joint stability and a higher likelihood of sustaining an ankle sprain.
- Poor conditioning and flexibility: A lack of proper conditioning and flexibility can impair an individual’s ability to control ankle movements, making them more vulnerable to sprains.
- Age and gender: Younger individuals and males tend to be more prone to syndesmotic ankle sprains, possibly due to their participation in high-risk activities and differences in biomechanics.
- Obesity: Excess body weight can increase the force exerted on the ankle joint during activities, making it more susceptible to injury.
Risk Factor
Several risk factors can increase the likelihood of experiencing a syndesmotic ankle sprain. These risk factors include:
- Participation in High-Impact Sports: Engaging in sports that involve rapid changes in direction, jumping, or contact, such as football, basketball, soccer, and skiing, can elevate the risk of syndesmotic sprains.
- Previous Ankle Injuries: Individuals with a history of ankle sprains or instability may be more prone to syndesmotic injuries, as previous damage to ligaments can weaken ankle stability.
- Foot Biomechanics: Factors like overpronation (excessive inward rolling of the foot), high arches, or flat feet can alter ankle joint mechanics and increase the risk of sprains, including syndesmotic ones.
- Inadequate Footwear: Wearing shoes that lack proper support or do not fit well can reduce ankle stability and make sprains more likely.
- Muscle Weakness and Imbalance: Weak ankle or calf muscles, as well as imbalances in strength between different muscle groups, can hinder joint stability.
- Fatigue: Performing physical activities when fatigued can compromise coordination and increase the risk of injury.
- Age and Gender: Younger individuals and males are generally at a higher risk of syndesmotic ankle sprains, possibly due to their participation in high-risk activities and differences in physical development.
- Obesity: Excess body weight can place additional stress on the ankle joint, making it more susceptible to injury.
- Environmental Factors: Walking, running, or playing on uneven or slippery surfaces increases the risk of twisting the ankle and causing a sprain.
- Lack of Proper Warm-Up and Stretching: Failing to warm up adequately and perform stretching exercises before physical activity can reduce joint flexibility and increase the likelihood of injury.
- Inadequate Rehabilitation: Not completing a full rehabilitation program after a previous ankle injury can leave the joint vulnerable to re-injury.
Symptoms of Syndesmotic Ankle Sprain
The symptoms of a syndesmotic ankle sprain, also known as a high ankle sprain, can vary in severity but often include:
- Pain: Pain is a common symptom and is typically located above the ankle joint between the tibia and fibula bones. The pain can range from mild ache to severe ache.
- Swelling: Swelling around the ankle joint, particularly above it, is another hallmark symptom. The swelling can develop quickly after the injury.
- Bruising: Bruising (ecchymosis) may occur on the outer and upper part of the ankle.
- Tenderness: The area above the ankle joint is often tender to the touch.
- Difficulty Walking: Due to pain and instability, walking or bearing weight on the affected leg can be challenging.
- Limited Range of Motion: Individuals may experience a reduced range of motion in the ankle joint.
- Pain with Certain Movements: Activities that involve dorsiflexion (pointing the toes upward) or rotation of the ankle can be particularly painful.
- Feeling of Instability: Some individuals report a sense of instability or a “giving way” sensation in the ankle.
- Difficulty Going Up or Down Stairs: Activities that require ankle dorsiflexion, such as stair climbing, can be painful and difficult.
- Pain During Weight-Bearing: Pain often worsens when you put weight on the affected ankle, making walking or standing uncomfortable.
- Pain with Passive Movements: You may experience pain when someone else gently moves your ankle, such as during a physical examination.
- Crepitus: In some cases, there may be a sensation of crepitus, which is a crackling or popping sound or feeling when moving the ankle.
- Difficulty Weight-Shifting: Shifting your weight from side to side on the affected leg can be challenging due to pain and instability.
- Stiffness: The ankle may feel stiff, particularly in the morning or after periods of inactivity.
- Numbness or Tingling: In more severe cases, there may be numbness or tingling in the affected leg or foot due to nerve irritation or compression.
- Pain That Persists: While some ankle sprains improve with rest and time, syndesmotic sprains often have more prolonged pain and a slower recovery period.
