Metacarpophalangeal (MP or MCP) Joint
Table of Contents
What is Metacarpophalangeal (MP or MCP) Joint?
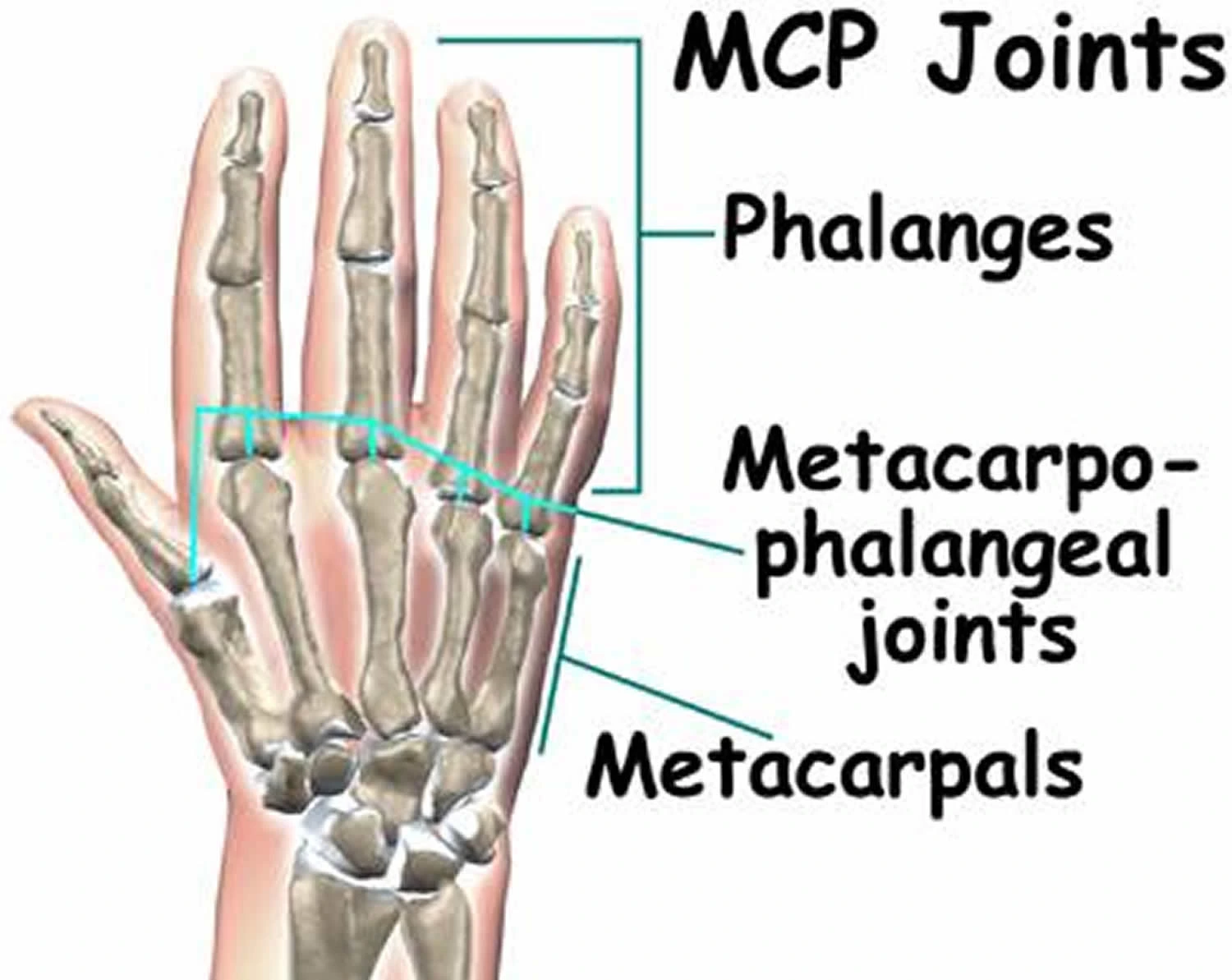
The metacarpophalangeal [ MP or MCP] joint, also known as “the knuckle,” is assembled by the articulation of the proximal phalanx & metacarpal head. This multiaxial joint permits flexion & extension as well as abduction & adduction movements. The MCP joint also dynamically corresponds with the interphalangeal (IP) joint to function in thumb opposition & cross-finger flexion. The MCP joint has substances in several congenital or developed malformations, sports-related damages, & degenerative disorders, & sequelae.
