Proximal Hamstring tendinopathy
Table of Contents
What is Proximal hamstring tendinopathy?
- Proximal hamstring tendinopathy is the inflammation within the hamstring tendon, which is located on the outside of the back of the knee. Proximal hamstring tendinopathy is sometimes known as proximal hamstring tendonitis. Physiotherapy is an important treatment for proximal hamstring tendinopathy.
- The hamstring muscle in the leg has a tendon behind and to the outside of the knee. This can become inflamed as part of an overuse injury in sports that involve rapid acceleration and deceleration. Microscopic tears accumulate faster than they can be repaired, causing inflammation.
- You will feel pain in the tendons on the back of the knee on the outside. In the beginning, the pain is only felt following exercise, but as the condition progresses, it may become more intrusive and interfere with sports and day-to-day activities. Certain biomechanical problems and tightness of the muscles make this condition more likely. In the meantime, you might want to avoid any aggravating activities that may prolong the problem. It generally does not get better on its own. The first thing to do is to reduce the problem activities. Ice and anti-inflammatory drugs are helpful after exercise.
- Treatment includes first confirming the diagnosis, then establishing the causes. An MRI scan can be useful for excluding other problems. Treatment options may include very specific physiotherapy, short-wave treatment, or injections. Once you have recovered, good physio might be able to prevent this from coming back.
Tendonitis or tendinopathy?
- The term “tendonitis” is most commonly used, but generally, this is not strictly accurate. Tendonitis refers to an acute inflammation of the tendon where, in actual fact, unless the injury is very recent, the pain is more likely due to long-term overuse and degeneration of the tendon. A broader and more accurate term for this type of tendon injury is tendonitis or tendinopathy.
Anatomy of Hamstring muscle:
The hamstring muscle is one of the 3 posterior thigh muscles in between the hip & the knee (from medial to lateral:
- Semimembranosus
- Semitendinosus
- Biceps femoris muscle
- The hamstrings are quite susceptible to injury.
- A hamstring strain is a common leg injury involving a tear in one or more of the hamstring muscles.
- A hamstring strain can range from mild to very severe involving a complete tear of the hamstring muscle.
You have four hamstring muscles: semimembranosus and semitendinosus (medially) and biceps femoris – short and long heads (laterally).
Biceps Femoris:
- Origin: Ischial tuberosity
- Insertion: The fibular head and lateral condyle of the tibia
- Function: Knee flexion, lateral rotation of the tibia, and hip extension
- Innervation: Tibial nerve
- Vascular supply: Perforating branches of the deep femoral artery
Semitendinosus
- Origin: Lower, medial surface of the ischial tuberosity
- Insertion: Medial tibia (pes anserinus)
- Action: Flexion of the knee joint, Extension of the hip joint, & Medial rotation of the tibia (with knee flexion)
- Innervation: Tibial nerve
- Blood supply: Perforating branches of the deep femoral artery
Semimembranosus
- The semimembranosus muscle is flattened and broad. It is located underneath the semitendinosus.
- Origin: Ischial tuberosity
- Insertion: Medial tibial condyle
- Function: Flexion of the knee joint, Extension of the hip joint, and Medially rotates the thigh at the hip joint and the leg at the knee joint.
- Nerve supply: Tibial nerve
- Blood supply: Perforating branches of the deep femoral artery.
How does proximal hamstring tendinopathy occur?
- Proximal hamstring tendinopathy happens most commonly in sports involving lots of acceleration and deceleration. The hamstring muscle-tendon transmits forces produced by the hamstring muscle to the lower leg to control the movement of the leg at the knee joint. Repetitive use of the hamstring muscle and, therefore, the hamstring tendon can cause microscopic tears within the tendon. The body acts to repair these microscopic tears by commencing an inflammatory response. This inflammation within the tendon is called tendinopathy.
- Inflammation or degeneration of the hamstring tendon happens at the points it inserts into the tibia (shin bone) and fibula. This is a result of overuse or may also develop after a partial rupture of a tendon that has not healed properly. Most commonly, it is the hamstring tendon that is involved.