Diagnosis
The diagnosis of a syndesmotic ankle sprain, or high ankle sprain, typically involves a combination of clinical evaluation and imaging studies. Here’s how it’s typically diagnosed:
- Clinical Examination: A healthcare provider, often an orthopedic specialist or sports medicine physician, will conduct a thorough physical examination of your ankle. They will assess for signs of tenderness, swelling, bruising, and stability. They may also perform specific tests to evaluate the syndesmotic ligaments and joint stability, such as the “squeeze test” or “external rotation stress test.”
- Medical History: Your doctor will ask about the circumstances of the injury, your symptoms, and any previous ankle injuries or relevant medical history.
- Imaging Studies: X-rays are often the first imaging study used to rule out fractures and assess the alignment of the tibia and fibula. If the X-rays do not provide a clear diagnosis but a high ankle sprain is still suspected, more advanced imaging studies such as MRI (Magnetic Resonance Imaging) or CT (Computed Tomography) scans may be ordered. These can help visualize the ligaments and provide a more detailed assessment of the injury.
- Ultrasound: In some cases, ultrasound imaging may be used to assess ligament integrity, especially if other imaging methods are inconclusive.
- Comparison with the Uninjured Ankle: Comparing the injured ankle with the uninjured one can help the healthcare provider identify differences in stability and function.
Medical Treatment of Syndesmotic Ankle Sprain
Medical treatment for a syndesmotic ankle sprain, also known as a high ankle sprain, varies based on the severity of the injury.
- R.I.C.E. Protocol: The initial treatment often follows the R.I.C.E. protocol, which stands for Rest period, Ice apply, Compression, and Elevation. Resting the ankle reduces stress on the injured ligaments, while ice helps control swelling, compression with an elastic bandage supports the injured area, and elevation minimizes swelling.
- Immobilization: In moderate to severe cases, your healthcare provider may recommend using a walking boot or cast to immobilize the ankle and allow the ligaments to heal. Crutches may be necessary to avoid putting weight on the injured ankle area.
- Pain Management: Over-the-counter or prescription pain medications may be recommended to manage pain and inflammation. Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used for pain relief purposes.
- Follow-Up Care: Regular follow-up appointments with your healthcare provider or orthopedic specialist are crucial to monitor your progress, adjust your treatment plan as needed, and ensure that your ankle heals properly.
Physiotherapy Treatment
Physiotherapy plays a significant role in the treatment and rehabilitation of syndesmotic ankle sprains (high ankle sprains). Here’s how physiotherapy is typically used in the treatment process:
- Initial Assessment: A physiotherapist will begin by conducting a thorough assessment of your ankle. They will evaluate the extent of the injury, the range of motion, strength, balance, and any associated muscle imbalances.
- Pain Management: If you’re experiencing pain and inflammation, the physiotherapist may use modalities such as ice, heat, or ultrasound to help alleviate discomfort and reduce swelling.
- Range of Motion Exercises: The physiotherapist will guide you through exercises designed to restore normal ankle range of motion. Gentle movements and stretches are often incorporated.
- Strengthening Exercises: Specific exercises to strengthen the muscles around the ankle joint, particularly the calf muscles and the muscles that support ankle stability, are crucial. These exercises help improve joint stability and prevent future injuries.
