Musculocutaneous Nerve
Table of Contents
What is a Musculocutaneous Nerve?
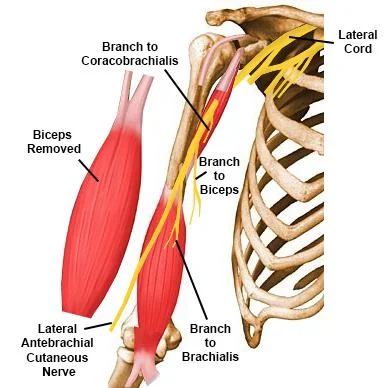
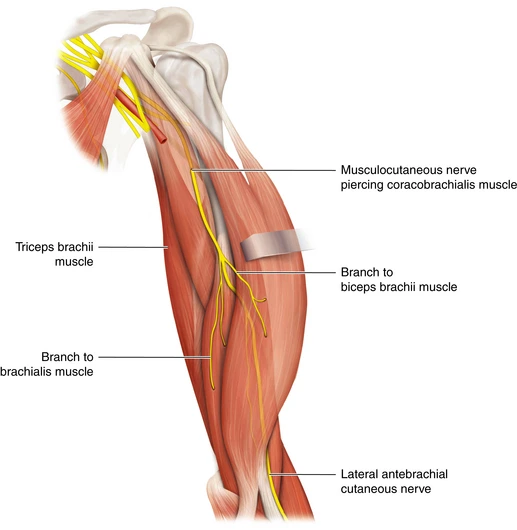
The brachial plexus is the complex set of nerves originating from the ventral roots of C5-T1 that innervates numerous muscles and cutaneous regions of the upper limb, thorax, and back. The 5 spinal roots form a superior, middle, and inferior trunk. Each of those trunks has an anterior and posterior division, which then continues into a medial, posterior, and lateral cord. Along the course of the brachial plexus, 18 nerves rise, involving five terminal branches. The musculocutaneous nerve (roots C5-7) may be a terminal branch of the lateral cord. The musculocutaneous nerve may be a major peripheral nerve of the upper limb.
The Musculocutaneous nerve may be a large branch of the plexus brachialis. It is called the musculocutaneous nerve because it supplies the muscles of the front of the arm and the skin of the lateral side of the forearm. The Musculocutaneous nerve could be a terminal branch of the lateral cord of the nerve plexus. It emerges at the inferior border of the pectoralis muscle. It passes lateral to the axillary and upper part of arteria brachialis. It leaves the axilla to then pierce the Coracobrachialis near its humeral insertion to consist of the intermuscular septum between the biceps humeri and brachialis muscles. Then it enters the elbow by piercing deep fascia and terminates because of the Lateral Cutaneous nerve of the forearm.
Origin
The musculocutaneous nerve originates from the lateral cord of the nerve plexus (C5-C7) at the inferior border of the pectoral muscle. The brachial plexus itself originates from the anterior rami of the spinal nerves C5-T1. The roots emerge between the anterior and middle scalene muscles, and coalesce and mingle to make an upper, middle and lower trunk, which eventually produce a medial, lateral, and posterior cord (all associated closely with and surrounding the axillary artery).
The cords are named in keeping with their relationship with the artery. Locating the nerve whilst dissecting is just a case of identifying coracobrachialis, and looking out for the nerve entering it.
Motor branches
Brachialis (supply from Radial nerve)
Coracobrachialis
Biceps Brachii(both long head and short head)
Sensory branches
lateral cutaneous nerve to the lateral forearm
Articular branches
Elbow joint and Humerus
Movements Produced
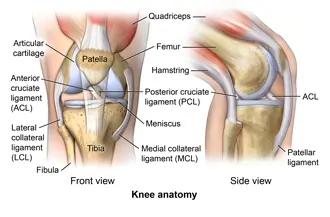
Brachialis– flexion of the ginglymus.
Coracobrachialis – flexes and adducts the glenohumeral (GH) joint and acts to stabilize the humeral head within the glenoid fossa when the arm is hanging freely by side.
Biceps Brachii- a weak abductor of GH joint when arm externally rotated, weak flexor of GH joint which helps to balance GH joint when weight brought in the arm, supinator, and flexor of the articulatio cubiti.
Structure and Functions
The musculocutaneous nerve innervates the three muscles of the anterior compartment of the arm: the coracobrachialis, musculus biceps brachii, and brachialis. it’s also liable for cutaneous stimulation of the lateral forearm. Before further discussing the particular functions of the muscles it innervates, an outline of the nerve’s general anatomy and course through the arm is helpful.
