Calcification
Table of Contents
What is a Calcification?
Calcification refers to the accumulation of calcium salts in body tissues, often leading to the hardening and loss of elasticity in those tissues. It can occur in various parts of the body, including arteries, heart valves, and even the brain.
In the medical context, calcification can be associated with conditions such as atherosclerosis, heart disease, and kidney stones.
Type Of Calcification
Calcification can occur in various forms and locations throughout the body. Here are some common types of calcification:
- Dystrophic Calcification: This type of calcification occurs in damaged or degenerated tissues, often as a response to inflammation or injury. It’s seen in conditions like atherosclerosis, where calcium deposits accumulate in artery walls.
- Metastatic Calcification: This occurs when there is an elevated level of calcium in the bloodstream, leading to the deposition of calcium in otherwise normal tissues. It can be caused by hypercalcemia (high blood calcium levels) due to various reasons, such as hyperparathyroidism or kidney failure.
- Vascular Calcification: Refers to the calcification of blood vessels, particularly arteries. It’s commonly associated with atherosclerosis, which is the hardening and narrowing of arteries due to the buildup of fatty plaques.
- Dental Calculus: Also known as tartar, dental calculus forms on teeth due to the mineralization of dental plaque. It’s a form of calcification that can lead to gum disease and other oral health issues.
- Soft Tissue Calcification: Calcification can occur in soft tissues such as muscles, tendons, and ligaments. It’s often associated with conditions like calcific tendinitis, where calcium deposits form within tendons.
- Kidney Stones (Renal Calculi): Kidney stones are formed when minerals, including calcium, crystallize in the kidneys. These stones can cause significant pain and urinary problems.
- Brain Calcification: Brain calcification can occur due to a variety of causes, including aging, infections, and genetic disorders. It might be visible on brain imaging scans like CT scans or MRIs.
- Breast Calcifications: These are small deposits of calcium that can appear in breast tissue. They might be detected on mammograms and can have various causes, including benign conditions or early breast cancer.
- Prostate Calcifications: Calcifications can occur in the prostate gland and might be detected during medical imaging. They are often benign but can be associated with prostate conditions.
- Corneal Calcification: Refers to the accumulation of calcium deposits in the cornea of the eye, potentially affecting vision.
- Thyroid Calcification: Calcifications in the thyroid gland might be associated with thyroid nodules or other thyroid conditions.
- Medial Calcification: This refers to calcification that occurs in the middle layer of blood vessels, particularly in medium and small arteries. It’s often associated with conditions like diabetes and chronic kidney disease.
- Aortic Valve Calcification: Calcification of the aortic valve can lead to aortic stenosis, a condition where the valve becomes narrowed and restricts blood flow from the heart.
- Mitral Annular Calcification: This involves the calcification of the fibrous ring around the mitral valve in the heart. It’s often a benign condition but can be associated with certain heart conditions.
- Pulmonary Valve Calcification: Calcification of the pulmonary valve can cause pulmonary valve stenosis, where the valve’s opening becomes narrowed, affecting blood flow from the heart to the lungs.
- Cerebral Calcification: Calcification in brain tissues can have various patterns and causes, including dystrophic, metastatic, and idiopathic calcifications. The brain’s many regions can be impacted.
- Psammoma Bodies: These are small, round calcium deposits often found in certain tumors, such as papillary thyroid carcinoma and serous ovarian tumors.
- Calciphylaxis: This rare condition involves extensive calcification of small blood vessels in the skin and fatty tissues, leading to painful skin ulcers and necrosis.
- Choroidal Calcification: Refers to calcification in the choroid layer of the eye, which can be visible in eye imaging studies and might be associated with certain ocular conditions.
- Idiopathic Calcification: In some cases, calcification occurs without a clear underlying cause and is referred to as idiopathic calcification. This can happen in various tissues.
- Vascular Media Calcification: This type of calcification specifically affects the media layer of blood vessels. It’s often associated with disorders like arteriosclerosis or chronic kidney disease.