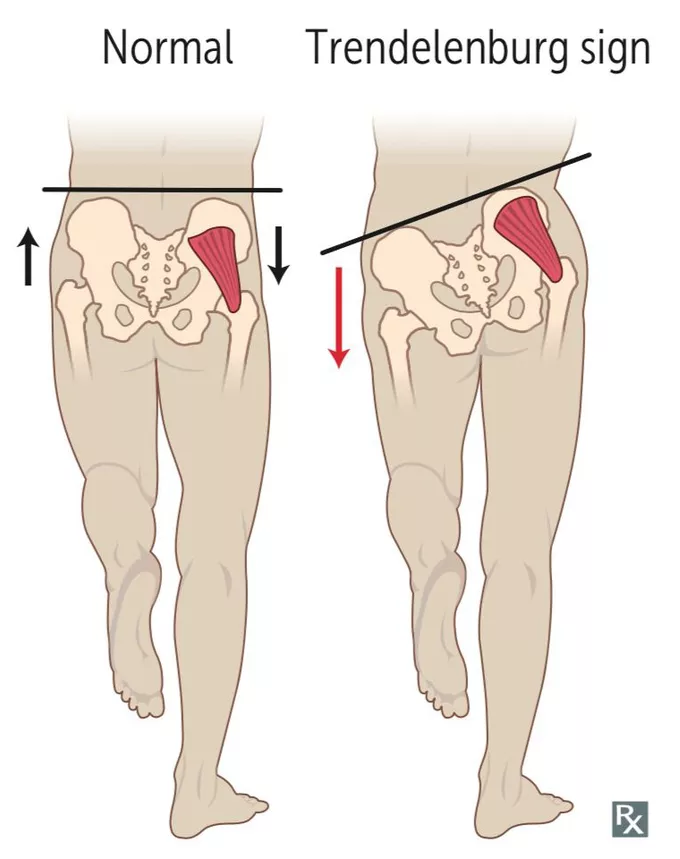
- Balance and Proprioception Training: High ankle sprains can disrupt your sense of balance and proprioception (awareness of joint position). Balance exercises on various surfaces, such as foam pads or balance boards, can help retrain these abilities.
- Functional Training: As your ankle heals, the physiotherapist will progress to functional exercises that mimic activities you do in daily life or sports. This helps prepare you for a safe return to your normal activities.
- Gait Training: Learning to walk without a limp or altered gait is an important part of rehabilitation. The physiotherapist will work with you to ensure proper walking mechanics.
- Bracing and Support: If necessary, the physiotherapist may recommend ankle bracing or taping techniques to provide extra support during the early stages of rehabilitation or when returning to sports.
- Education: You’ll receive guidance on self-management techniques, including how to manage pain, continue exercises at home, and recognize signs of reinjury.
- Progress Monitoring: Throughout the rehabilitation process, your physiotherapist will regularly assess your progress and adjust the treatment plan as needed.
- Return to Activity: The ultimate goal is to safely return to your normal activities or sports. The physiotherapist will provide guidance on when it’s appropriate to resume these activities and how to do so gradually to minimize the risk of re-injury.
Exercise
Exercise is an essential component of the rehabilitation process for a syndesmotic ankle sprain (high ankle sprain). Here are some exercises that are commonly prescribed by physiotherapists to help in the recovery and strengthening of the affected ankle:
- Range of Motion Exercises: Gentle ankle movements to improve flexibility and reduce stiffness. This may include ankle circles, toe-pointing, and dorsiflexion (lifting your toes towards your shin).
- Resistance Band Exercises: Using resistance bands to perform exercises that strengthen the ankle muscles. Examples include resisted ankle dorsiflexion and resisted ankle eversion.
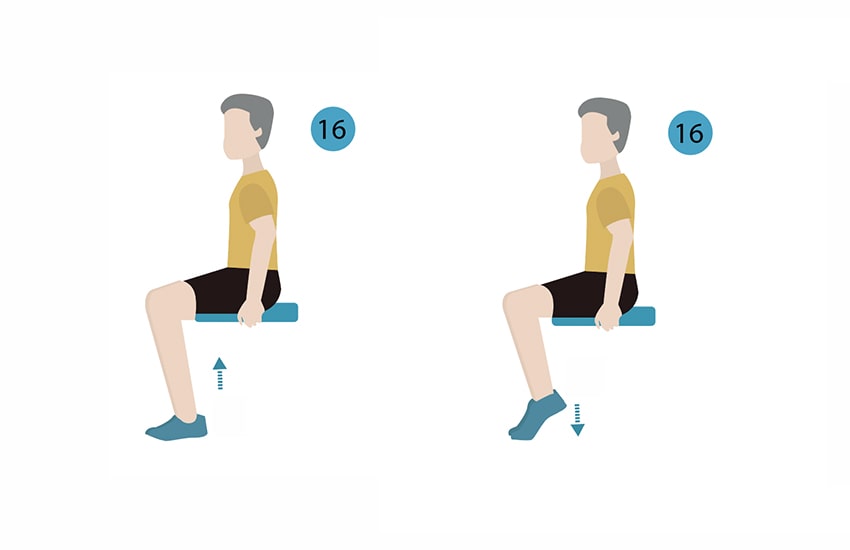
- Calf Raises: These exercises help strengthen the calf muscles, which play a crucial role in ankle stability. Perform both seated position and standing position calf raises.
