Patella Alta
Table of Contents
Introduction
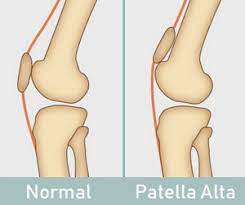
Patella Alta, also known as high riding patella, is a condition in which the kneecap rides higher on the thigh bone than usual.
The knee becomes less stable as a result, making it more prone to dislocation and anterior knee pain.
The majority of the time, patella alta is a congenital condition, but it can also arise as a result of a knee injury, such as a ruptured patellar tendon.
Here, we examine what patella alta is, why it’s problematic, common causes and symptoms, how it’s diagnosed, and various patella alta treatment options.
What Is Patella Alta?
The patella bone, also known as the kneecap, is a tiny, triangular bone that sits in front of the knee and is inverted (or upside down).
The patellofemoral joint, which is formed by the kneecap resting in a dip on the front of the femur bone, the lower thigh bone, is encircled by the quadriceps tendon. The patellofemoral groove, also called the patella groove, trochlear groove, or intercondylar groove, is the name of this dip. The patella slides up and down this groove as the knee moves.
The patellar tendon emerges from the base of the kneecap, connecting it to the tibia, the shin bone.
The kneecap sits higher than usual in the patella groove in the patella alta. There is only a very slight barrier on either side of the kneecap because the groove is much shallower here than it is further down.
As a result, the groove offers the kneecap very little sideways support.
Why Is Patella Alta A Problem?
The patella typically moves up and down the middle of the patellofemoral groove when the knee is bent and straightened. Because the groove’s nice depth restricts the kneecap’s sideways movement, the patella is kept firmly in place.
However, there is less sideways stability in the patella alta because the kneecap is positioned higher than usual in the shallower part of the groove.
As a result, the patella runs the risk of being partially or completely dislocated as it is pulled sideways over the low edge of the groove during knee flexion.
Patella alta is thought to be the cause of about 30% of recurrent patella dislocation cases.
Patellofemoral pain, also known as anterior knee pain, and chondromalacia are both conditions that can result from the patella dislocating or subluxing (partially dislocating).
Patella Alta also increases the chance of knee arthritis and fat pad or infrapatellar bursitis inflammation.
Clinically Relevant Anatomy
The patella, a flat, triangular bone with one corner inverted, is located in front of the knee joint. The area of the knee joint between the patella and the femoral condyles is known as the patellofemoral joint. The function of the, connected to the patella with a shared tendon, completely depends on the patellofemoral articulation.
The rectus femoris (RF), the vastus lateralis (VL), the vastus intermedius (VI), and the vastus medial (VM) are the four muscles that make up the quadriceps femoris, all of which insert on the patella. The patellar tendon, which joins the patella’s base to the tibia, is another tendon. The quadriceps muscle group can straighten the leg thanks to the strength of this tendon. Articular cartilage, an incredibly tough, smooth substance intended to lessen friction forces, covers these three bones. The intercondylar groove on the femur is where the patella is located.
What Causes Patella Alta?
A high-riding patella is referred to as patella alta, which is an idiopathic condition, meaning that the cause is frequently unknown. The following are typical patella alta causes:
Patella alta is typically a congenital defect present from birth and likely resulting from embryonic development.
Long Patellar Tendon: Patella alta is typical in people with abnormally long patellar tendons, >52mm.
Patella Alta may appear following a knee injury, usually a dislocated kneecap.
Patella alta is mostly found with cerebral palsy and diplegia-related conditions in which in kids who walk with bent knees.
Patella Alta Symptoms
Typical symptoms of patella alta include:
People with patella alta frequently express discomfort or instability in their knees, especially when moving or running.
Recurrent Kneecap Dislocation: People with a high-riding patella frequently experience knee dislocation. Some people have the ability to willfully move their kneecap in and out of the patellar groove, causing it to dislocate and then realign.
Patellofemoral pain syndrome, also known as anterior knee pain, is a common symptom of patella alta and is exacerbated by activities such as squatting, prolonged sitting, and climbing stairs.
How Is Patella Alta Diagnosed?
Your doctor will first examine your knee in order to determine if you have patella alta. They will examine the relationship between the kneecap and femur from various perspectives and with the knee in various positions.