Structure and Function of MCP Joint
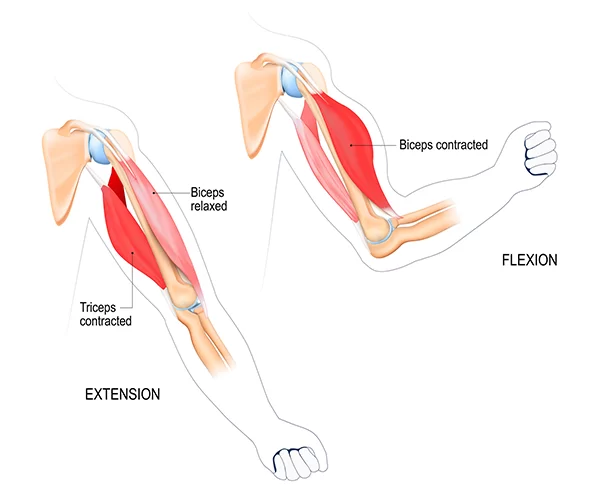
The MCP joint is reliable for 2 planes of movement; flexion & extension, as well as abduction & adduction.
Thumb MCP joint
The proximal convex surface of the 1st metacarpal bone is countered by the oval cavity of the proximal phalanx. Further, 2 sesamoid bones secured by intersesamoid ligaments are present in the palmar element of the joint capsule. The first MCP joint delivers additional flexion to the thumb in antagonism, allowing the grasping & contouring of objects to encourage fine motor studies. Unlike the other digits of the hand, the thumb joint just has one interphalangeal joint, and the MP joint corresponds to thumb opposition. Compared to the other MCP joints of the hand, the MCP joint of the thumb has a more limited range of motion [ROM ].
Finger MCP joints
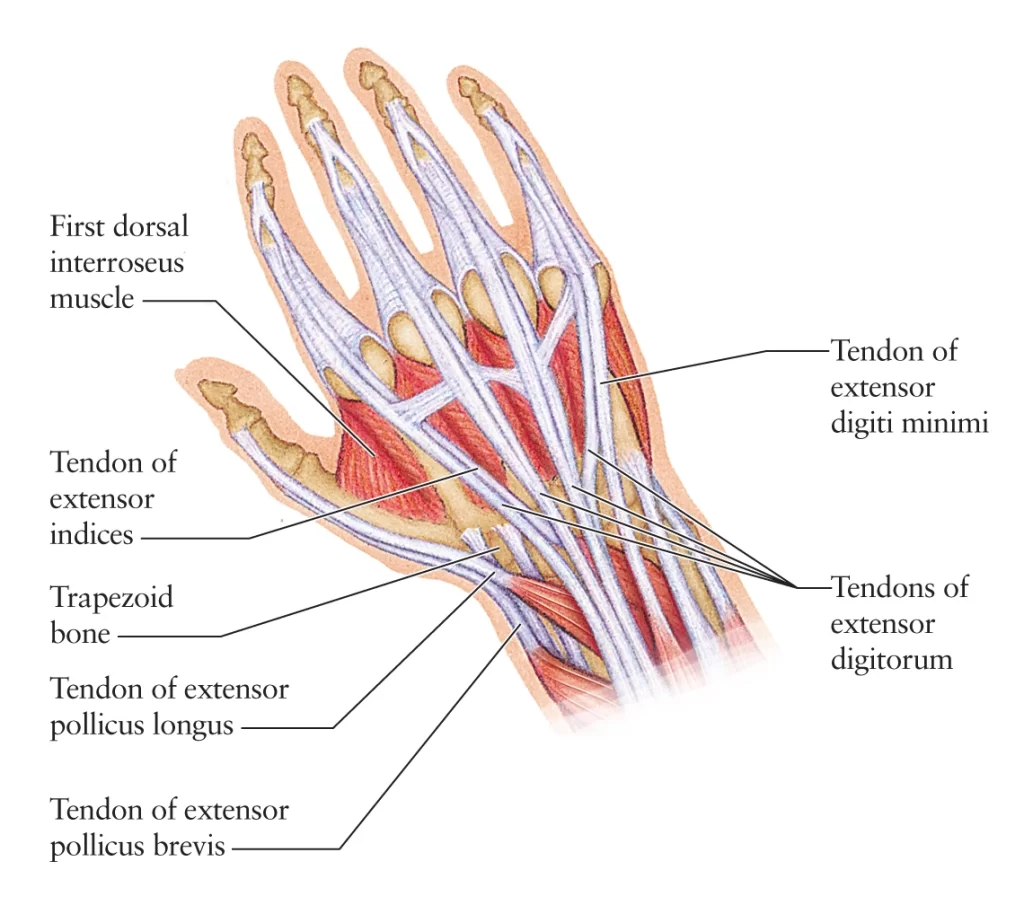
The finger MCP joints have an elliptic convex metacarpal surface that articulates with a concave, shallow proximal phalangeal surface. Despite their structural parallels, these joints are much less limited in movement corresponding to the 1st MCP joint of the thumb. Comprehensive musculature stabilizes these joints. On the palmar aspect, the flexor digitorum superficialis, flexor digitorum profundus, lumbricals, interossei, flexor digit minimi, flexor pollicis longus, & flexor pollicis brevis muscles support the joint. Dorsally, the extensor digitorum, extensor indicis, extensor digiti minimi, extensor pollicis longus, & extensor pollicis brevis muscles support the joint.