- Pancreatic Calcification: Calcification can occur in the pancreas and might be seen on imaging studies. It can be linked to conditions like chronic pancreatitis
Causes of Calcification
Calcification can have various causes depending on the specific location in the body. Here are a few common causes:
- Atherosclerosis: In blood vessels, calcification can occur as a result of atherosclerosis, a condition where fatty deposits build up on artery walls. Over time, these deposits can harden and calcify, leading to reduced blood flow and an increased risk of cardiovascular events.
- Heart Valves: Heart valves can also calcify due to aging or conditions like valvular stenosis or regurgitation. This can lead to reduced valve function and potential heart problems.
- Soft Tissues: In soft tissues, such as muscles or tendons, calcification can occur as a response to injury or inflammation. This is often seen in conditions like tendinitis or other chronic inflammatory conditions.
- Kidney Stones: Kidney stones are formed when certain minerals, including calcium, accumulate in the kidneys and crystallize. These crystals can come together to form stones that can cause pain and blockages.
- Brain: In the brain, calcification can occur due to a variety of factors, including aging, infections, or genetic disorders. Calcifications in the brain might be visible on imaging scans like CT scans or MRIs.
- Dental Calculus: Dental calculus, or tartar, forms on teeth due to the mineralization of dental plaque. It may aggravate oral health problems such as gum disease.
- Soft Tissue Injury: In response to chronic injuries or repetitive trauma, the body might deposit calcium in soft tissues like muscles and tendons as a part of the healing process. This can sometimes lead to calcific tendinitis or myositis ossificans.
- Breast Tissue: Calcifications can appear in breast tissue, often seen on mammograms. They might be benign or associated with conditions like fibrocystic changes or even early breast cancer.
- Prostate Gland: Prostate calcification can occur as men age. It might be linked to chronic prostatitis or other prostate-related issues.
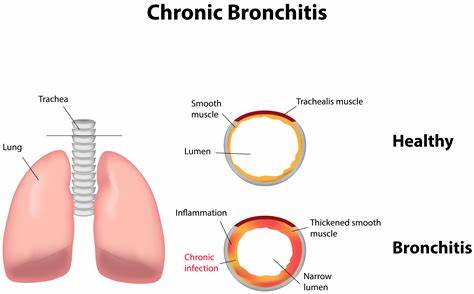
- Lung Tissue: Calcification in the lung tissue can sometimes result from past infections, such as tuberculosis, or from certain types of lung nodules.
- Soft Tissue Sarcomas: Certain types of soft tissue sarcomas can cause the deposition of calcium within tumors. This might be visible on imaging studies.
- Skin: Skin calcification can occur in conditions like calcinosis cutis, where calcium deposits form under the skin due to various causes, including autoimmune disorders.
- Eye: Calcification can also occur in the eye’s tissues, such as the cornea or the lens, sometimes causing vision issues.
- Thyroid Gland: Thyroid gland calcification might be seen in some thyroid nodules, which could be benign or cancerous.
Risk Factor
Certainly, here are some common risk factors that can increase the likelihood of developing calcification in various parts of the body:
- Age: As we age, the risk of calcification tends to increase. Aging tissues may become less efficient at regulating calcium levels.
- Atherosclerosis Risk Factors: Risk factors for atherosclerosis, such as high blood pressure, high cholesterol, smoking, and diabetes, can also contribute to calcification of blood vessels and heart valves.
- Chronic Inflammation: Conditions characterized by chronic inflammation, such as rheumatoid arthritis or chronic kidney disease, can promote calcification in affected tissues.
- Genetic Predisposition: Certain genetic factors might make some individuals more prone to developing calcification in specific tissues.
- Kidney Issues: Chronic kidney disease can lead to imbalances in calcium and phosphate levels in the blood, increasing the risk of calcification in various body tissues.
- Hormonal Imbalances: Certain hormonal imbalances, like those seen in hyperparathyroidism or disorders affecting vitamin D metabolism, can impact calcium regulation and potentially lead to calcification.
- Trauma and Injury: Repeated trauma or injury to a specific area can trigger the body’s response to deposit calcium, leading to calcification.
- Infections and Inflammatory Conditions: Chronic infections or inflammatory conditions in certain tissues can create an environment conducive to calcification.
- Radiation Exposure: Prolonged exposure to ionizing radiation can increase the risk of developing calcifications, especially in soft tissues.