Epidemiology/Etiology of Proximal Hamstring Tendinopathy
- With tendinopathy, there is a multitude of factors that can contribute to the etiology. These factors are usually load-related. Some extrinsic factors include training errors such as an increase in training volume and intensity too quickly (often with the introduction of sprint work, lunges, hill running, and hurdles). These type of training errors has been reported in the research as training errors preceding proximal hamstring tendinopathy. With this type of activity, the hamstring needs to contract and lengthen when the hip is in flexion. This can lead to a higher tensile and compressive load at the tendon insertion. Another cause of the symptoms may be excessive static stretching, i.e. in yoga or Pilates. These types of exercises involve sustained end-range hip flexion postures. Long periods of sitting can also cause it in some patients.
Risk Factors of the proximal hamstring tendinopathy
Intrinsic factors:
- Malalignments
- Leg length discrepancy
- Imbalance
- Decreased flexibility
- Joint laxity
- Female gender
- Age – Reduction in muscle fiber size & number are associated with advancing in age, this leads to losses of mass & strength.
- Overweight
- Proprioceptive deficiency
- Ischial tuberosity tenderness
- Core weakness
- Pelvic dysfunction
- Previous injury – Strength is reduced by previous hamstrings, knee, or groin injuries.
- Neuromyofascial involvement- increased neural tension & posterior thigh pain due to the myofascial trigger points; often associated with decreased flexibility.
- Hip stiffness
- Tightness/Weakness of the hamstrings & quadriceps
- Poor lumbopelvic/core stability.
- History of other lower extremity injury – previous injury to the other lower limb, or injuries to other muscles or tendons in the same lower limb.
- Sciatic nerve pain or irritation.
Extrinsic factors:
- Excessive, repetitive overloads & overtraining.
- Poor training
- Environmental conditions
- Poor equipment
- Insufficient warm-up – A warm-up with isometric contractions increases the strength & length of the muscle. A study found an association between hamstrings injuries & lack of stretch prior to sports participation.
- Fatigue – causes a decline in muscle energy, decreased concentration & coordination, and poor technique.
- Intrinsic & Extrinsic factors contribute to the formation of injury. The tendinopathy usually starts with micro-damage without a remarkable trauma. Normally the tendon is capable of intrinsically repairing itself, meaning that the consequences of this injury are the little. Sometimes, an imbalance can cause further damage and fail to heal. All of this leads to the formation of tendinopathy.
What are the symptoms of proximal hamstring tendinopathy?
- Hamstring tendinopathy causes the gradual onset of pain felt on the outside of the back of the knee. Initially, the pain may be present only after exercise. At this stage, the pain is often ignored as it is relieved with gentle motion or the application of heat. However, if you ignore the problem and continue to exercise, the tendinopathy is likely to worsen and your pain may start to be present for longer periods during exercise until it is present all of the time. Symptoms may include:
- reduced range of movement.
- swelling or inflammation
- stiffness
- Muscle weakness
- Tenderness and swelling over the outside back of the knee.
- Pain is likely to come on gradually. You may have had a ‘niggle’ or restriction that you have put up with for some time.
- You may feel stiffness at the back of your knee, which is often worse in the mornings, or after sitting for long periods.
- Often, when the tendon warms up, the pain eases off, only to return later.
What should I do if I’ve got proximal hamstring tendinopathy?
- If you have proximal hamstring tendinopathy, you should arrange a physiotherapy appointment as soon as possible. Without treatment, it doesn’t generally get better. In the meantime, you can start icing the painful area for 15–20 twinkles every 1–2 hours using a bag of frozen peas or crushed ice wrapped in a damp cloth.
What should I not do if I’ve got proximal hamstring tendinopathy?
- Still, you shouldn’t ignore the problem and continue to exercise if you suspect that you have biceps femoris tendinopathy. Although the pain may ease as you exercise, the exercise itself could be causing further damage. However, you may find that your pain starts to worsen with exercise and your recovery may be prolonged if this occurs.
Could there be any long-term benefits from proximal hamstring tendinopathy?
- Still, proximal hamstring tendinopathy can lead to prolonged pain at the reverse of the knee and a prolonged lay-off from exercise and sport if left undiagnosed and undressed.
How to diagnose proximal hamstring tendinopathy?
- An MRI is required to confirm the diagnosis and to take a look at the severity of the injury. MRI can detect tendon thickening, tearing, inflammation, and swelling at the ischial tuberosity.