Different ligamentous structures such as the volar plate, longitudinal fibers of the joint capsule, & transverse metacarpal ligaments [ superficial & deep] supply extra stability to the joint.
From deep to superficial, the anatomic structures of the MCP joint reduce the overall dynamic function of the MCP joint containing:
- Volar plate
- Joint capsule fibers
- Deep transverse metacarpal ligament
- Flexor digitorum profundus (FDP) tendon
- Flexor digitorum superficialis (FDS) tendon
- Digital tendon sheath
- A1 annular pulley
The volar plate is a short, transverse thickening of the joint capsule that functions to improve overall joint agreement & prevents MCP joint hyperextension.
The joint capsule is a thin, fibrous, & enduring network, supported by the flexor pollicis brevis & adductor pollicis brevis muscles, the palmar plate, & various collateral ligament relations. The radial & ulnar collateral ligaments originate proximally from their separate sides on the metacarpal bone, traveling the distal & volar sides of the joint to connect on the proximal phalanx. Each collateral ligament has its own proper & additional ligamentous structures.
The volar fan-shaped supplement ligament connects to the middle of the metacarpal head & extends to the palmar plate & deep transverse metacarpal ligament which tightens during finger extension. The dorsal, cord-shaped, proper ligament connects to the metacarpal head & extends to the proximal phalanx base, evolving taut at about 30 degrees of finger flexion. The natatory ligament, also comprehended as the surface transverse metacarpal ligament, originates distal to the MCP joint & travels via the webspace to insert on the proximal phalanx. It works to resist abduction. The deep transverse metacarpal ligament attaches the 2nd to 5th metacarpal heads together at the volar plate & delivers soft tissue support. Dorsal to this ligament is the ribbon-shaped sagittal bands that concentrate the MCP joint & stabilize the extensor tendons in movement.
Embryology of MCP joint
The Metacarpophalangeal joint includes a cavity in the mesenchyme between developing bones. The mesenchyme also provides rise to the joint capsule & other ligaments that stabilize the joint. The upper limb bud occurs around the 4th week of gestation, with the effect of the MCP joint occurring around 6 to 7 weeks of gestation. The sesamoid bones of the 1st metacarpophalangeal joint do not occur until approximately 12 years of age.
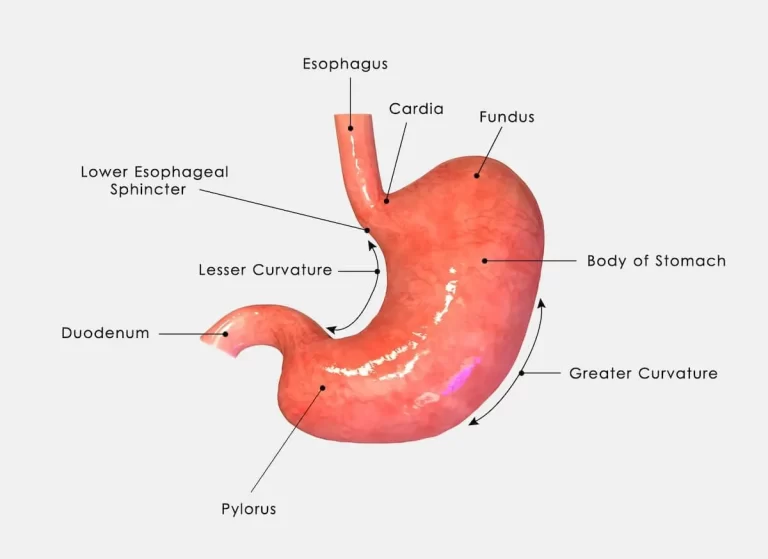
Blood Supply and Lymphatics
The preliminary blood supply to the hand is via the radial & ulnar arteries. The ulnar artery provides rise to the superficial palmar arch & gives off a deep branch to anastomose with the deep arch. The radial artery provides rise to the deep arch & gives off a superficial branch to anastomose with the superficial arch. This forms an extensive collateral network to control ischemia injury. Blood supply to the thumb MCP joint may be directly from the superficial arch or through a deep branch of the radial artery; the princeps pollicis artery. The arterial supply to the MCP joints of the fingers is by branches from contiguous digital arteries.
