Hypothenar Hammer Syndrome
Table of Contents
What is a Hypothenar Hammer Syndrome?
Hypothenar hammer syndrome, also known as HHS, is a rare condition that affects the hand and occurs as a result of repetitive trauma to the hypothenar eminence. The hypothenar eminence is the fleshy area of the palm below the pinky finger.
This condition usually occurs in people who engage in activities that involve repetitive and forceful use of their hands, such as using tools such as hammers or vibrating tools. It can also occur in athletes who repeatedly hit the ball with their hands, such as baseball or handball players.
Repeated trauma can damage the hypothenar blood vessels, causing them to narrow or become blocked. This reduces blood flow to the area, causing symptoms such as pain, sensitivity to cold, numbness, and, in severe cases, even ulceration or necrosis.
Anatomy of Hypothenar Muscles
The anatomy of the hand is critical to understanding hypothenar hammer syndrome. Let’s study the relevant anatomical structures:
Hypothenar Eminence:
- The hypothenar is a muscle area on the side of the palm below the pinky finger.
- It consists of several muscles, including the abductor digiti minimi, flexor digiti minimi brevis, and opponens digiti minimi.
- The hypothenar eminence provides strength and control to the pinky finger and promotes grip and fine motor skills.
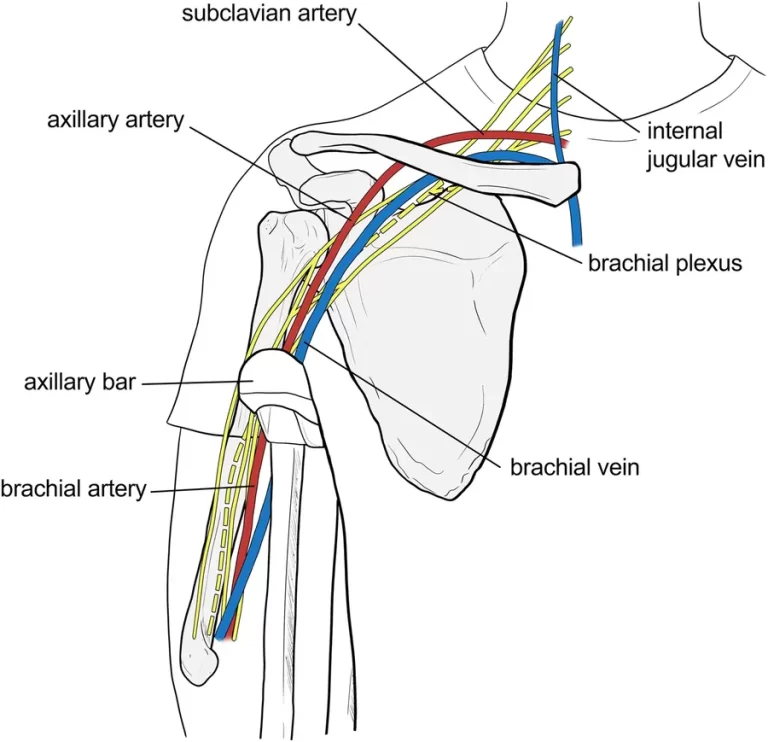
Ulnar artery:
- The ulnar artery is one of the most important blood vessels supplying the hand.
- It runs along the inner (medial) side of the forearm and enters the hand through Guyon’s canal, a passage formed by the hamatum and the hook of the bone in the form of a bone.
- In the hand, the ulnar artery gives off various branches that supply blood to the palm, fingers, and hypothenar eminence.
Ulnar nerve:
- The ulnar nerve runs along with the ulnar artery of the forearm and hand.
- It supplies sensory and motor nerve to the hypotenuse muscles and the muscles that control the movement of the pinky and half-ring fingers.
- The ulnar nerve also senses the skin on the ulnar side of the hand and fingers.
Bookmark:
- The ulnar artery forms the superficial and deep palps in the palm.
- These arches are interconnected networks of blood vessels that supply the palm and fingers with blood.
- A deep palmar arch provides a hypothenar eminence.
- In hypothenar hammer syndrome, repeated trauma or compression of the hypothenar eminence can cause damage to blood vessels, particularly the ulnar artery.
Repeated trauma can damage the walls of the artery, causing narrowing or blockage. This reduces blood flow to the hypothenar eminence and can cause symptoms such as pain, sensitivity to cold, and numbness. Understanding the anatomy involved in hypotension hammertoe syndrome can help diagnose the condition, plan treatment options, and manage its effects on affected structures.
Cause of Hypotenic Hammer Syndrome
Hypothenar hammer syndrome is primarily caused by repetitive trauma or compression of the hypothenar eminence of the hand. This condition is usually seen in people who engage in activities that involve repetitive and forceful use of their hands. Here are the main causes of hypothenar hammer syndrome:
Professional activity:
- Individuals who perform tasks that involve repetitive impact or hand vibration are at increased risk for developing hypothenar hammer syndrome.
- This includes occupations such as carpentry, construction, mechanics, and manufacturing where tools such as hammers, pneumatic tools, or vibrating tools are widely used.