- Ultrasound is also used, but this technique is not able to give precise visualization of bone marrow edema. Normally, a high hamstring injury may be combined with stress reaction or bone edema in the ischial tuberosity and findings of the tendon. In the case of tendinopathy, an increased signal is noticeable on the T1-weighted images with no abnormalities on fat-suppressed T2-weighted images.
- A series of provocation tests have been developed in order to help with the diagnosis of this injury.
Assessment tests of Proximal hamstring tendinopathy
Passive Stretch Tests:
- A professional therapist will do a number of assessment tests and take a full case history to understand the injury. In particular,‘resisted knee flexion (trying to bend the knee against resistance) may produce symptoms at the back of the knee. You may also show signs of tight hamstring muscles.
- The bent-knee stretch, the modified bent-knee stretch, and the Puraven-Orava test are used as passive stretch tests in the diagnosis of proximal hamstring tendinopathy. These tests have moderate to high validity, high sensitivity, and specificity for the diagnosis of proximal hamstring tendinopathy.
Bent-knee stretch test:
- The test is performed while the patient is supine. The hip and knee are maximally flexed. Slowly, the therapist will straighten the knee till it is maximally extended; the hip must remain at 90° of flexion. The test is also doable without the assistance of a therapist. The patient can use the rope or a belt to straighten his knee.
Modified bent-knee stretch test:
- The test is performed while the patient is supine lying; the hip and knee are in extension. The therapist takes the heel in one hand and holds the knee with the other hand. He brings the hip and knee into maximal flexion and then rapidly straightens the knee.
- These tests are used to identify a hamstring origin tendinopathy but do not replace an MRI.
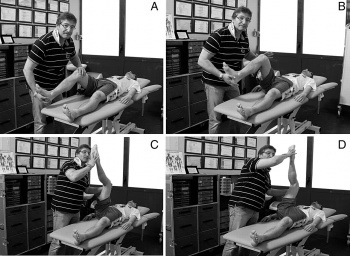
The Puranen-Orava test:
- The Puranen-Orava test is a standing test that actively stretches the hamstring when the hip is flexed to 90°, the knee is extended fully, and the foot is on support at 90° to the standing body.
- Furthermore, the pain response to palpation varies and may have low specificity in the diagnosis of tendinopathies.
Loading Tests
- The reproduction of pain with various loading tests can aid in the diagnosis of proximal hamstring tendinopathy, but the accuracy of these tests still needs to be investigated more extensively. The principle is to reproduce the pain by loading the proximal hamstring tendons. This is done by progressively increasing the compressive and tensile loads and by increasing the angle of hip flexion.
- An example of the load test assessment for patients with proximal hamstring tendinopathy may consist of progression from the single-leg bent knee bridge to the long lever bridge (moderate load) and movements to the single-leg dead-lift (high-load clinical test). The movements are initiated slowly at first, only adding speed if the patient is asymptomatic. The pain score might be increased with the load across all these tests.
Differential Diagnosis of proximal hamstring tendinopathy
- During the examination of the patient, the physiotherapist may have to distinguish between various injuries such as adductor strains, avulsion injury, lumbosacral referred pain syndrome, piriformis syndrome, sacroiliac dysfunction, sciatica, hamstring tendinitis, and ischial bursitis.
- Other sources of posterior thigh pain that could also be confused with hamstring muscle pull should be considered during the examination process. Specific tests and imaging are used to assess and exclude those different pain source possibilities.
- Sciatic nerve mobility limitations can contribute to posterior thigh pain and adverse neural tension could, in some cases, be the only source of pain without any particular muscular injury. In some cases, it is difficult to determine whether it is the hamstrings or other muscle groups like hip adductors (e.g. M. Gracilis and M. Adductor Magnus & Longus) that are injured due to their proximities. Many times, imaging procedures may be required to determine the exact location of the injury.
- Other conditions with similar presentations as hamstring muscle pull are strained popliteus muscle, tendonitis at either origin of the gastrocnemius, sprained posterior cruciate ligament, astrophysicist-pain in ischial tuberosity, lumbar spine disorders, and lesions of the upper tibiofibular joint.
- Biceps femoris tendon avulsion is where the tendon pulls a small piece of bone away with it.
- A hamstring strain is a tear in any of the hamstring muscles.
- Localized constant pain in the buttock and around the ischial tuberosity could be triggered by hamstring origin tendinopathy or ischiogluteal bursitis.