The axillary lymph nodes supply lymphatic drainage of the upper limb. The lymphatic system of the upper extremity uses a pathway that arises in the distal fingers tips & palms. The lymphatic system runs on the dorsal part of the hand. The lymphatic vessels are generally found just posterior to the cutaneous veins. The lymph drainage resumes proximally up the arm, running with the basilic vein until joining to the lymph nodes in the lateral axillary area.
Nerves supply of MCP joint
The MCP joint obtains innervation from the articular branches of the dorsal & palmar digital nerves. The 2nd-5th MCP joints obtain innervation from a deep branch of the ulnar nerve that is superficial to the interosseous muscles, but deep & radial to the flexor tendon.
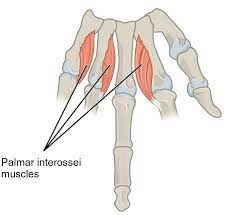
Muscles around the Metacarpophalangeal Joint
Several muscles are counteracting the actions of the MCP joint. The extrinsic & intrinsic hand muscles function in flexion & extension respectively. The intrinsic muscles working on the MCP joint include;
- Abductor pollicis brevis
- Adductor pollicis
- Dorsal interosseus
- Palmar interosseus
- Flexor digiti minimi
- Flexor pollicis brevis
- Lumbrical muscles.
The extrinsic muscles working on the MCP joint include;
- The flexor digitorum profundus
- Flexor digitorum superficialis
- Flexor pollicis longus
- Extensor digitorum communis
- Extensor indicis proprius
- Extensor digiti minimi
The flexor digitorum superficialis & flexor digitorum profundus muscles are the flexors of the MCP joint. The flexor digitorum superficialis muscle produces additional torque at the metacarpophalangeal joint than the flexor digitorum profundus muscle. Corresponded to the flexor digitorum profundus, the flexor digitorum superficialis muscle crosses more irregular joints & is less likely to lose tension as it shortens. The flexor pollicis brevis bends the thumb MCP joint. The flexor digiti minimi muscle bends the MCP joint of the little [ pinkie ] finger.
The dorsal interosseous muscles work mainly in MCP joint abduction. The abductor pollicis brevis & abductor digiti minimi muscles act similar functions at the thumb & pinky respectively. The palmar interosseous muscles perform adduction of the MP joint to complete spread fingers. The lumbrical muscles are intrinsic muscles that are powerless metacarpophalangeal flexors that simultaneously extend the IP joints.
Thumb extension at the MCP joint is a procedure of the extensor pollicis brevis & extensor pollicis longus muscles. Extension of the MCP joint of digits 2 to 5 is a function of the extensor digitorum communis, extensor indicis, & extensor digiti minimi. Especially, the extensor indicis & extensor digiti minimi muscles extend the MCP joints at the index & little fingers respectively. The extensor digitorum communis muscle produces tension over the sagittal bands & pulls them over the proximal phalanx, to complete MCP joint hyperextension.
Physiologic Variants
The literature represents anatomic variation concerning the area of the sesamoid bones of the MCP joint. In complement to the thumb MCP joint, sesamoid bones are sometimes present at the metacarpal heads of the index & little [ pinky ] fingers.