- Certain Medical Treatments: Some medical treatments, such as certain cancer treatments or long-term use of certain medications, can contribute to calcification risk.
- Metabolic Disorders: Certain metabolic disorders, such as disorders of calcium and phosphate metabolism, can predispose individuals to calcification.
- Obesity: Obesity has been linked to an increased risk of developing atherosclerosis and other conditions associated with calcification.
Symptoms of Calcification
The symptoms of calcification can vary depending on the location and underlying cause. Here are some potential symptoms associated with calcification in different areas of the body:
- Arteries and Heart Valves: Calcification in arteries and heart valves might not cause noticeable symptoms initially. However, as it progresses, it can lead to reduced blood flow, chest pain (angina), shortness of breath, fatigue, and an increased risk of heart attack or stroke.
- Soft Tissues (Muscles, Tendons): Calcification in soft tissues can cause pain, limited range of motion, and discomfort in the affected area. Movement might be restricted due to the hardening of the tissue.
- Brain: Depending on the location and extent of calcification in the brain, symptoms can include headaches, neurological deficits, cognitive changes, and even seizures in some cases.
- Kidney Stones: Kidney stones caused by calcification can lead to severe pain in the back or side, pain during urination, frequent urination, blood in the urine, and discomfort in the lower abdomen.
- Breast Tissue: Calcifications in breast tissue might be detected during routine mammograms. While most calcifications are benign, certain patterns might require further evaluation to rule out breast cancer.
- Prostate Gland: Calcifications in the prostate might not cause symptoms. However, if they are associated with prostatitis or other prostate conditions, symptoms could include urinary issues, pain, or discomfort.
- Lung Tissue: Calcifications in the lung tissue might not cause noticeable symptoms. They are often detected incidentally on imaging tests.
- Skin: In cases of calcinosis cutis, where calcium deposits form under the skin, symptoms might include painful or tender lumps under the skin.
- Eye: Calcification in the eye’s tissues can affect vision, potentially causing blurred vision, light sensitivity, and discomfort.
- Thyroid Gland: Calcifications in the thyroid might not cause symptoms, but they could be detected during imaging tests or routine examinations.
Diagnosis
The diagnosis of calcification typically involves a combination of medical history, physical examination, and diagnostic imaging.
Medical History and Examination: The doctor will ask about your symptoms, medical history, and any relevant risk factors. They will also conduct a physical examination to assess the affected area and any associated symptoms.
Imaging Tests: Diagnostic imaging plays a crucial role in identifying calcification. Different types of imaging tests might be used depending on the suspected location of calcification:
- X-rays: X-rays can reveal the presence of calcification in bones and some soft tissues.
- Ultrasound: Ultrasound might be used to detect calcification in certain soft tissues, such as the breast or thyroid.
- Computed Tomography (CT): CT scans provide detailed images that can help identify calcification in various body parts, including the brain, blood vessels, and organs.
- Magnetic Resonance Imaging (MRI): MRI scans can detect calcification in soft tissues and organs, providing detailed images without using ionizing radiation.
Laboratory Tests: Blood tests might be performed to assess calcium and phosphate levels, especially if there is suspicion of metabolic disorders contributing to calcification.
Biopsy: In some cases, a biopsy might be performed to analyze tissue samples for calcification. This is more common when calcification is associated with specific conditions like breast calcifications.
Clinical Assessment: The combination of medical history, examination findings, and imaging results will help the healthcare provider determine the cause and potential implications of the calcification.
Medical Treatment
Medical treatment for calcification depends on the underlying cause and the specific location in the body.
- Managing Underlying Conditions: Treating the underlying condition that is causing calcification is often the primary focus. For example, managing atherosclerosis risk factors (like blood pressure and cholesterol) can slow the progression of arterial calcification.
- Medications: Depending on the situation, medications might be used to manage symptoms or slow the progression of calcification. For example, certain medications can help control blood pressure or cholesterol levels.
- Pain Management: In cases where calcification leads to pain, over-the-counter pain relievers or prescription medications might be recommended to manage discomfort.
- Anti-Inflammatory Treatment: In conditions involving inflammation, such as calcific tendinitis, anti-inflammatory medications might be prescribed to reduce pain and inflammation.