- If the patient complains of pain in the upper gluteal region, there should be a problem with the piriformis muscle.
- Pain occurring over the sacrum or near the sacroiliac joint refers to a pelvic stress fracture or inflammation or malalignment of the sacroiliac joint.
- There are also rare cases where buttock and posterior thigh pain refer to chronic compartment syndrome of the posterior thigh. Due to the resemblance of some symptoms of this injury with other hip injuries, it’s important to get a proper diagnosis; this will likely entail a physical examination and an MRI.
- Sciatic nerve irritation at the piriformis muscle or near the ischial tuberosity
- Ischiofemoral impingement
- The unfused ischial growth plate in the post-adolescent athlete
- Apophysitis or avulsion fracture among adolescents
- Deep gluteal muscle tears
- Stress fracture of the posterior pubic or ischial ramus
- Partial or complete rupture of the proximal hamstring tendon
How to Treat Proximal hamstring Tendinopathy?
- Identify which activity that causing the problem, & stop the activity. Remember that this is an overuse injury, so it’s likely to be the activity done the most regularly.
- Use ice to the site where the pain is located. Apply for 5 to 10 minutes 3 to 5 times per day. The ice will help to reduce inflammation & allow the joint the time it needs to rest & recover after an injury.
- Avoid hamstring stretches. Stretching can separate the muscle fibers, & cause more inflammation. Avoid stretching for at least 2 weeks or until advised by a physical therapist.
- Get physical therapy twice per week or else every day if you are an elite athlete. Massage, ultrasound, LASER & acupuncture can all help stimulate blood flow & encourage healing.
- Don’t sit for extended periods of time. The pressure of sitting can irritate the pain under the buttock, especially on a hard chair. Get up & move regularly.
- Adequate rest is required.
- Use of ice or cold therapy.
- Consultation with the sports injury professional.
- Anti-inflammatory medications can be used for the reduction of pain, swelling & inflammation.
- Ultrasound & laser has been found to be beneficial.
- A comprehensive rehabilitation program with exercises focusing on stretching & strengthening is beneficial.
- Eccentric training is found to be quite helpful for the treatment of tendinopathy.
- Massage therapy is also to be found quite beneficial.
Tips:
- It is quite normal to feel a squeaking or clunking in the knee when you bend it, or squat.
- 3 days after you no longer have pain, start graduall strengthening exercises.
- Tenderness & pain under the buttocks & along the outside of the knee all signal biceps femoris tendinopathy.
- When you experience pain under the buttock while running or sprinting you need to be checked for Proximal hamstring tendinopathy.
Medical treatment:
- Ibuprofen and other non-steroidal anti-inflammatory drugs (NSAIDs) can help relieve pain and reduce swelling in the leg. Some doctors prefer other medicines like acetaminophen.
- Talk with your doctor about what you should take.
- Do strengthening exercises.
- Slowly adding some exercises can help to improve your leg’s strength and flexibility (and, perhaps, prevent the injury from happening again).
- A doctor, athletic trainer, or physical therapist can help determine when your hamstring is ready for these exercises.
- If you have a complete tear of one of your hamstring muscles or tendons, your doctor might want you to have surgery to reattach the tendon to the bone or fix the tendon.
Surgical Treatment
- Surgery is most often performed for tendon avulsion injuries, where the tendon has pulled completely away from the bone.
- Tears from the pelvis (proximal tendon avulsions) are more common than tears from the shinbone (distal tendon avulsions).
- Surgery may also be needed to repair a complete tear within the muscle.
Procedure:
- To repair a tendon avulsion, your surgeon must pull the hamstring muscle back into place and remove any scar tissue.
- Then the tendon is reattached to the bone using large stitches or staples.
- A complete tear within the muscle is sewn back together using stitches.
- Not overdoing things is key when it comes to this type of injury.
- Many people have a hamstring strain come back because they returned to play too quickly.
- So follow your doctor’s advice and don’t push yourself or feel pressure to get back into sports or other activities.
Physiotherapy treatment
Rehabilitation for Proximal hamstring Tendinopathy
Aims of Rehabilitation:
- Reduction of pain & inflammation.
- Stretching of the muscles to regain mobility & flexibility.
- Muscle strengthening.
- Gradual return to the full activity.