- Toe Tapping: While seated, tap your toes on the ground to work on ankle mobility and improve blood circulation.
- Alphabet Exercises: Write the alphabet with your big toe, focusing on precise and controlled movements. This helps with ankle mobility and coordination.
- Balancing Exercises: Stand on one foot, progressing to more challenging stances like single-leg stands on an unstable surface (e.g., foam pad or pillow). This improves balance and proprioception.
- Heel Walks and Toe Walks: Walking on your heels and toes helps improve ankle strength and coordination.
- Resistance Band Inversion and Eversion: Attach a resistance band to a stationary object and perform ankle inversion (turning your sole inward) and eversion (turning your sole outward) exercises.

- Single-Leg Squats: Once you have regained some strength and stability, progress to single-leg squats to further strengthen the ankle and leg muscles.
- Stair Exercises: If your rehabilitation has advanced, you can perform controlled stair climbs to work on strength and balance.

- Resistance Band Plantarflexion: Attach a resistance band to a stationary object, sit down with your knee extended, and loop the band around your forefoot. Push your foot downward against the resistance to strengthen the ankle’s plantar flexor muscles.
- Eccentric Calf Raises: Stand on the edge of a step with the patient’s heels hanging off. Rise up on your toes using both feet, then lift the patient’s uninjured foot off, and slowly lower your injured foot below the step level. This eccentric exercise can help improve calf muscle strength.
- Ankle Dorsiflexion with Towel: Sit with your foot on a towel on a smooth surface. While keeping your heel on the ground, use your toes to scrunch the towel toward you to work on dorsiflexion strength.
- Towel Scrunches: Place a small towel on the floor and use your toes to scrunch it up toward you. This exercise can help improve toe and intrinsic foot muscle strength.
- Ankle Alphabet in the Air: While seated or lying down, draw the letters of the alphabet in the air with your big toe. This helps improve the range of motion and control.
- Bosu Ball Exercises: Exercises on a Bosu ball or other unstable surface can be done once you’ve regained some stability to test your balance and improve your ankle muscles.
- Resistance Band Calf Stretch: Sit on the floor with your legs extended. Loop a resistance band around the ball of your foot and gently pull your toes towards you, stretching your calf muscles.
- Strengthening with a TheraBand: Attach a TheraBand to a fixed point and loop it around your forefoot. Perform dorsiflexion, eversion, and inversion exercises with the band for resistance.
- Treadmill or Elliptical Training: Under the guidance of your physiotherapist, you may eventually incorporate low-impact treadmill or elliptical workouts to improve cardiovascular fitness while minimizing impact on the injured ankle.

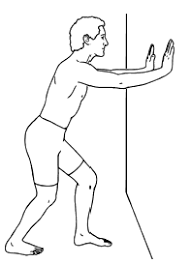
- Calf Stretch: Stand facing a wall, place the patient’s hands on the wall for support, and step one foot back. Keep the injured foot forward with the knee slightly bent and the heel on the ground. Gently lean forward to stretch the calf muscle.

- Lateral Band Walks: Place a resistance band around the patient’s ankles and take small steps sideways. This exercise helps strengthen the muscles that support ankle joint stability.
- Step-Ups: Using a stable step or platform, step up with the injured leg and then step back down. This exercise can be adjusted in height to gradually increase the challenge.

- Bosu Ball Balancing: Stand position on a Bosu ball with the flat side down, focusing on maintaining balance. This exercise is excellent for improving ankle proprioception and stability.
- Plyometric Exercises: Once you’ve progressed in your rehabilitation, plyometric exercises like jumping drills and hopping can be introduced to improve power and coordination. Ensure your physiotherapist approves of these exercises before attempting them.