There are numerous illnesses that are known to be connected to patella alta, including:
- Patellofemoral instability
- Recurrent patellofemoral dislocation
- Neuromuscular diseases (poliomyelitis)
- Spastic cerebral palsy
- Osgood Schlatter disease
- Sinding Larsen Johanssen disease
- Patella tendon-lateral femoral condyle friction syndrome
- Chondromalacia patella
Diagnostic Procedures
Most often, measurements based on imaging are used to define patella alta; descriptions are used only rarely. Imaging consists of patellar tendon length, sagittal MRI, radiographic ratios measured on MRI, and lateral radiographs. For ISI and CDI, the cutoff values for patella alta ranged from > 1.2 to > 1.5. The cutoff values for both indices were comparable to those for traditional radiographs, but they were rarely used on MRI. The patellotrochlear index was frequently used on sagittal MRI; the cutoff values ranged from 0.125 to 0.28. There was an increase in patellar tendon length (from > 52 mm to > 56 mm) according to eleven studies.
Outcome Measures
There are several ways to find out if patella alta is present. The method of measuring patella height using the ratio of the patella tendon’s length to the patella’s diagonal length on lateral radiographs was first described by Insall-Salvati. Since then, numerous methods have been developed in an effort to categorize patella position, including those by Blackburne and Peel, Caton et al., and de Carvalho et al. The patella has a normal range of 0,8 to 1,2. When the ratio is higher, patella alta occurs.
The presence of patella alta can also be detected using the Blackburne-Peel index. This method involves taking a lateral radiograph of the knee with 30° of flexion. To determine whether there is a patella alta, the lengths of three surfaces must be measured. The first length is a vertical line that runs from the tibial plateau’s horizontal line to the top of the inferior aspect of the patella articular surface. The superior patella articular surface is the second length, which is vertical. The posterior aspect of the patella articular surface is where both vertical lines are measured. A horizontal line on the tibial plateau represents the third length.
Because it requires measurements across various sections, this technique is difficult to use with an MRI. A patella ratio of 0,5 to 1,0 is considered normal. Patella alta occurs when the ratio is greater than 1.
The most popular radiographic technique for measuring patellar height is the Caton-Deschamps index. On a radiograph of the knee taken from the side, it is measured at 30 degrees of flexion. On an MRI, this technique is simple to measure. to measure the patella’s height. We measure the distance between the anterior lip of the tibial plateau and the inferior articular surface. A patella ratio of 0,6 to 1,3 is considered normal. There is a patella alta when the ratio is greater than 1,3.
Examination
Physical Examination
Tests:
Full Knee Extension: The kneecap can move slightly from side to side when the knee is completely straight and relaxed. Your doctor will suspect patella alta if it moves farther than usual.
Knee Slightly Bent: Patella alta frequently exhibits the “camelback sign” when the knee is flexed at about 30 degrees. Two humps, resembling two humps on a camel, can be seen when viewed from the side. One is caused by the high-riding patella pointing upwards, and the other is caused by an enlarged infrapatellar fat pad or infrapatellar bursa.
Knee Bent: When the patella alta is present, the kneecaps point upward rather than forward and may be externally tilted, rotated, or twisted round to the outer side of the knee when the knee is at a right angle of 90 degrees. Positive “grasshopper eyes sign” is what this is.
Fairbanks patellar apprehension test:
When there is pain and a defensive muscle contraction caused by lateral patellar dislocation with 20° to 30° of knee flexion, the test is positive. The positive test results suggest that the patient’s problem includes lateral patellar instability as a significant component. This may be so effective that the patient grabs the therapist’s arm or pulls the leg back when the therapist reaches for the knee with his hand to avoid making contact.
94.1% overall accuracy, 88.4% specificity, and 100% sensitivity.
Patellar glide test:
The instability is assessed using this test. Ineffective lateral/medial restraints are consistent with a medial/lateral displacement of the patella with this test that is greater than or equal to 3 quadrants. More often than medial instability, lateral patellar instability occurs.
Imaging For Patella Alta
The most common methods for conclusively diagnosing patella alta are X-rays and MRIs. The knee should be flexed 30 degrees in a lateral view from the side. Patella alta can be diagnosed using a variety of techniques. Each one requires taking various knee measurements and calculating their ratios:
Insall-Salvati Ratio: Patella alta is indicated by an A/B ratio greater than 1.2.