Reducing Pain & Inflammation of Proximal hamstring Tendinopathy
- Activities or exercises which have the potential to worsen the injury need to be avoided. The injury can be further aggravated if the affected individual works in a place where has to stand for a long period of time. A sufficient rest period is imperative at least till a stage when the acute injury passes off. The acute stage of the injury is the first 48 hours of the injury. This stage may get prolonged with the use of the injured tendon & inadequate rest. To know if the acute stage of the injury has passed, the patient needs to flex the knee & if there is no pain experienced then it signifies that the acute stage has passed.
Cold therapy: If the injury is recent or acute then rest & apply ice or cold therapy for 10 to 15 minutes every hour for the first 24 to 48 hours.
Knee supports:
- Wear an elastic type of support to help reduce any swelling & support the knee joint.
- Later, once the initial acute stage has passed, or if the injury is a long-term chronic condition then applying heat & wearing a heat retainer type knee support is likely to be more beneficial.
Massage: Cross friction massage techniques are applied to the tendon and are sometimes used. Deep tissue massage to the hamstring muscles themselves helps improve the overall muscle condition.
Soft tissue mobilization:
- Performing soft tissue mobilization via IASTM to gluteals, IT band, Quadriceps, adductors & hamstrings, twice per week for 3 weeks helps in improving the knee extension range of motion among patients suffering from a decrease in flexibility or decreased movement range due to soft tissue limitations.
Electrotherapy
Applying ultrasound or laser treatment can also help with the inflammation & healing process.
Ultrasound Therapy:
- Can be applied after 24 hours, for the first week.
- At the same time, ice treatment should be continued.
- Then, from the second week, alternate heat and cold should be introduced.
- Heat encourages bleeding so it should not be used in the early stages.
- However, at later stages, it will encourage blood flow and healing.
- Heat also helps with muscle relaxation, which in turn can help with pain relief.
- Heat wheat packs are ideal for home use.
The following suggestions will be helpful :
- Completely rehabilitate a hamstring injury before returning to activity.
- Always include a general warm-up, followed by an activity-specific warm-up before training and especially competition.
- Cool down thoroughly after training and competition.
- Include an eccentric strength training program (muscle contraction and lengthening at the same time) for the hamstrings.
- Practice balance, agility, and proprioception drills to improve knee and hip stability.
- Reduce the frequency of, or stop completely, any activities that aggravate the hamstring.
- Rest in between training sessions or competition allows the body to heal minor injuries and repair the muscles to be ready for the next round of activity.
Exercises
- Once pain & swelling have gone, stretching & strengthening exercises can begin to restore the muscle & tendon to full fitness & make it stronger to prevent the injury from recurring.
- Gradually increase the load through the tendon so it can cope with the normal demands of sports.
- Eccentric exercises where the muscle contracts as it lengthens are very beneficial in treating tendinopathies.
- Exercises to strengthen the hip muscles, in particular, the large gluteus maximum muscle may also be beneficial.
In general, the following should apply:
- Resistance training principles should be applied to ensure optimal loading, contraction speed & time under tension
- Monitor pain at the same time on a day-to-day basis with a load test during rehabilitation
- Some pain is allowed during & after exercise (Stable pain – VAS 0 to 3 out of 10)
- Symptoms should settle within 24 hours
- Symptoms should be not progressively worsened over the course of the loading program
- Treat every patient individually & focus on particular phases of rehabilitation or kinetic chain factors specific to the individual
- Progression through the exercise stages might be based on the symptoms & the response when progressing the exercise load & not on specific time frames
- The stage 4 program may take 3 -6 months to complete, but the variation will most likely be present
Stage 1: Isometric hamstring load
- Isometric exercises in the positions without tendon compression are proposed as an effective method of loading the muscle-tendon unit as well as reducing pain in proximal hamstring tendinopathy with irritable symptoms. It has been reported that isometric exercises have a pain inhibitory response. It is recommended that isometric exercises might be repeated several times per day.
- Symptom severity & irritability are used to determine the dosage. The dosage can be adjusted to shorter or less intense contractions or vice versa based on the symptoms. In the early stages of proximal hamstring tendinopathy, the position of the hip might be near neutral hip flexion-extension or in minimal hip flexion (20°- 30° for a straight leg pulldowns). A sign of isometric hamstring loading is an immediate reduction in pain with hamstring loading tests after exercise.