- Agility Ladder Drills: Using an agility ladder on the ground, perform various footwork patterns to enhance coordination and agility. Start with slow, controlled movements.
- Towel Scrunches with Weight: Place a towel on the floor and put a small weight (e.g., a small dumbbell or water bottle) on one end. Use your toes to scrunch the towel towards you, lifting the weight. This exercise further strengthens the intrinsic foot muscles.
- Mini-Trampoline (Rebounder) Exercises: Gentle bouncing on a mini-trampoline can improve ankle mobility and coordination while minimizing impact.
- Isometric Contractions: Perform isometric contractions by pushing your foot against a stationary object, such as a wall or floor, in various directions (dorsiflexion, plantarflexion, inversion, and eversion). Hold each contraction for several seconds.
- Ankle Circles with Resistance: Sit with your leg extended and loop a resistance band around the ball of your foot. Move your ankle in circular motions in both directions against the resistance of the band to improve mobility.
- Single-Leg Balance on Foam: Stand on one foot on a foam pad or cushion, challenging your balance. The patient can progress this exercise by closing your eyes or performing small movements while balancing.
- Elastic Band Torsion Resistance: Attach an elastic band to a stationary object and loop it around your ankle. Perform slow, controlled inward and outward twisting motions to strengthen the ankle’s eversion and inversion muscles.
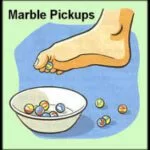
- Marble Pickup: Place a few marbles on the floor, use your toes to pick them up, and place them in a container. This exercise enhances toe dexterity and strength.
- Towel Stretch: Sit with your leg extended and loop a towel around the ball of your foot. Gently pull the towel towards you to stretch the calf and Achilles tendon.
- Soleus Stretch: While facing a wall, stand with one foot behind the other. Bend both knees, keeping the back heel on the floor. This targets the deeper calf muscle, the soleus muscle.
- Stair Descents: Once you’re comfortable with stair climbs, practice controlled descents by slowly lowering your body using the injured ankle. Hold onto a railing for support if necessary.
- Toe Tapping on a Resistance Band: Place a resistance band under the ball of your foot and hold the ends with your hands. Tap your toes against the resistance of the band to strengthen the ankle’s dorsiflexor muscles.
- Lateral Hops: Jump laterally from one side to the other, landing softly on the balls of your feet. Ensure your ankles are stable before attempting this exercise.
- Ankle Pumps: While seated, flex and extend your foot at the ankle joint to encourage blood flow and reduce swelling.

- Single-Leg Stand with Eyes Closed: Once you’re comfortable with single-leg balancing, try doing it with your eyes closed to challenge your proprioception.
- Sitting Heel Raises: While seated, lift both heels off the ground and hold for a few seconds. This exercise helps maintain ankle strength and mobility.

Surgery
Surgery for a syndesmotic ankle sprain, while not always necessary, may be recommended in severe cases where there is significant ligament damage or fractures. Here’s an overview of the surgical procedure and what to expect:
Indications for Surgery:
Surgery may be considered if:
The syndesmotic ligaments are severely torn and not likely to heal properly without surgical intervention.
There are associated fractures of the tibia or fibula that require stabilization. Conservative treatments have not yielded sufficient improvement in pain, stability, or function.
Types of Surgery:
There are several surgical techniques for treating syndesmotic ankle injuries, including:
- Syndesmotic Screw Fixation: A screw is placed through the tibia and fibula bones to hold them together and stabilize the syndesmosis. This prevents excessive movement and allows for proper healing of the ligaments.
- Suture Button Fixation: This technique involves using a suture button device to secure the tibia and fibula, providing dynamic stabilization. It allows for limited motion during the healing process.
- Tightrope Fixation: A tightrope system uses a strong suture material to maintain the correct alignment and stability of the syndesmosis.
The Surgical Procedure:
The surgery procedure is typically performed under general anesthesia or regional anesthesia. The surgeon makes an incision near the ankle to access the syndesmotic area. Depending on the chosen technique, screws, sutures, or other devices are used to stabilize the syndesmosis and, if necessary, repair any associated fractures. The incision is then closed, and the ankle is usually immobilized in a cast or brace.