Gross Anatomy and Course
The musculocutaneous nerve may be the leading recognizable nerve of the brachial plexus. When viewing the axilla, the musculocutaneous nerve may be seen branching from the lateral cord and piercing directly into the deep surface of the coracobrachialis muscle. The nerve enters the coracobrachialis on average 5.6 cm from the muscle’s origination on the coracoid process of the scapula. It then is seen exiting the anterior surface of the coracobrachialis to continue coursing inferiorly within the anterior compartment. Throughout this portion of the arm, the nerve is found deep to the biceps humeri and superficial to the brachialis, and it gives off motor branches to those muscles along the way.
Using the acromion process because of the origin, the nerve branch points for the musculus biceps brachii and brachialis were found to occur at a median distance of 13.0 cm and 17.5 cm as well as the course of the musculocutaneous nerve, individually. Having given off all of its motor fibers, the trunk continues inferiorly. some cm superior to the cubital joint, the musculocutaneous nerve then leaves the space between the biceps and brachialis muscles just lateral to the biceps brachii tendon and is at this time considered the lateral antebrachial cutaneous nerve. The lateral antebrachial cutaneous nerve pierces the deep fascia superficially to realize access to the subcutaneous compartment.
This terminal cutaneous branch of the musculocutaneous nerve gives off a volar and dorsal branch to provide the skin of the lateral forearm. Cutaneous innervation of the medial forearm is supplied by the medial antebrachial cutaneous nerve (roots C8-T1), an instantaneous branch of the medial cord. The posterior forearm receives cutaneous innervation from the posterior antebrachial cutaneous nerve (roots C7-C8), a branch of the nerve.
Motor Functions
The musculocutaneous nerve innervates the muscles within the anterior compartment of the arm:
- Biceps brachii
- Brachialis
- Coracobrachialis
These muscles flex the shoulder and the elbow from the upper arm. additionally, the biceps humeri also supinate the forearm. A useful mnemonic to assist you to remember these muscles is BBC.
Sensory Functions
The musculocutaneous nerve provides arise to the lateral cutaneous nerve of the forearm.
This nerve initially enters the deep forearm, then again pierces the deep fascia to become subcutaneous. during this region, it will be found near the venous blood vessel. The lateral cutaneous nerve of the forearm stimulates the skin of the anterolateral aspect of the forearm.
Variations
The musculocutaneous nerve shows usual variations and connections with the median nerve.
It may adhere for a few distances to the median so pass outward, beneath the biceps, rather than through the coracobrachialis.
Some of the fibers of the median may last a long way within the musculocutaneous and then leave it to hitch their proper trunk; less frequently the reverse is the case, and the median sends a branch to difficulty the musculocutaneous.
The nerve may pass under the coracobrachialis or through the musculus biceps brachii.
Occasionally it gives a filament to the pronator teres, and it supplies the dorsal surface of the thumb when the superficial branch of the musculospiral nerve is absent.
Blood Supply and Lymphatics
Arterial Supply
The musculocutaneous nerve parallels the arteria axillaris proximally within the arm, but because the nerve passes into the coracobrachialis it then takes the unique course described above that doesn’t parallel any specific artery. Nevertheless, the blood supply to the arm is managed primarily by the continuation of the arterial blood vessel, which is termed the arteria brachialis once it passes the lower margin of the teres major muscle. The arterial blood vessel and its branches- the deep brachial, radial, and ulnar arteries- supply the muscles of the arm’s anterior compartment additionally to all or any of the opposite structures within the arm, forearm, and hand.
Venous Drainage
Venous drainage within the arm is primarily handled by the venous blood vessel and its tributaries laterally, and therefore the vena basilica and its tributaries medially. These two veins together with the vena brachialis deep within the arm all drain into the vena axillaris, which carries blood back towards the proper atrium. The vein closely parallels the lateral antebrachial cutaneous nerve distal to the nerve’s passage on the lateral side of the biceps humeri tendon.
Muscles
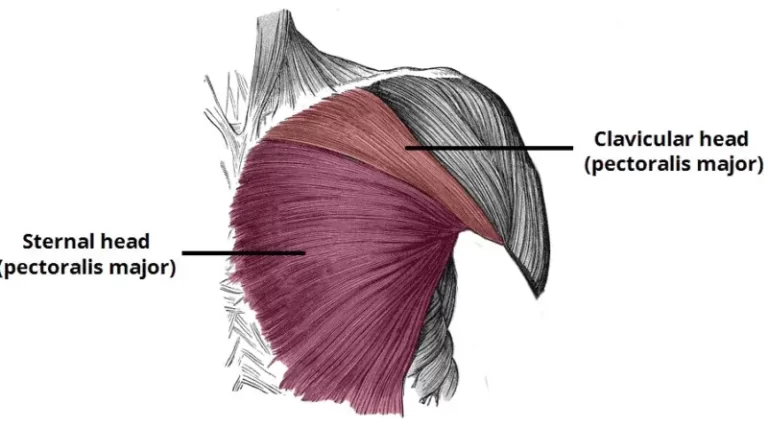
The musculocutaneous nerve stimulates the three muscles of the arm anterior compartment. The coracobrachialis, the primary muscle to receive innervation, originates in the coracoid process and inserts on the center third of the medial aspect of the humerus. It flexes and adducts the shoulder at the glenohumeral joint and it’s significant to observe that different the opposite two muscles of the anterior compartment, the coracobrachialis doesn’t cross the elbow and thus has no action on the elbow.