- Chelation Therapy: In certain cases, chelation therapy might be used to treat calcification. This involves using medications that can help remove excess minerals from the body.
Physiotherapy Treatment
Physical therapy and exercises can sometimes help improve mobility and reduce discomfort caused by calcification in muscles and tendons. Physiotherapy, also known as physical therapy, can play a crucial role in managing symptoms and improving mobility in cases of calcification affecting muscles, tendons, and other soft tissues. Here’s how physiotherapy might be used as a treatment approach:
- Pain Management: Physiotherapists can use various techniques such as manual therapy, massage, and modalities like heat or cold therapy to help manage pain associated with calcification.
- Range of Motion Exercises: Gentle exercises and stretches prescribed by a physiotherapist can help maintain or improve the range of motion in affected joints and tissues. This can be especially helpful in conditions like calcific tendinitis.
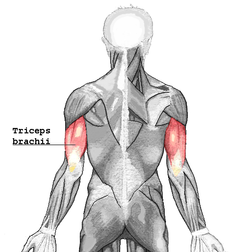
- Strengthening Exercises: Specific exercises can be designed to target the muscles surrounding the calcified area. Strengthening these muscles can help support the affected area and improve overall function.
- Modalities: Physiotherapy modalities such as ultrasound, electrical stimulation, or laser therapy might be used to reduce inflammation, promote healing, and relieve pain.
- Manual Therapy: Hands-on techniques performed by physiotherapists, such as joint mobilization and soft tissue manipulation, can help improve tissue mobility and alleviate discomfort.
- Posture and Movement Correction: Physiotherapists can identify and address any postural or movement issues that might be contributing to calcification-related pain or discomfort.
- Education: Physiotherapists can provide education on proper body mechanics, exercises, and lifestyle modifications that can help prevent further calcification-related issues and promote better overall musculoskeletal health.
- Home Exercise Programs: Physiotherapists often prescribe tailored exercise programs that patients can perform at home to continue their progress between sessions.
- Progress Monitoring: Physiotherapy treatment plans are usually progressive. The therapist will monitor your progress and adjust the treatment plan as needed to achieve the best possible outcomes.
- Preventing Recurrence: Physiotherapists can guide you on how to prevent future episodes of calcification-related pain or discomfort through proper exercises, ergonomics, and self-care strategies.
Exercises
Certainly, exercise can be beneficial for overall health and, in some cases, for managing symptoms related to calcification. However, the type and intensity of exercise you should engage in can vary depending on the location and severity of the calcification, as well as any underlying medical conditions. Here are some general guidelines:
- Consult Your Healthcare Provider: Before starting any new exercise routine, especially if you have calcification or related health concerns, it’s essential to consult your healthcare provider. They can provide personalized advice based on the patient’s medical history and current condition.
- Low-Impact Activities: If you’re experiencing pain or discomfort due to calcification, consider engaging in low-impact activities such as walking, swimming, or stationary cycling. These activities can help maintain cardiovascular fitness without putting excessive stress on joints or affected areas.
- Range of Motion Exercises: Gentle stretching exercises can help maintain or improve the flexibility of muscles and joints affected by calcification. Make sure to perform these exercises within a pain-free range of motion.
- Strengthening Exercises: Depending on the location of calcification, your healthcare provider or a physiotherapist might recommend specific strengthening exercises to target muscles surrounding the affected area. Strengthening these muscles can provide better support and stability of the muscles.
- Core Strengthening: Engaging in exercises that target the core muscles can help improve posture and support the spine, which might be beneficial in cases of back-related calcification.
- Balance and Stability Training: Balance exercises can help prevent falls and improve stability, which is important if you have calcification that affects your mobility.
- Avoid Overexertion: If you’re experiencing aches or discomfort during the exercise period, stop and rest. Pushing through an ache could worsen the patient’s condition.
- Gradual Progression: Start out slowly and build up to more intense and prolonged workouts over time. This approach can help prevent overexertion and reduce the risk of injury.
- Listen to Your Body: Pay attention to how your body responds to exercise. If you notice any increased pain, discomfort, or unusual symptoms, stop and consult your healthcare provider.
- Stay Hydrated: Proper hydration is important for overall health and can help prevent complications related to certain types of calcification, such as kidney stones.