A: patellar tendon length, measured from the insertion point on the tibial tuberosity to the bottom of the kneecap.
B: Greatest pole-to-pole measurement of patellar length
Modified Insall-Salvati Ratio: The length of the patella’s articular surface (the back) is used to measure the patellar length in a slightly different way. Here, an A/B ratio of 1.25 is considered normal; a ratio of more than 2 indicates patella alta.
If A/B is greater than 1.3, the Caton-Deschamps Index indicates that the patient has patella alta.
A: The distance from the front tip of the tibial plateau to the lower pole of the patella.
B: Articular surface length and patella length
Blackburn-Peel Ratio: A diagnosis of patella alta is thought to be confirmed if the B/A ratio is greater than 1.
A: Patella length = articular surface length
B: Draw a horizontal line parallel to the tibial plateau and measure from the line to the inferior aspect of the articular surface, which is the bottom of the back of the kneecap.
Medical Treatment
Patients with patella alta may undergo tibial tuberosity osteotomy. With this procedure, the patellar ligament’s attachment is moved from the kneecap to the tibia. The patella moves downward because it is connected to this ligament as well. Patella alta can cause the quadriceps angle to increase; this can be fixed by moving the patellar ligament’s bony attachment inward.
Following the procedure, a few things like infection, knee joint stiffness, nerve damage, and recurring instability are possible. After the procedure, the patient must walk with crutches. Physical therapy and exercise should be done after surgery to reduce pain and swelling because this will impair the knee’s range of motion. Physical therapy will also improve your muscle control. Three to six months should pass while you recover.
How Do You Treat Patella Alta?
The goal of treating patella alta is to lessen knee pain and instability while regaining complete knee function.
For a high-riding patella, non-operative treatment options include:
Rest: to allow any inflammation to subside, refrain from provoking activities.
Strengthening Exercises:
With a high-riding patella, strengthening the knee, kneecap, and buttock muscles can help to correct the patella position, which will lessen pain and enhance knee stability. Exercises are a good way to treat knee pain and stop it from returning.
The quad muscles are maintained and strengthened with the help of quad crunches, which also make it possible for the knee to be fully straightened. Straight leg and/or knee, By bringing your knee all the way down, tighten the muscle in the front of your thigh. Your thigh muscles ought to clench. 3-second hold. Every 3 to 4 hours, repeat 10 to 20 times. If you are having trouble getting your knee to fully straighten, lift your leg a little bit off the bed by placing a towel rolled up underneath the ankle. Then perform the exercise as directed. Gravity can help the knee straighten by lifting it slightly.
Short Arcs: This exercise helps to increase control and strengthen the quadriceps muscles without requiring much knee movement. Sit upright with your leg extended on a flat surface, such as a bed, or lie flat on your back. Put a rolled-up towel with a diameter of approximately 10 cm under the knee and/or Cinch your thigh muscles as you bring your toes closer to you. Keep your knee resting on the towel as you gradually raise your foot off the bed until it is straight. Hold for three to five seconds before lowering slowly. Repeat ten to twenty times. adding weight, such as by donning a shoe or using a light ankle weight, and advancing further by doing so, you can challenge yourself further.
Straight Leg Raise (SLR): Lie on your back with your legs relaxed on the floor and your hips straight. Your unaffected leg should be bent at the knee to a 90-degree angle, with the foot flat on the ground. By tensing your quadriceps (the group of muscles on the front of your thigh), you can stabilize the muscles on your straight leg. Lift the straight leg six inches off the ground after taking a slow, deep breath. Take a three-second hold. Slowly exhale as you steadily lower the leg to the ground. Unwind and repeat ten more times. When performed correctly, the movement will cause tension in your hip, thigh, and abdomen.
The Clamshell: Stack your feet and hips while lying on your side. Your knees should be 90 degrees bent, and then place your head on your right arm. until your feet are parallel to your butt, draw your knees in towards your body. To prevent your other hip from sagging back, place a hand on it. Your starting point is here. Raise one knee as high as you can without rotating your hip or lifting your other knee off the floor while keeping your abs tight and your feet together. Slowly lower one knee to the starting position while holding for one second and contracting your glutes at the top of the move. 20 repetitions in total, then repeat on the opposite side.
