Fibromyalgia Pressure Point
Table of Contents
What is a Fibromyalgia Pressure Point?
The pressure point of fibromyalgia describes sensitive areas on the body that become painful with a high amount of pressure on the area.
- Therapists used to use the phrase “pressure points” (or “tender points”) to describe sensitive areas on the body that become painful with a high amount of pressure on the area.
- The tender point of fibromyalgia is also known as the pressure point of fibromyalgia.
What is fibromyalgia?
- Fibromyalgia (FM) is a long-term condition that causes widespread pain throughout the whole body.
- Doctors used to use “pressure points” to help them form an identity.
- These are areas on the body that feel pressure after giving some firm pressure.
- However, recent guidelines have phased these out and introduced brand-new diagnostic criteria.
- The main symptoms of FM are chronic pain (which may be mild or severe), extreme tiredness, and disrupted sleep.
- Depression or anxiety can also arise from FM’s ongoing impact on everyday life.
- It is hard for doctors to diagnose FM from the symptoms of pain alone.
- Many other factors should come into deliberation while forming a diagnosis.
- Of this fact, physicians no longer use the pressure points described above to diagnose FM.
What are the pressure points?
- Therapists used to use the phrase “pressure points” (or “tender points”) to describe sensitive areas on the body that become painful with a high amount of pressure on the area.
- The tender point of fibromyalgia is also known as the pressure point of fibromyalgia.
- In the past, doctors would diagnose the condition according to a set of criteria that identified eighteen pressure points on the body.
- To qualify for a diagnosis of FM, a patient had to experience pressure in eleven of these tender points.
- The previous pressure points of FM included the following areas on both sides of the body:
- The upper chest
- The back of the head
- The outer elbows
- The knees
- The hips
- The tops of the shoulders.
- However, there were too many problems with these criteria.
- For example, using pressure points was actually contributing to the overdiagnosis of FM.
- Also, an individual with FM may not feel constant pain.
- The pain can be intermittent, and it may even move to various areas of the body.
- Other medical conditions, like polymyalgia rheumatica, can also generate pressure in these areas.
- Many rheumatic diseases — like Lyme disease, rheumatoid arthritis, lupus, and Sjogren’s syndrome — can also generate widespread pain and pressure areas.
What Causes Pressure Points?
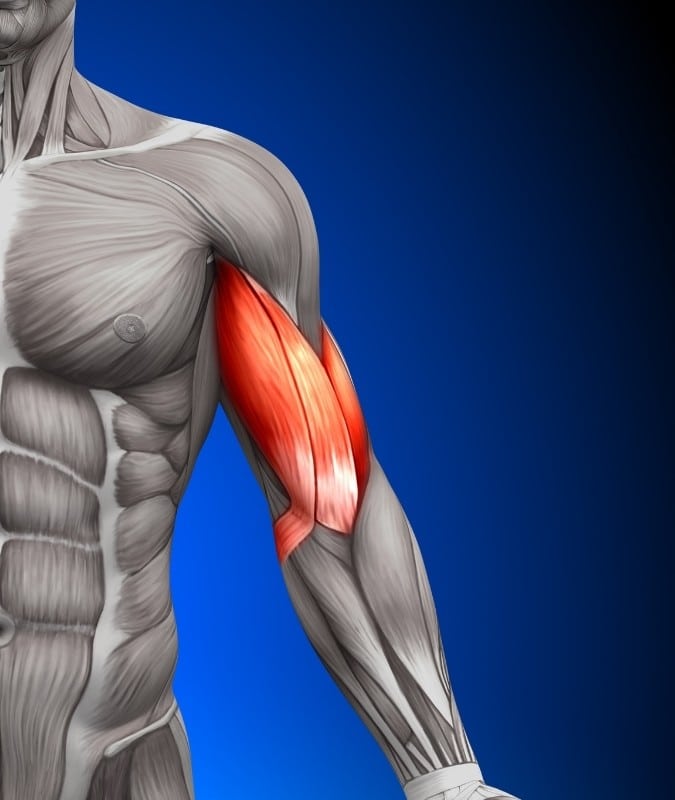
- Although experts do not know particularly what is causing these sensitivities in specific areas, it has to do with muscle spasms. “
- When muscle spasms (involuntary contractions), they tend to have a lack of oxygen and blood.
- That replacement of oxygen and buildup of acid and carbon dioxide generates too much pain in the muscles, which causes greater spasms, and it’s a vicious cycle.”
- Why do muscles have spasms in the first place? “We still do not know the reason for these spasms and increased sensitivities,”
Why Are Pressure Points No Longer Counted Today?
- Fibromyalgia is a challenging disorder to identify because physicians ca not see patients’ symptoms on the body or in blood tests or X-rays.
- Diagnosing fibromyalgia comes down to a physician — often a rheumatologist — listening to a patient’s overall history and symptoms, including their severity and duration.
- The one research center that had researched the Fibromyalgia Diagnostic Criteria, and established that 11 of the 18 pressure points had to be present and cause pain for at least three months.
- But updated guidelines did not require counting pressure points in order to make a fibromyalgia diagnosis.
- The research found that too many patients who had fibromyalgia were not meeting the pressure points criteria.
- When we first latched onto those pressure points, we thought they were more than they turned out to be.
- It requires pressing with a particular force and some physicians use more force than other physicians.