- Balanced Approach: Remember that exercise should be part of a balanced approach to health. Adequate rest, proper nutrition, and other lifestyle factors play a role in managing conditions like calcification.
- Swimming: Swimming is a low-impact exercise that provides a full-body area workout. It is gentle on the joints and can help increase cardiovascular fitness and muscle strength.

- Yoga: Yoga combines stretching, flexibility, and gentle strength-building. It can be particularly useful for maintaining flexibility and reducing muscle tension in areas affected by calcification.

- Tai Chi: Tai Chi is a mind-body practice that involves slow, flowing movements. It can improve balance, coordination, and muscle strength while being gentle on the joints.
- Pilates: Pilates focuses on core strength, flexibility, and stability. It can help improve posture and target specific muscle groups affected by calcification.
- Cycling: Stationary cycling or outdoor biking is a low-impact cardiovascular exercise that can be gentle on the joints while providing an effective workout.

- Resistance Training: Using resistance bands, light weights, or bodyweight exercises can help strengthen muscles surrounding the affected area. Always start with light resistance and progress gradually.
- Stretching: Gentle stretching exercises can help maintain or improve flexibility in muscles and tendons, reducing the risk of stiffness caused by calcification.
- Aerobic Exercises: Low-impact aerobic exercises like brisk walking or using an elliptical machine can help improve cardiovascular fitness without putting excessive stress on joints.

- Water Aerobics: Water provides buoyancy, which can reduce impact on joints. Water aerobics classes can offer a fun and effective way to exercise.
- Balance and Stability Exercises: Incorporating exercises that challenge balance and stability, such as standing on one leg or using a balance board, can help improve proprioception and prevent falls.
- Walking: Walking is one of the simplest and most accessible forms of exercise. It can be done virtually anywhere and can help improve cardiovascular health, promote weight management, and boost mood.

- Elliptical Trainer: Using an elliptical machine provides a low-impact, full-body workout that engages both the upper and lower body.
- Rowing: Rowing machines provide a challenging cardiovascular workout while also engaging muscles in the arms, back, and legs.
- Stretch Bands: Resistance bands can be used for gentle strength training and stretching. They are particularly versatile and can be used to target various muscle groups.
- Stair Climbing: If appropriate for your condition, climbing stairs can provide an effective lower body workout that helps strengthen muscles and improve cardiovascular fitness.
- Dancing: Whether you join a dance class or simply dance at home, dancing is a fun way to get moving, improve coordination, and boost your mood.

- Group Fitness Classes: Consider joining group fitness classes like aerobics, Zumba, or spinning for a motivating and social exercise experience.
- Hiking: If you enjoy spending time outdoors, hiking on trails can provide both a physical workout and a connection to nature.
- Body weight Exercises: Body weight exercises like squats, lunges, push-ups, and planks can help build strength without the need for equipment.
- Circuit Training: Create a circuit that combines various exercises targeting different muscle groups. This can help keep your workout interesting and effective.
- Gentle Mobility Work: Incorporate gentle movements like tai chi or qigong to improve flexibility, balance, and relaxation.
- Sports and Recreational Activities: Engage in sports or recreational activities you enjoy, such as tennis, golf, or even gardening, which can contribute to your physical activity levels.
Surgery
Surgery might be considered as a treatment option for certain cases of calcification, especially when conservative treatments have not been effective or when the condition is causing significant discomfort or health risks. The decision to undergo surgery will depend on factors such as the location of the calcification, the underlying cause, the severity of symptoms, and your overall health. Here are a few scenarios where surgery might be considered:
- Heart Valve Replacement: Severe calcification of heart valves, especially the aortic valve, might require surgical intervention to replace the damaged valve with a prosthetic one.
- Kidney Stones: Large or problematic kidney stones caused by calcification might need to be surgically removed, often through procedures like extracorporeal shock wave lithotripsy (ESWL), ureteroscopy, or percutaneous nephrolithotomy.
- Joint Surgery: In some cases of severe calcification in joints, surgical procedures like arthroscopy or joint replacement might be considered to alleviate pain and improve joint function.
- Soft Tissue Removal: In conditions like calcific tendinitis or calcinosis cutis, surgery might involve removing the calcified deposits to relieve pain or discomfort.