Surgical Considerations
MCP joint arthritis is a recurring topic in the literature discussing different situations that ultimately result in mild to end-stage degenerative changes & deformation that can immensely impact a patient’s ability to perform necessary daily functions. In milder forms of acquired [ For instance post-traumatic ] or degenerative arthritis & deformity, nonoperative measures are the standard, first-line treatment options:
- Rest, activity change
- Oral or topic anti-inflammatory drugs
- Cortisone injections
- Splinting
Additionally, the healthcare provider should evaluate the underlying etiology as this may suggest additional management options. For instance, patients with underlying rheumatoid arthritis should receive a referral to a rheumatologist for technological medical treatment to believe starting the patient on disease-modifying antirheumatic drugs [ DMARDs ].
Continued symptoms, synovitis, or swelling despite a 3 to 6-month period of nonoperative interventions warrants consultation with a hand specialist for possible surgical concerns. Considerations for surgery, specifically in patients with RA, need a comprehensive evaluation of the patient’s overall health & nutritional status, comorbidities, pharmacologic disease control, & infection risk. Additionally, the degree of bone deformation, which contains an assessment of total bone loss, will help to decide, the most likely surgical choices for the patient.
- Metacarpophalangeal Joint Arthroscopy
- Metacarpophalangeal joint arthroscopy was 1st explained in 1979, although in general, its use remains restricted.
Metacarpophalangeal Joint Arthroplasty
The primary indication for MCP joint arthroplasty is painful degenerative arthritis, but the process also can be used to treat joint deformations from multiple dislocations, subluxations, and cartilage damage.
MCP joint arthroplasty remains a somewhat reliable method in terms of its ability to restore function, relieve pain, & improve both function & range of motion [ ROM ].
This process practically affects the replacement of the deformed joint with a hinged silicone implant, or newer-generation, unconstrained implants designed with either hydrocarbon or metal on polyethylene, are considered to be most likely to produce good long-term results in patients with pre-existing soft-tissue stability. In patients with end-stage degenerative deformations involving the compromise of the surrounding soft tissue stabilizing structures, silicone implants are the favored option. The pyrolytic carbon joint reserves occur to be preferable for patients with well-controlled osteoarthritis or early RA with no or minimal deformation. The process begins with a dorsal incision at the metacarpal neck.
The extensor tendons are abandoned to expose the joint capsule. The sagittal band & collateral ligaments are released followed by the joint capsule. The metacarpal head is resected & prepared for implantation of the prosthesis. The patient is advised to stay in a splint for 12 weeks & start physical therapy at week 6 post-operation.
Metacarpophalangeal Joint Arthrodesis
Metacarpophalangeal joint arthrodesis, also known as “MCP joint fusion,” is generally used to fix MCP joint arthritis in the thumb. This surgical procedure usually implicates a dorsal incision. The extensor interval is marked longitudinally, & the dorsal capsule is split to reveal the joint. Following the stripping of the diseased cartilage, fixation is possible via a variety of means, involving screws, plates, & wires. Adjuvant allograft or autograft bone grafting is serviceable in cases of severe bone loss or deformation. The patient needs immobilization for 4 – 6 weeks or until radiographic union occurs.
Clinical Significance
MCP Joint Arthritis in Patients with Rheumatoid Arthritis
Rheumatoid arthritis is a typical autoimmune disorder associated with a developed disability caused by synovial inflammation & hyperplasia that cause the production of autoantibodies, rheumatoid factor, & anti-citrullinated protein antibodies which attack the MCP joint & lead to increasing degrees of swelling, pain, & underlying cartilage & osseous destruction. Cardiopulmonary conditions, psychological conditions, & musculoskeletal difficulties are also characteristic of this disease.
MCP joint arthritis is a characteristic feature of rheumatoid arthritis. In RA, the collapse of the MCP joint connective tissue causes an imbalance of the active & passive forces, directing to joint instability, pain, & deformity. A specific early result of the condition is bilateral symmetric swelling of the MCP joints. Pain with passive movement or squeezing of the MCP joints is a sensitive test for the joint inflammation that continually presents with this situation. This joint dislocation is mostly seen in the end range of movement as flexion & ulnar variation, with dislocation of the joint. Surgical intervention is a patient-centered determination to consider when the deformation severely restricts function.
MP Joint Dislocation
Metacarpophalangeal [ MCP ] joint injuries & dislocations of the fingers & thumb commonly arise secondary to direct trauma or fall.
A patient with an MCP joint dislocation will generally present with a swollen, bruised, & deformed finger. The patient will be focally tender to palpation over the joint itself in complement to the limited ability to move the finger.