Sports activities:
- Athletes who repeatedly hit a ball or object with their hand, such as baseball players, handball players, or martial artists, may develop hypothenar hammer syndrome.
- Repeated impact on the hypothenar eminence can lead to injury and subsequent vascular problems.
Hobbies and interests:
- Certain hobbies or recreational activities that involve repetitive arm movements or strikes can contribute to hypothenar hammer syndrome.
- Examples include playing certain musical instruments (such as percussion instruments), hand drumming, and activities such as using a hammer to split wood.
Traumatic injuries:
- Hypothenar hammer syndrome can also result from an acute traumatic injury to the hypothenar eminence or the ulnar artery.
- Direct blows or crushing injuries to the arm can damage the blood vessels, which can lead to vascular problems and hypothenar hammer syndrome.
- It is important to note that hypothenar hammer syndrome is relatively rare compared to other hand disorders. Repeated trauma or compression damages blood vessels in the hypothenar region, causing decreased blood flow and associated symptoms.
- If you suspect you may have hypothenar hammer syndrome or are experiencing symptoms, it is important to see your doctor for an accurate diagnosis and appropriate treatment.
Symptoms of Hypothenar Hammer Syndrome
Symptoms of hypothenar hammer syndrome are usually caused by decreased blood flow and damage to blood vessels in the hypothenar region of the arm. The disease may come up with a mixture of signs and symptoms, including:
Pain:
- Pain is a common symptom of hypothenar hammer syndrome.
- The pain is usually located in the hypothenar eminence, which is the fleshy area below the pinky finger.
- The pain can range from mild to severe and can be aggravated by activities that involve grasping or using the hand.
Cold sensitivity:
- The affected hand may become more sensitive to cold temperatures.
- Decreased blood flow to the hypothenar eminence can cause poor temperature regulation, causing the hand to feel colder than usual.
Numbness or tingling:
- There may be numbness, tingling, or “pins and needles” in the reddened finger of the hand or on the side of the ulna.
- This is due to impaired nerve function due to reduced blood flow or nerve compression.
Weakness or decreased grip strength:
- Some people with hypothenar hammer syndrome may experience weakness or decreased grip strength in the affected hand.
- This can make it difficult to perform tasks that require fine motor skills or a strong grip on objects.
Skin changes:
- In advanced cases, skin changes may occur. The skin over the hypotension eminence may appear pale, thin, or shiny.
- Ulcers or ulcers may form in severe cases, and necrosis (tissue death) may occur in extreme cases.
- It is significant to note that the harshness of symptoms may vary from person to person.
- Some individuals can communicate mild discomfort, while others may have more severe symptoms.
- If you suspect that you have hypothenar hammer syndrome or are experiencing these symptoms, it is recommended that you see a doctor for a proper evaluation and diagnosis.
- They can provide appropriate treatment options depending on the severity of the condition.
Diagnostic procedure
The diagnostic procedure for hypotension hammer syndrome usually involves a combination of medical history evaluation, physical examination, and diagnostic tests.
Medical history:
- Your doctor will begin by taking a detailed medical history that includes information about your symptoms, work or recreational activities that involve using your hands, and any related past injuries.
- This information will help determine a possible connection between your symptoms and hypothenar hammer syndrome.
Physical Examination:
- A full physical examination is performed, focusing on the affected arm and hypothenar.
- A healthcare provider will assess pain, tenderness, changes in skin color or texture, and other abnormalities.
- They may also evaluate your hand’s strength, grip, and sensation to assess nerve function.
Imaging studies:
Various imaging studies can help confirm the diagnosis and assess the extent of vascular damage. These may include:
Doppler ultrasound:
Doppler ultrasound uses sound waves to see blood flow in arteries and veins. This can help detect a narrowing or blockage of the ulnar artery or other blood vessels in the hand.
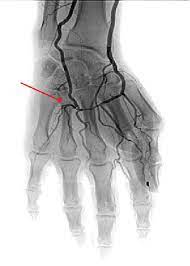
Angiography:
Angiography involves injecting contrast material into blood vessels and taking X-rays. This provides detailed imaging of the blood vessels and helps identify any abnormalities such as stenosis or blockage.
Magnetic resonance Angiography (MRA):
MRA is a non-invasive imaging technique that uses magnetic resonance imaging (MRI) to visualize blood vessels. It can provide detailed information about blood circulation and detect possible vascular disorders.
Nerve conduction studies:
- Nerve conduction studies may be performed to evaluate the function of the ulnar nerve and rule out other nerve-related conditions.
- These tests involve applying small electrical impulses to the nerves and measuring the response.
- These can help determine if nerve damage or compression is contributing to symptoms.
Based on the history, physical examination, and results of diagnostic tests, a healthcare provider can diagnose hypothenar hammer syndrome. It is important to consult a doctor for an accurate diagnosis and treatment recommendations tailored to your situation.