The musculus biceps brachii muscle incorporates a short and long head. The short head arises on the coracoid process of the scapula, while the long head arises on the supraglenoid tubercle of the scapula. These two heads are close to making one tendon that inserts on the radial tuberosity and therefore the fascia of the forearm via the bicipital aponeurosis. The muscle biceps brachii works to flex the elbow, additionally supinating the forearm. The biceps muscle accepts its innervation from the C5 and C6 fibers of the musculocutaneous nerve.
The brachialis muscle originates on the distal portion of the anterior humerus, and inserts on both the processus coronoideus and tuberosity of the ulna. Many will think about the musculus biceps brachii when thinking of elbow flexion, but it’s actually the brachialis that’s considered the most flexor of the elbow. The brachialis may be a versatile flexor therein it’s ready to flex the elbow from either a pronated or supinated forearm position.
Surgical Considerations
Surgeons always remain astute to the peripheral nerve anatomy because of the relative susceptibility that several nerves have to intraoperative damage. Zlotolow, et al describe the various surgical exposures of the humerus and also the specific nerves that will be injured with each approach. The deltopectoral approach, specifically for repairs of subscapularis tears, places the musculocutaneous nerve in danger. Anterolateral approaches for the reduction of humeral fractures place the lateral antebrachial cutaneous nerve in danger. Additionally, it’s noted that surgeons should avoid dissecting medial to the conjoined tendon (short head of the biceps and coracobrachialis attachment on the coracoid process) because of the danger of lesioning the musculocutaneous nerve.
Pathology/Injury
Isolated injuries of the Musculocutaneous Nerve are rare. it’s going to become injured by:
- Brachial Plexus damage
- Compression injury eg weight lifting or sports involving many forearm flexing and supination.The biceps aponeurosis and tendon compress against the fascia of the brachialis muscle causing sensory loss below the elbow on the lateral side of the forearm.
- Dislocation of the shoulder
- Shoulder surgery
- Entrapment of the nerve at the elbow
Clinical Significance
Musculocutaneous Nerve Palsy
As with all nerves, direct trauma to the musculocutaneous nerve within the type of lacerations, gunshot wounds, and nearby bone fractures has been reported. While isolated musculocutaneous nerve syndromes are relatively uncommon, some specific clinical situations are described within the literature. most vital is entrapment of the musculocutaneous nerve within the coracobrachialis muscle, resulting in biceps humeri and brachialis weakness and atrophy with accompanying loss of sensation within the lateral forearm.
It’s been found that patients most apt to develop this condition are active young individuals that regularly engage in shoulder flexion and elbow flexion with the forearm during a pronated position. This syndrome often occurs secondary to hypertrophy of the coracobrachialis and thus may be a result of chronic overuse. it’s important to notice that the compressed nerve within the coracobrachialis has already given off its motor branch to the coracobrachialis, and thus won’t present with defects of coracobrachialis muscle function.
Another important clinical scenario could be a shoulder dislocation. While the foremost frequently injured nerve during this scenario is the axillary nerve, several cases of musculocutaneous nerve damage are reported secondary to anterior humeral dislocations. The musculocutaneous nerve branches from the lateral cord just anterior to the glenohumeral joint, explaining its susceptibility to break with anterior dislocations. Additionally, it’s been found that downward traction and external rotation place significant tension on the nerve, and anterior humeral dislocations may place the nerve during this position.
The musculocutaneous nerve is well secure within the axilla and injury is relatively uncommon. Characteristic mechanisms of injury include penetrating injury to the axilla e.g. stabbing, and induced injury resulting from heavy retraction while the deltopectoral approach to the shoulder.
Motor functions – coracobrachialis, musculus biceps brachii, and brachialis muscles are affected:
Flexion at the shoulder and elbow are weakened but can still be carried out by the pecs and brachioradialis individually.
Sensory functions – over the lateral side of the forearm loss of sensation.