Recovery and Rehabilitation:
After surgery, you can expect a period of non-weight-bearing or partial weight-bearing on the affected leg. You’ll work closely with a physiotherapist to start gentle range of motion exercises and gradually progress to weight-bearing activities. The length of the recovery period varies but can take several months.
Potential Complications: Like any surgical procedure, there are potential risks and complications, such as infection, nerve damage, or hardware irritation. It’s essential to follow your surgeon’s post-operative instructions carefully to minimize these risks.
The decision to undergo surgery for a syndesmotic ankle sprain is typically made after a thorough evaluation by an orthopedic specialist. They will consider the severity of the injury, the presence of fractures, and your individual circumstances. Ankle surgery is usually reserved for cases where conservative treatments are unlikely to provide adequate healing and recovery. Your surgeon will discuss the benefits, risks, and expected outcomes with you before proceeding.
Prevention
Preventing a syndesmotic ankle sprain, or high ankle sprain, involves strategies to strengthen and protect the ankle joint, improve balance, and reduce the risk of injury. Here are some prevention tips:
- Ankle Strengthening Exercises: Incorporate regular exercises to strengthen the muscles around the ankle joint, particularly the calf muscles and the muscles that support ankle stability. Strong muscles provide better joint support.
- Balance and Proprioception Training: Engage in balance and stability exercises, such as standing on one leg or using balance boards, to improve proprioception (awareness of joint position) and reduce the risk of twisting your ankle.
- Proper Footwear: Wear appropriate shoes for your activities, ensuring they provide adequate support and cushioning. For sports or activities that carry a higher risk of ankle injury, consider shoes with ankle support or orthotic inserts if recommended.
- Ankle Bracing or Taping: If you have a history of ankle instability or have previously experienced ankle sprains, consider using ankle braces or taping techniques during physical activities. Consult with a healthcare professional or physiotherapist for guidance on the best approach.
- Warm-Up and Stretching: Prior to physical activity, perform a proper warm-up routine to prepare your muscles and joints for the demands of exercise. Include dynamic stretching exercises to increase joint mobility.
- Technique and Form: Ensure you use proper technique when participating in sports or activities that involve running, jumping, or quick changes in direction. Improper form can improve the risk of injury.
- Adequate Rest and Recovery: Allow your body sufficient time to recover between intense workouts or sports activities. Overtraining can lead to fatigue and increase the risk of injury.
- Terrain Awareness: When engaging in outdoor activities, be aware of your surroundings and any uneven or unstable terrain. Take extra caution when walking or running on unfamiliar surfaces.
- Avoiding Overuse: Avoid excessive repetitive movements or activities that can strain the ankle joint, such as long-distance running without proper training or sudden increases in activity level.
- Stay Hydrated: Proper hydration helps maintain muscle function and reduces the risk of muscle fatigue and cramping, which can contribute to ankle injuries.
- Regular Physical Checkups: If you have a history of ankle injuries or concerns about your ankle health, consult with a healthcare provider or sports medicine specialist. They can assess your risk factors and provide guidance on prevention.
- Safe Rehabilitation: If you’ve previously had an ankle injury, ensure that you complete a comprehensive rehabilitation program to restore strength, stability, and function to the injured ankle.
Complication
Syndesmotic ankle sprains, like any injury, can have potential complications if not properly managed or if they are severe. Some possible complications of a syndesmotic ankle sprain include:
- Chronic Ankle Instability: Inadequate rehabilitation or incomplete healing of the ligaments can lead to chronic ankle instability. This means the ankle may continue to feel “giving way” or unstable, increasing the risk of future sprains.
- Persistent Pain: Some individuals may experience persistent pain in the ankle even after rehabilitation. This can be due to ongoing ligament damage, joint instability, or other factors.
- Post-Traumatic Arthritis: In severe cases or when fractures are involved, the risk of developing post-traumatic arthritis in the ankle joint increases. This can result in chronic aches, stiffness, and reduced mobility.
- Loss of Range of Motion: Scar tissue formation or improper healing can lead to a loss of ankle joint range of motion, making it difficult to move the foot as freely as before.