Dislocations are defined concerning the distal osseous fragment or bone’s position proximate to the proximal osseous component. Dorsal dislocations are the most typical presentation design. In addition, dislocations are further categorized as simple versus complex. The former indicates a successfully closed decrease is achieved by applying axial traction & splinting, while the latter implies the MCP joint dislocation is fundamental by closed means.
The classic definition of complex dorsal MCP dislocations are:
Proximal phalanx hyperextension
Volar plate rupture & avulsion off of the proximal metacarpal head
The volar plate interposes & restrains closed reduction as it lies on the dorsum of the metacarpal head
Flexor tendons show ulnar expulsion: metacarpal head displaces in both radial & volar directions
Metacarpal head “button-holes” between 4 designs:
- Lumbrical
- Superficial transverse ligament [ proximal ]
- Transverse bands of the natatory ligaments [ distal ]
- Flexor tendon on the ulnar side of the dislocated digit
Complex MCP dislocations, by description, need open reduction to release the interposing structures which are restricting reduction.
For the thumb MCP joint, anatomical forms that may become entangled contain the volar plate, sesamoid bones, bony fracture fragments, & the flexor pollicis longus tendon.
Thumb Collateral Ligament Injury
Thumb collateral ligaments contain damages to the radial collateral ligament [ rare ] or ulnar collateral ligament [ UCL ]. Thumb UCL damages can also be defined established on existing eponyms in the literature:
- Chronic thumb UCL damages: gamekeeper’s thumb
- Acute thumb UCL damage: skier’s thumb
- Stener lesion:
- By description, it indicates complete UCL avulsion & displacement above the adductor aponeurosis. The aponeurosis then lies between the UCL & its attachment site, controlling healing.
- Stener lesions can contain thumb UCL avulsion with or without an avulsed osseous affection.
Patients will generally present with a swollen, discolored thumb, with pain that is aggravated by activity in any direction. Patients may also present important weakness of grasp, at the base of the thumb in the 1st webspace, & wrist pain. The mechanism of injury is generally hyperextension of the MCP joint.
Failure to correct a Stener lesion inevitably results in chronic pain, instability, deformity, deficiency, & arthritis. This leads to a UCL tear being managed surgically to control long-term disability.
Milder damages & ligamentous sprains [ without instability ] are amenable to nonoperative treatment. A thumb spica splint may be used until symptoms determine.
Sagittal Band Rupture
Sagittal band rupture is known as “boxer’s knuckle,” for its disposition to commonly involve members of the fighter profession. This damage involves a traumatic extensor tendon rupture on the dorsal part of the MCP joint. Sagittal band rupture usually goes unnoticed because the extensor tendon can stay in its normal midline position following the injury. Symptoms range from MCP joint pain & edema, due to extensor tendon dislocation. Associated damages contain capsular injury, collateral ligament sprains, & osteochondral fractures. Many critical damages can be treated nonsurgically using extension splints. The optimal administration of chronic or subacute damages remains unclear. Surgical treatment affects the repair or reconstruction of the radial sagittal band.
FAQ
The metacarpophalangeal (MCP) joint is categorized as a condyloid synovial joint. It combines each digit into the palm. The metacarpophalangeal joint consists of an articulation between 2 bones of the hand: Metacarpal head – large articulating surface, convex shape.
The metacarpophalangeal (MCP) joint is categorized as a condyloid synovial joint. It combines each digit into the palm. The metacarpophalangeal joint consists of an articulation between 2 bones of the hand: Metacarpal head – large articulating surface, convex shape.
The metacarpals are the five bones discovered between the wrist & the fingers, including the thumb. The MCP joints are condyloid joints that permit action back & forth as well as side-to-side [ fanning the fingers ].
Five different metacarpophalangeal joints attach each metacarpal bone to the corresponding proximal phalanx of each finger.
Each metacarpophalangeal joint is constructed by the convex heads of the metacarpal bones which are accepted by the concave bases of the proximal phalanges. The primary movements of the metacarpophalangeal joints are flexion, extension, abduction, adduction, circumduction, & restricted movement.
The metacarpophalangeal joint capsule is supported by numerous ligaments & contiguous musculoskeletal structures. The medial & lateral parts of the joint capsule are supported by proper & accessory collateral metacarpophalangeal ligaments.
The arterial supply to the MCP joints is supplied by branches of the radial & ulnar arteries: The movements in the metacarpophalangeal joints include flexion, extension, adduction, abduction, circumduction, and fixed rotation.

23 Comments