Appropriate exercises for stage I rehabilitation
- Isometric leg curl
- Bridge holds – hip in neutral
- Isometric straight leg pulldowns
- Trunk extensions
- Isometric long leg bridging on two, progressing to one leg holds
Stage 2: Isotonic hamstring load with the minimal hip flexion
Important aspects of proximal hamstring tendinopathy rehabilitation are:
- to restore hamstring strength
- to restore hamstring muscle bulk & capacity in a functional range of motion
- Isotonic hamstring loading may begin when there is minimal or no pain (VAS 0 -3 out of 10) during hamstring loading in the early ranges of hip flexion. Although eccentric exercises are widely accepted as the treatment of choice for tendinopathies, there is not enough evidence for isolating the eccentric component. Heavy slow resistance training adds eccentric & concentric elements. It has also been shown to compare with isolated eccentric loading in tendinopathy rehabilitation.
- With Heavy Slow Resistance, the aim is to perform a slow fatiguing resisted isotonic exercise. Start with 15 RM (the maximum load that can be lifted 15 times in a single set) and progress to 8 RM. Perform 3-4 sets every second or other days Hold contractions for 3 seconds for each phase of the exercise (concentric and eccentric).
- Minimize loaded hip flexion in the early stages. This is advised to preserve the enthesis against too much compression. It is main to concentrate on single-leg work to address asymmetrical strength loss. Continue with the stage 1 isometric exercises on the “off” days. This will help with symptoms (pain), especially if there are still symptoms present.
- Appropriate exercise for stage 2
- Single leg bridge
- prone hip extension
- prone leg curl
- Nordic hamstring exercise
- Bridging progressions
- Supine leg curl
Stage 3: Isotonic exercises in increased hip flexion (70° to 90°)
The aim of rehabilitation in this stage are:
- to continue with the hamstring muscle strengthening in more hip flexion
- to continue with muscle hypertrophy in more hip flexion
- to continue with functional training in more hip flexion
- Once there is minimal pain or no pain (VAS 0 – 3 out of 10) with higher loading hip flexion tests such as lunging & arabesques, isotonic strengthening in increased hip flexion can be implemented. The dosage & frequency of exercises remains the same as in stage 2. The technique is important & exercises might be performed slowly & controlled. The progression into greater hip flexion often causes pain & irritability & is important to monitor the 24-hour response post-exercise with loading tests into hip flexion (hamstring bridge, deadlift, single-leg arabesque).
- Appropriate exercises for stage 3
- slow hip thrusts
- forward step-ups
- walking lunges
- deadlifts
- Romanian deadlifts
- At the end of phase 3, patients with proximal hamstring tendinopathy should be able to load the proximal hamstring comfortably through sport-specific ranges with little aggravation of symptoms.
Stage 4: Energy storage loading
- This stage is only necessary for patients & athletes returning to sports that involve lower limb energy storage or impact loading. The introduction of power or elastic stimulus for the myotendinous unit can start when there is minimal pain during load tests (VAS 0-3out of 10. It is also essential to have adequate bilateral strength in single-leg exercises from stages 2 & 3. Good movement control is also needed. In the early phase of stage 4, it is advised to limit the amount of hip flexion, to preserve the proximal hamstring and the tendon from compression. Note that this is the most provocative stage in the rehabilitation process & a conservative approach is needed for the dosage & frequency of the exercises prescribed. Start with performing exercises only every 3rd day. Follow with a stage 1 day, to settle the tendon. The following day will then include strengthening exercises from stages 2-3. This adds up to a 3- day high, low, & medium tendon load cycle, twice a week, with a rest day between cycles.
- Appropriate exercise for stage 4
- Sprinter leg curl
- A-skips
- Fast sled push or pull
- Alternate leg split squats
- Bounding
- Stair or hill bounding
- Kettlebell swings
- Lateral, rotational cutting movements
Stretching exercise of hamstring muscle

- Hamstring muscle stretch:
- Sit on the ground with both legs out straight.
- Extend the arms & reach forward by bending at the waist as far as possible while keeping the knees straight.
- Hold this position for 15-30 seconds.
- Relax back into the starting position.
- Repeat three times.
Be sure to stretch until a moderate pull is felt in the back of the thighs. If you feel any excessive pain, you might stop the exercise.