- Nerve or Blood Vessel Damage: In rare instances, severe injuries can cause damage to nearby nerves or blood vessels. This may result in numbness, tingling, or circulation issues in the affected foot.
- Recurrent Syndesmotic Sprains: Once an ankle has sustained a syndesmotic sprain, it may be more prone to future syndesmotic sprains due to ligament laxity or altered joint mechanics.
- Functional Limitations: Some individuals may experience limitations in their ability to participate in certain sports or activities due to persistent symptoms or instability.
- Psychological Impact: Chronic pain and limitations in physical activities can have psychological effects, such as anxiety or depression, which may require additional support and management.
Home Advice
If you’re recovering from a syndesmotic ankle sprain and receiving medical care, there are several home care tips and advice to aid in your recovery and promote healing. However, always follow your healthcare provider’s specific recommendations and treatment plan.
- Rest: Give your injured ankle adequate rest. Avoid putting weight on it as recommended by your healthcare provider.
- Elevate: Elevate your injured leg whenever possible, especially during the first few days. Elevating the ankle helps reduce swelling.
- Ice: Apply ice to the affected area for 15-20 minutes every 2-3 hours during the initial 48 hours. Use a cloth or towel wrap to protect the patient’s skin from direct contact with the ice.
- Compression: If advised by your healthcare provider, use an elastic bandage or compression wrap to help reduce swelling. Make sure it is not too tight wrap to avoid restricting blood flow.
- Medication: Take over-the-counter pain relievers or prescribed medications as directed by your healthcare provider to manage pain and inflammation. Avoid excessive use and follow recommended dosages.
- Follow R.I.C.E. Protocol: Remember the R.I.C.E. protocol: Rest, Ice, Compression, and Elevation. This acronym summarizes key steps for managing ankle sprains.
- Bracing or Taping: If your healthcare provider recommends it, use any prescribed ankle braces or taping techniques to provide additional support and stability during the early stages of recovery.
- Avoid Alcohol and Smoking: These substances can slow down the healing process. Try to minimize or avoid them during your recovery.
- Healthy Diet: Eat a well-balanced and healthy diet rich in nutrients to support the healing process. Adequate protein, vitamins, and minerals are useful.
- Stay Hydrated: Proper hydration is crucial for the patient’s overall health and recovery.
- Follow Rehabilitation Exercises: Be consistent with the prescribed exercises and rehabilitation program provided by your physiotherapist. These exercises are crucial for regaining strength and stability in your ankle.
- Avoid High-Risk Activities: Refrain from activities that may increase the risk of re-injury or aggravate your condition. Consult your healthcare provider about when it’s safe to return to specific activities.
- Monitor Your Progress: Pay attention to how the patient’s ankle is healing. Report any unusual or worsening symptoms to the patient’s healthcare provider promptly.
- Ergonomics: Ensure your home environment is safe and supportive of your recovery. Remove tripping hazards, secure rugs, and arrange furniture to minimize the risk of falls.
- Psychological Support: Don’t underestimate the emotional impact of an injury. Seek support from friends, family members, or a mental health professional if needed.
FAQ
What is a syndesmotic ankle sprain?
syndesmotic ankle sprain, also known as a high ankle sprain, is an injury to the syndesmosis, which is the group of ligaments that connect the tibia and fibula bones in the lower leg just above the ankle joint.
What causes a syndesmotic ankle sprain?
These sprains are often caused by sudden twisting or rotational movements of the ankle, such as those that occur in sports, falls, or accidents.
What are the common symptoms of a syndesmotic ankle sprain?
Common symptoms include pain above the ankle joint, swelling, bruising, difficulty walking, tenderness, and a sense of instability.
What are the potential complications of a syndesmotic ankle sprain?
Complications may include chronic ankle instability, persistent pain, post-traumatic arthritis, loss of range of motion, and recurrent syndesmotic sprains.
Can I prevent a syndesmotic ankle sprain?
Yes, preventive measures include strengthening ankle muscles, balance training, wearing proper
footwear, and using supportive braces or taping during high-risk activities.