Lateral Antebrachial Cutaneous Nerve Palsy
In the musculocutaneous nerve lesions described, specific damage to the lateral antebrachial cutaneous nerve has also been investigated. While this sensory-only lesion often goes unnoticed clinically, there are some clinical situations worth noting. Just before leaving the deep fascia to give cutaneous innervation, the lateral antebrachial cutaneous nerve passes between what has been described as a tunnel created by difficult fascial layers of the brachialis and bicipital aponeurosis. The nerve may be compacted by the bicipital aponeurosis in cases of chronic elbow extension with the forearm while in a pronated position. this could result in hypesthesia within the lateral forearm region.
The lateral antebrachial cutaneous nerve travels in close proximity to the vein, thus in danger of injury during venipuncture procedures. General practice is to avoid the medial aspect of the cubital fossa during venipuncture because of cases of median antebrachial cutaneous nerve damage. However, cases of lateral antebrachial cutaneous nerve damage like that described by Rayegani and Azadi suggest that caution should be taken when using the lateral aspect of the cubital fossa similarly. Using as superficial an approach as possible has been suggested to scale back the risk of peripheral nerve damage.
Nerve injuries
Injury to the musculocutaneous nerve is led by three mechanisms: repeated microtrauma, indirect trauma, or direct trauma on the nerve. overdo of coracobrachialis, biceps, and brachialis muscles can lead to the stretching or constriction of the musculocutaneous nerve. people who have it can complain of pain, tingling, or reduced sensation over the lateral side of the forearm. These symptoms are frequently replicated by pressing over the region to lower the coracoid process (positive Tinel’s sign). Pain may be replicated by flexing the arm against resistance. Other differential diagnoses which will mimic the symptoms of musculocutaneous palsy are C6 radiculopathy (pain will be produced by the movement of the neck), long head of biceps tendinopathy (no motor or sensory deficiencies), and pain of the bicipital groove. Electromyography test displays slight neural damage at the biceps and also the brachialis muscles with slower motor and sensory convection over the Erb’s point.
Clinical Consequences
This is the most common reason for musculocutaneous nerve injury. The nerve is well protected within the axilla and also by musculature within the arm.
Imagine for a second that the musculocutaneous nerve has been severed at its roots, in order that it’s now not innervating the structures it normally does, i.e. the elbow flexors. The solution surprisingly is yes, but it’ll be weakened. this can be due to a muscle called brachioradialis that originates from the lateral epicondylar eminence and epicondyle and inserts onto the radial process.
This muscle incorporates a number of functions including supination, wrist abduction, and wrist extension, but also some elbow flexion. it’s innervated by the nervous, so isn’t plagued by musculocutaneous nerve injury.
Supination and flexion at the cotyloid joint are additionally weakened but not lost thanks to the role of the supinator and greater pectoral muscle respectively. Sensation to the lateral part of the forearm would even be affected.
FAQ
What happens if the musculocutaneous nerve is damaged?
Isolated injury to the musculocutaneous nerve could be a rare occurrence. Associated signs and symptoms of an isolated musculocutaneous neuropathy may include weakness in elbow flexion or shoulder flexion, atrophy of the musculus {biceps brachii|biceps humeri|biceps}|biceps humeri|biceps}, and pain or paresthesia at the lateral forearm.
What does the musculocutaneous nerve branch into?
Its terminal branch, the lateral cutaneous nerve of the forearm, supplies the feeling of the lateral side of the forearm from the elbow to the wrist. Besides, the musculocutaneous nerve also gives articular branches to the cubitus and to the humerus.
Where is the musculocutaneous nerve most vulnerable?
axilla
Injury is additionally not common because the nerve incorporates a protected location and course, deep within the arm. it’s vulnerable within the axilla, which is the most typical site of isolated injury.What is the most function of the musculocutaneous nerve?
The musculocutaneous nerve innervates the three muscles of the anterior division of the arm: the coracobrachialis, biceps brachii, and brachialis. it’s also responsible for cutaneous innervation of the lateral side of the forearm.
Which skin area will lose sensation if the musculocutaneous nerve is cut?
Damage to the shoulder and plexus brachialis can affect the musculocutaneous nerve. Constriction of the nerve by the biceps aponeurosis and tendon as opposed to the fascia of the brachialis muscle leads to sensory loss below the elbow on the lateral side of the forearm. Entrapment of the nerve is one reason for pain at the elbow.
What does the musculocutaneous nerve supply?
The musculocutaneous nerve stimulates the three muscles of the anterior compartment of the arm: the coracobrachialis, biceps brachii, and brachialis. It’s also responsible for cutaneous stimulation of the lateral forearm.



4 Comments