2. Hurdler hamstring muscle stretch:
- Sit on the ground with one leg and are out straight.
- Bend the other leg at the knee & position the sole of that foot against the opposite inner thigh.
- Extend the arms & reach forward over the one straight leg by bending at the waist as far as possible.
- Hold this position for 15 seconds.
- Relax and then repeat with the other leg.
3. Standing hamstring muscle stretch( Both legs are together):

- This hamstring stretch is a simple one to do anywhere at all. It is done in the standing position & stretches both legs at once. Here is how you to do the standing hamstring stretch:
- Stand & cross the right foot in front of the left.
- Slowly lower the forehead to the right knee joint by bending at the waist.
- Keep the both knees straight.
- Hold this position for 15-30 seconds.
- Relax and then Repeat for the other side by crossing the left foot in front of the right.

4. Standing hamstring muscle stretch (one leg at a time)
- The one-legged standing hamstring stretch is completely possible the easiest hamstring stretch to do. It can be done anywhere home, office, or outdoors & it requires no special tools.
- Stand up the straight with one heel resting on a small stool. if it is outside, one can use the curb, but be sure to watch for cars.
- Keep the knee straight.
- Reach both arms up toward the place where the wall & ceiling meet. If outside where there is no wall and ceiling, when simply reach up into the air so that the arms are about even with the ears. Reaching the arms up and as opposed to reaching down toward the foot, will keep the back straight.
- Keep the back straight & One should be bending forward slightly from the hips.
- Reach the forward & feel a stretch in the hamstring behind the thigh.
- Hold this position for 15-30 seconds, & repeat 3 times.
5. Runner’s hamstring stretch

- The runner’s stretch is a common flexibility exercise for hamstrings
- Stand one foot from a wall & place the hands on the wall at shoulder height, shoulder-width apart.
- Take a step back with 1 leg while pushing into the wall
- Keep the back straight & press the heels into the floor.
- Hold for 15-30 seconds.
- Step forward and repeat with the other leg.
- Repeat the exercise 3 times on each side.
6. Stretching
- The position of the patient is side-lying & support is provided to the lower leg with hip & knee flexed
- Hold the upper leg & bring it into abduction
- During abduction, try to support the leg against your body, so that the patient can extend the knee whilst pressing the hip into flexion
- With one hand, hold the upper leg & with the thenar of your other hand try to provide stretch to the muscle away from the site of insertion
Quadriceps foam rolling:
- The foam rolling to the quadriceps alone is effective in decreasing the activation of the biceps femoris muscle. Foam rolling on patients’ muscles can lead to alteration in range of motion, performance & muscular co-activation around the particular joint. According to the researcher, when there is a simultaneous contraction of the agonist and antagonist muscle, it helps in providing stability to the knee joint. However, if any disturbance occurs to the stability of the joint, the knee particularly goes for injury.
- Furthermore, the study portrays ACL injury, which is more common due to alteration in muscular co-activation, & further research is required to identify the efficacy of foam rolling on the activation of muscle around the knee joint.
Strengthening exercise of hamstrings muscle:
- Strengthening exercises should be done to gradually & progressively increase the load through the tendon. This is important to prevent injury from recurring. Simply going straight back to normal training levels as soon as are free of pain is not a good idea.
- Strengthening exercises can start as soon as they can be done without pain. This may be after the first 48 hours or it may be up to a week prior to strengthening can begin.
- There might be a gradual progression. Once you can cope with the easy exercises without pain during, after, or the following day, then move on to a more difficult exercise.
Strengthening exercises should continue long after feeling the injury has recovered.
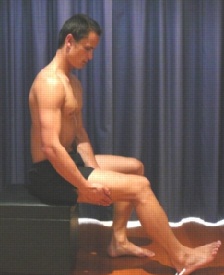
- Static Hamstring contraction
- Start this exercise by sitting with the knee bent to about 45 degrees.
- Press the heel into the ground tightening the back of the thigh.
- Hold for 5 seconds & repeat 10 times as hard as possible pain-free.
2. Bridging exercise

- Start this exercise lying on the back in the supine position.
- Gradually, lift the bottom pushing through the feet, until the knees, hips & shoulders are in a straight line.
- Tighten the back of the thigh while performing this exercise.
- Hold for 3-5 seconds then slowly lower the bottom of the backdown.