- Brain Surgery: Extremely rare cases of extensive calcification in the brain might require surgery if they are causing neurological symptoms or compromising brain function.
- Vascular Surgery: Severely calcified arteries might necessitate vascular surgery to restore blood flow and reduce the risk of cardiovascular events.
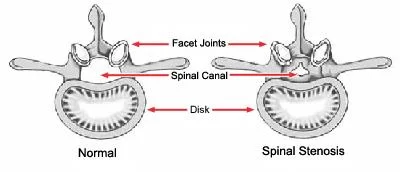
- Spinal Surgery: If calcification is affecting the spine and causing compression of spinal nerves, surgery might be needed to decompress the nerves and alleviate symptoms.
Prevention
Prevention strategies for calcification can vary based on the specific type of calcification and the underlying causes. Here are some general measures that might help prevent or reduce the risk of calcification in different contexts:
- Healthy Lifestyle: Adopt a healthy lifestyle that includes a balanced diet, regular exercise, and maintaining a healthy weight. This can help prevent conditions like atherosclerosis and reduce the risk of arterial and heart valve calcification.
- Bone Health: Consume an adequate amount of calcium and vitamin D to support bone health, but avoid excessive intake. Speak to a healthcare provider about the right balance for your individual needs.
- Hydration: Stay well-hydrated, especially in the case of kidney stones. Drinking enough water can help prevent the formation of certain types of kidney stones caused by calcium deposits.
- Blood Pressure and Cholesterol Management: Control your blood pressure and cholesterol levels through a healthy diet, regular exercise, and, if necessary, medication. This can help prevent calcification in arteries.
- Diabetes Management: Manage your blood sugar levels well if you have diabetes. Uncontrolled diabetes can contribute to arterial calcification.
- Avoid Smoking: Smoking is a significant risk factor for atherosclerosis and arterial calcification. Quitting smoking can help decrease the patient’s risk.
- Proper Dental Hygiene: Maintain good oral hygiene to prevent dental calculus (tartar) formation, which can lead to dental calcification.
- Protect Joints: Take care to avoid repetitive trauma or overuse of joints. This can help reduce the risk of soft tissue calcification.
- Balance Hormones: If you have hormonal imbalances, work with a healthcare provider to manage these conditions effectively.
- Regular Check-ups: Attend regular medical check-ups to monitor your health and catch any potential issues early.
- Medication Review: If you’re on long-term medication, discuss with your healthcare provider to ensure that the medications you’re taking do not contribute to calcification.
- Bone and Joint Health: For calcification related to soft tissues, engage in regular stretching and strengthening exercises to maintain flexibility and strength in muscles and tendons.
- Sun Exposure: Adequate sun exposure can help your body produce vitamin D, which is important for calcium regulation. However, be mindful of sun protection to prevent skin damage.
Complication
Complications arising from calcification can vary widely based on the location and underlying causes of the calcification. Here are some potential complications associated with different types of calcification:
Arterial and Heart Valve Calcification:
- Reduced Blood Flow: Severe calcification in arteries can lead to reduced blood flow, increasing the risk of cardiovascular events like heart attack or stroke.
- Heart Valve Dysfunction: Calcification of heart valves can lead to impaired valve function, potentially causing conditions like aortic stenosis or mitral valve regurgitation.
Kidney Stones (Renal Calculi)
- Obstruction and Infection: Large kidney stones can block the flow of urine, causing pain and increasing the risk of urinary tract infections.
- Kidney Damage: Chronic kidney stone formation might lead to kidney damage and impaired kidney function over time.
Brain Calcification:
- Neurological Symptoms: Extensive calcification in the brain might cause neurological symptoms such as seizures, cognitive impairment, and movement disorders.
- Underlying Conditions: Brain calcification can be associated with underlying conditions like Fahr’s disease, which might cause significant health issues.
Soft Tissue Calcification:
- Pain and Mobility Issues: Calcification in muscles, tendons, or ligaments can lead to pain, limited range of motion, and impaired mobility.
- Impaired Function: Depending on the location, calcification might affect the function of affected tissues, leading to discomfort or reduced function.