Leg Standing, Hamstring Clenches, The Bridge, Long Arcs, Knee Marching, Kick Backs, Heel Raises, and Buttock Kicks are some additional exercises.
Exercises for strengthening the knee help to increase the most crucial aspects of knee strength and control:
To control and stabilize the knee
To guarantee proper foot, knee, hip, and back biomechanics
To lessen the possibility of harm
To permit complete pain-free movement
To ensure proper operation
Physical Therapy:
The resting position of the kneecap may be improved with manual therapy. Manual gliding is used to alter the patella’s resting height prior to knee extension, theoretically reducing knee pain. Patellar alignment can be corrected by using tape to correct the patella’s positional issue. Patients reported that walking was not too difficult for them, that their average pain level was a VAS score of 12, and that they were using fewer painkillers.
Ice Packs: Regularly applying ice packs could also help with symptoms of patella alta Inflammation, swelling, and pain can be reduced with knee ice wraps. Injuries or long-term knee conditions may also benefit from their assistance. They can be anything from single-use disposable packs to ice packs with specialized designs and knee brace inserts with higher-quality cryotherapy. You can compare models, read reviews, or choose the best ice wrap for you from the five types that are covered here:
Knee Brace: Using a brace while wearing a brace may help to lessen the signs and symptoms of a high-riding patella. The brace should ideally have a tubular portion that sits above the kneecap to prevent it from riding up. Different support levels and fixing techniques are offered by knee braces. Additionally, they come in a variety of materials and have a wide range of prices. Bracing has been found to be effective in treating patients with patellofemoral dysfunction and anterior knee pain by decreasing pain and expanding the patellofemoral contact area. Although Shellock, et al. (1994) showed that the brace was ineffective when patella Alta was present during a study to evaluate the effectiveness of a brace developed to prevent medial and lateral patellar subluxation. Four of the five knees in this study’s group that did not improve had patella, Alta. The brace used in this study may not have been the best brace design for people with patella Alta because it only stabilized the medial and lateral patellar glide.
Patellar Taping: The patella’s position could also be adjusted with the aid of taping. Taping is frequently used as a temporary or supplemental technique. The tape is commonly used by physiotherapists to: decrease injury recurrence, improve joint stability, boost athlete confidence, inhibit muscle action, facilitate muscle action, lessen the strain on injured or vulnerable tissues, improve proprioception, compress in the presence of edema, and promote lymphatic drainage.
Operative Treatment
Surgery is required to effectively treat severe cases of patella alta where the kneecap keeps dislocating or when conservative treatment fails. There are several different surgical procedures for patella alta, including:
Knee tuberosity Tibial tubercle transfer is also known as osteotomy.
At this point, the patella is moved downward along with the attachment of the patellar tendon. The patellar tendon attachment can be shifted inward, if necessary, to correct the Q angle.
In a tibial tuberosity osteotomy, the tibial tuberosity is removed from the front of the shin bone, moved downward, and then fixed in place with a screw and wires.
Lateral Release: If the structures on the outside of the knee are too tight and are causing the patella to ride high, lateral release surgery can be done to loosen them. Learn more about the procedure in the lateral release section.
The patella is completely removed during a patellectomy, which is only recommended when all other surgical options have failed or when there is severe patellofemoral arthritis.
Recovering From Surgery
Following patella alta surgery, you will:
Wear A Knee Brace: Following surgery, a hinged knee brace is typically worn for up to six weeks. In order to facilitate proper knee healing, the brace will restrict knee flexion.
Use crutches: For the first few weeks, you should only bear a small amount of weight on the operated leg, necessitating the use of crutches. Over the following few weeks, you will be able to gradually increase the weight through the leg. By six weeks, the majority of patients are free of crutches. See our best advice for using crutches on stairs.
Physical Therapy: As soon as your knee can be moved, you’ll begin physical therapy to help it regain its full strength, stability, range of motion, and functionality. Around three months after birth, you can begin low-impact exercises like lunges and work your way up to light jogging.
After a patella alta surgery, it typically takes six months to recover and resume high-impact activities and sports fully.





One Comment