- Perform this exercise 3 sets of 10 repetitions provided the exercise is pain-free.
3. Single leg bridging

- Lie flat on the back with the knees bent & feet flat on the floor. The feet & knees might be hip-distance apart.
- Tighten the abdominal muscles slightly to engage the core and stabilize the lower back.
- Lift up into a simple bridge position but as one holds the bridge position, lift 1 foot off the floor & extend the knee as shown.
- Hold for 3-5 seconds, bring the foot back down, & then lower the buttocks to the floor.
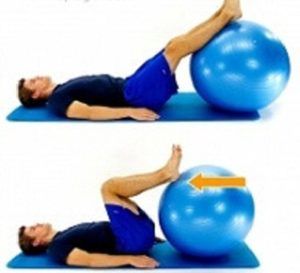
4. Hamstring curls with gym ball:

- Lies on the back with the feet & lower calves resting on a gym ball with knees straight & arms crossed over the chest.
- Slowly curl the ball towards the body by bending the knees & then slowly roll the ball away
- Repeat this exercise 10 times.
5. Pistol Squat (With Optional Plyo)
- Stand holding your arms straight out in front of your body.
- Raise your right leg off the floor in front of you.
- Keeping your right leg straight, push your hips back and lower your body as far as you can without breaking form.
- As you do this, raise your right leg so that it doesn’t touch the floor, and keep your torso as upright as possible. Pause, then push your body back to the starting position.
- Do equal reps for each leg. For a bigger challenge, as you rise out of the squat, add in a jump-off of your planted leg.
6. Split Jumps (With Or Without Dumbbells) :
- Stand in a staggered stance, your right foot in front of your left.
- Lower your body as far as you can.
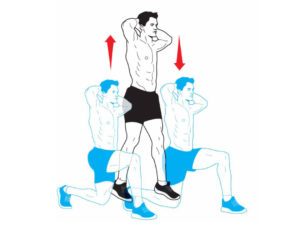
- Quickly switch directions and jump with enough force to propel both feet off the floor.
- While in the air, scissor-kick your legs so you land with the opposite leg forward. Repeat, alternating back and forth with each repetition.
7. Glutes Roll
- Sit on a foam roller with it positioned on the back of your right thigh, just below your glutes.
- Cross your right leg over the front of your left thigh.
- Put your hands flat on the floor for support.
- Roll your body forward until the roller reaches your lower back.
- Then roll back and forth. Repeat with the roller under your left thigh.
Hamstring kt tape:
- Kinesiology taping can be applied during the later stages of rehabilitation by encouraging activation of the muscle fibers.
- Lack of use, particularly if splinting, results in muscle shrinkage and the formation of scar tissue where the tear is healing.
- Excessive scar tissue prevents healthy muscle function, as it doesn’t stretch and move as normal muscle does.
- To avoid these complications rehabilitation exercises need to begin early (except for grade III injuries):
- After a few days, once the pain has subsided, you should start to do regular gentle biceps femoris stretches followed by a programmer of gentle exercises, such as walking and cycling.
- Always warm-up before exercising and cool down afterward.
- Stop if the pain returns.
- To avoid injuring yourself again, you should only return to a full level of activity when your hamstring muscles are strong enough.
Your physiotherapist or a sports therapist will be able to advise you on returning to your sport and on a suitable graded exercise program, which might include:
- Starting with declining treadmill running.
- Moving to steep decline treadmill running.
- Doing hamstring strengthening exercises using a pulley system to reduce the load.
- Doing regular hamstring exercises.
- When strength has returned, a gradual return to the desired sport can be attempted.
- Running should be re-introduced gradually.
- Full return is usually possible only after maximal flexibility and strength have been obtained.
- Re-injury is extremely common. Athletes are highly motivated and are likely to have set personal goals for training, timing, and performance. However, re-injury not only prolongs recovery, it also increases the risk of permanent damage.
How to Prevent Hamstring tendon injury?
- Always ensure you follow a correct warm-up prior to rain or competition.
- Stretch the hamstring muscles both before & after training. Stretch every day, regardless of whether you are training or not.
- Strengthen the muscles to cope with the demands placed on them. In particular eccentric strengthening is important.
- Have regular sports massage to keep the muscles & tendons in good condition.
- Avoid doing too many accelerating/decelerating runs or hill work.