Dental Calcification:
- Gum Disease: Dental calculus can contribute to gum disease (periodontitis), which can lead to tooth loss if left untreated.
Eye Calcification
- Vision Impairment: Calcification in eye tissues can lead to vision problems and discomfort.
Thyroid Gland Calcification:
- Thyroid Dysfunction: Calcifications in the thyroid might be associated with thyroid nodules or disorders that affect thyroid function.
Skin Calcification:
- Pain and Discomfort: In cases of calcinosis cutis, painful lumps can form under the skin.
- Functional Impairment: Extensive skin calcification can lead to reduced skin flexibility and movement.
Home Advice
Certainly, here are some general home advice and self-care tips that you can consider, but please remember to consult with a healthcare professional for advice tailored to your specific situation:
Maintain a Healthy Lifestyle:
- Eat a balanced diet rich in fruits, green vegetables, whole grains, lean proteins, and healthy fats.
- Stay hydrated by drinking an adequate amount of drink water throughout the day period.
- Limit excessive consumption of foods high in sugar, salt, and saturated fats.
Stay Active:
- Engage in regular physical activity, such as walking, swimming, or yoga, based on your doctor’s recommendations.
- Incorporate stretching muscles and mobility exercises to maintain flexibility.
Manage Underlying Conditions:
- If you have chronic conditions like diabetes, hypertension, or kidney disease, work closely with your healthcare provider to manage them effectively.
Practice Oral Hygiene:
- Brush and floss your teeth regularly to prevent dental plaque buildup, which can lead to dental calcification.
Healthy Bone Habits:
- Consume foods rich in calcium and vitamin D components to support bone health.
- Engage in weight-bearing exercises to promote to patient’s bone strength.
Quit Smoking and Limit Drinking Alcohol: If the patient smokes, consider quitting smoking, and limit alcohol consumption to promote overall patient’s health.
Manage Stress:
- Practice stress-reduction techniques like deep breathing, meditation, or mindfulness to help manage stress.
Avoid Overuse of Joints:
- If you have conditions like calcific tendinitis, avoid overusing the affected joints and seek guidance from a healthcare provider on appropriate exercises.
Stay Informed:
- Learn about the patient’s specific condition and how to manage it effectively. Knowledge can empower the patient to make informed decisions.
Regular Check-ups:
- Attend routine medical check-ups to monitor your health and catch any potential issues early.
Follow Medical Recommendations:
- Adhere to any treatment plans, medications, or exercises recommended by your healthcare provider.
Stay Hydrated and Mind Your Diet:
- If you’re prone to kidney stones, consult your healthcare provider about dietary adjustments to prevent stone formation.
Monitor Symptoms:
- Keep track of any changes or symptoms related to calcification or underlying conditions. This information can be helpful during medical appointments.
FAQ
Calcification refers to the accumulation of calcium deposits in various tissues of the body. It can occur in bones, soft tissues, blood vessels, and organs.
Calcification can be caused by various factors, including aging, inflammation, injury, metabolic disorders, and underlying health conditions.
Symptoms depend on the location and cause of calcification. They can range from pain and reduced mobility to cardiovascular symptoms and neurological issues.
Diagnosis involves medical history, physical examination, imaging tests (X-rays, CT scans, MRI), blood tests, and sometimes biopsies.
Prevention strategies vary by type and cause of calcification. Maintaining a healthy lifestyle, managing underlying conditions, and following medical recommendations can help.
These calcium deposits can accumulate in one area or may occur in more than one location. If the deposits grow bigger or become more irritated, they can cause severe aches.
Calcification happens when calcium builds up in tissue areas, blood vessels, or organs, causing them to harden. Treatment will depend on the severity of the pain and the location of the calcification and can range from drug to surgery.
Calcification happens when tumors are no longer time able to regulate the movement of calcium in and out of their cells. This may be due to damage to the blood vessels, resulting in a localized hemorrhage (uncontrolled blood flow) within the tumor that kills some of the cells.
Calcium is a sign of how much fatty build-up (plaque) is in the patient, ‘s arteries because this build-up contains calcium. Plaques in the arteries of the patient’s heart are the main cause of heart attacks. If a piece of plaque breaks off a blood clot can form around it, blocking the flow of blood and the oxygen supply to the patient’s heart.