Treatment of Hypothenar Hammer Syndrome
Medical treatment for hypothenar hammer syndrome aims to relieve symptoms, improve circulation, and prevent the condition from progressing. Specific treatments may vary depending on the severity of the syndrome and the general health of the individual. Here are some common approaches to medical treatment:
Conservative Treatment of Hypothenar Hammer Syndrome
Activity modification:
- It is important to avoid or minimize activities that aggravate symptoms.
- This may require changing work tasks or using protective measures such as pads or anti-vibration gloves.
Avoid the cold:
- Protecting your hands from the cold by wearing warm clothes or hand warmers can help reduce the symptoms of cold sensitivity.
Medication
- Over-the-counter pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can help relieve pain and reduce inflammation.
- Other medications, such as vasodilators, may be prescribed to improve blood flow to the affected area.
Occupational therapy:
Hand therapy:
- A hand therapist can provide exercises and techniques to improve hand strength, range of motion, and function.
- They can also provide training on proper ergonomics and hand protection while working.
Medicines:
Blood thinners:
In some cases, anticoagulants may be prescribed to prevent blood clots and improve blood flow in damaged blood vessels.
Vasodilators:
Medicines that promote blood vasculature may be prescribed to improve blood circulation in the hands.
Intervention measures:
Thrombolysis:
In cases where a blood vessel is blocked by a clot, a procedure called thrombolysis can be performed to dissolve the clot and restore blood flow.
Angioplasty or stenting:
In more severe cases, when the blood vessels are significantly narrowed or blocked, angioplasty or stenting procedures may be considered. These procedures involve widening the narrowed blood vessel or inserting a stent to keep it open.
Surgical interventions:
- Surgical options may be necessary for severe or advanced hypothenar hammer syndrome.
- In extreme cases, these may include bypass surgery, arterial reconstruction, or accidental amputation of the affected fingers.
- The choice of treatment depends on factors such as the severity of symptoms, the extent of vascular damage, and the individual characteristics of the patient.
- It is important to talk to a doctor who will evaluate your condition and recommend the most appropriate treatment plan.
Physiotherapy Treatment in Hypothenar Hammer Syndrome
Physical therapy can play a valuable role in treating hypothenar hammer syndrome by focusing on improving hand function, reducing pain, and improving overall arm and hand strength. Here are some common physical therapy procedures and techniques used to treat hypothenar hammer syndrome:
Therapeutic exercises:
Range of motion exercise
- These exercises aim to improve the mobility and flexibility of the hands and fingers. These may include finger extensions, wrist movements, and thumb movements. Strengthening exercises: Special exercises may be prescribed to strengthen the muscles of the hand, forearm, and upper arm. This can improve grip strength and overall hand function.
Grip and dexterity training:
Various grip and dexterity exercises, such as using an adjustment set or finger and hand manipulation tasks, can help improve fine motor skills.
Progressive resistance exercises:
Gradually increasing resistance using therapeutic bands or weights can improve hand and forearm muscle strength and endurance.
Manual therapy techniques:
Soft tissue mobilization: Manual techniques such as massage and soft tissue mobilization can help relieve muscle tension, reduce pain, and improve blood flow to the affected area. Joint mobilization: Gentle mobilization techniques can be used to improve joint mobility, reduce stiffness, and improve overall hand function.
Treatment of pain:
Heat and cold therapy:
Using hot or cold packs can help reduce pain, inflammation, and discomfort in the affected arm.
Transcutaneous Electrical Nerve Stimulation (TENS):
TENS involves the use of low-level electrical stimulation to relieve pain and promote circulation.
Ultrasound
Ultrasound uses sound waves to promote healing and improve blood flow to the affected area. This may assist relieve pain and inflammation.
Training and ergonomic advice:
Ergonomic Assessment:
Physical therapists can provide advice on proper ergonomics and body mechanics to reduce stress on the arm and prevent further injury.
Activity modification:
Providing instructions for modifying activities to reduce repetitive trauma and hand tremors can be helpful.
Physiotherapy for hypotension hammer syndrome is usually tailored to the specific needs of the individual and can vary depending on the severity of symptoms and the stage of the condition. A qualified physical therapist can create an individualized treatment plan that meets the individual’s goals and optimizes hand function and recovery.
FAQs
Hypotenic hammer syndrome (HHS) is caused by repeated use of the hand as a hammer, causing thrombosis in the superficial palmar arch of the ulnar artery. There is trauma above the hook of the hamate where the superficial branch of the palmar artery is.
Repetitive occupational or recreational trauma can cause injury to the ulnar artery as it courses relatively unprotected across the humerus, resulting in distal vascular injury manifesting as hypothenar hammer syndrome.
Hypotenoid hammer syndrome (HHS) is caused by damage to the ulnar artery either from work or sports. The diagnosis should be suspected when a younger man presents with symptoms of pain, a palpable lump, and ischemia in the dominant arm.
Rest, ice, elevation, and the use of OTC pain and anti-inflammatory medications are usually the best way to get immediate and long-term relief from this injury. See a doctor for noticeably abnormal joints or fractures that cause severe pain or do not respond to basic treatment.