- Counting pressure points turned out to not be very useful diagnostically.
- “The way that one can apply pressure to a patient may be different from another physician.”
- Some other factor is that fibromyalgia pain may deteriorate in location and intensity from day to day.
- One day, a fibro patient could have severe pain in nearly all pressure points.
- On another day, they might have pain in only a few.
- Doctors feel that over-relying on pressure points to make a fibromyalgia diagnosis was leading to too many patients being underdiagnosed.
- The prior criteria that emphasized pressure points also ignored the other chronic symptoms many fibromyalgia patients experiences, including sleep difficulties, fatigue, not feeling refreshed in the morning after sleeping, and cognitive issues like “fibro fog.”
- By that time, the researchers changed their most recent guidelines for diagnosing fibromyalgia that factored in the Widespread Pain Index (WPI), which assesses where the patient felt pain in specific areas of the body, counting a one for each area.
- The Symptom Severity Scale (SSS) score assesses how the pain is experienced in terms of fatigue, cognitive symptoms, and how they feel when they wake up, on a scale of 0 (no pain) to 3 (severe and constant).
The newest criteria for diagnosing fibromyalgia include these factors:
- Utilizing this Widespread Pain Index and Symptom Severity Scale when (WPI) ≥7 and the Symptom Severity Scale (SSS) score ≥5, OR WPI 4–6 and SSS score ≥9.
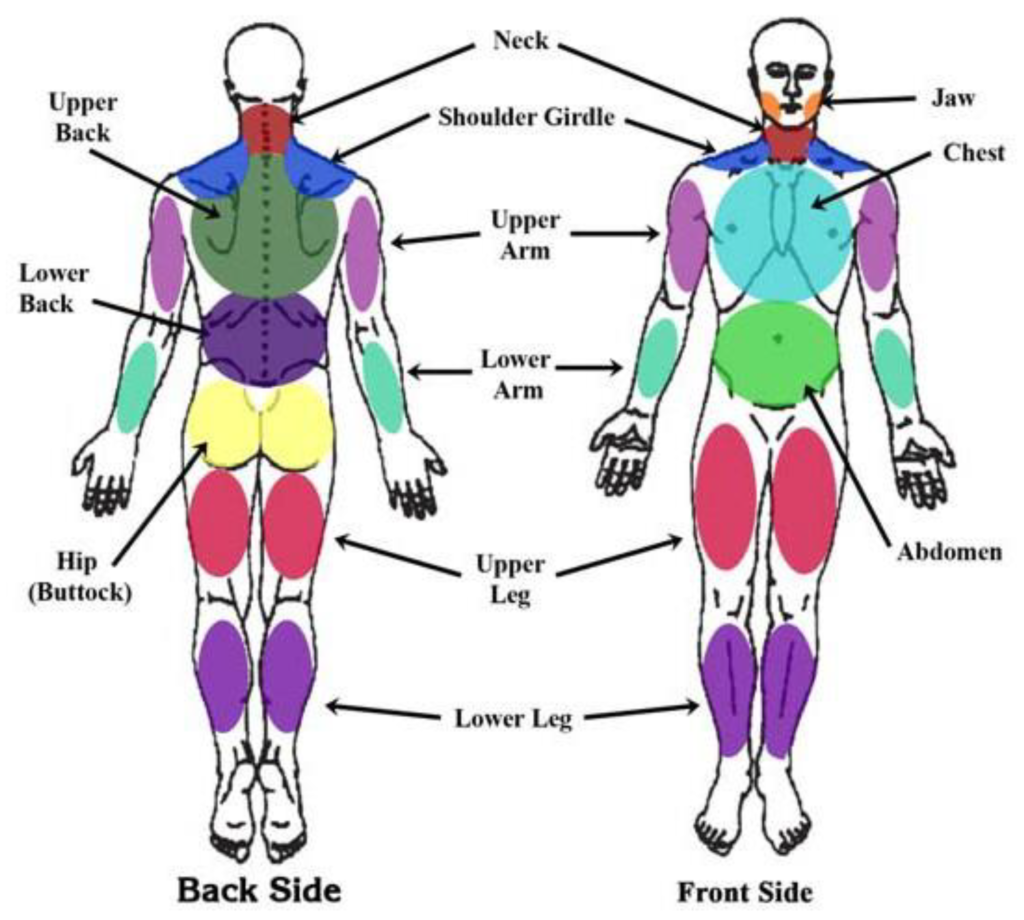
- Generalized pain, described as pain in at least four of five regions (left upper, right upper, left lower, right lower, low back) is present.
- Symptoms have been present and accordant for at least three months Counting pressure points (not required).
- Some of the differences made between the mid-year diagnostic criteria and the ones used today are that the “pain areas” that are counted are the left upper body, right upper body, left lower body, right lower body, and the center of the body (normally low back).
- Now the jaw area, abdominal area, and chest pains are not assessed as part of the criteria.
- The person may have fibro at the same time as other diseases.
Current diagnostic criteria-
- Doctors no longer use pressure points to diagnose FM.
- As the medical community’s understanding of FM advanced, here are newly developed criteria to aid diagnosis.
- These criteria are as follows-
Widespread pain index-
- These criteria do not rely on pressure points that respond to pressure from a finger.
- On the other hand, they take into account the number of areas in which the patient has felt pain over the past week.
- The doctor checks these areas and generates a widespread pain index (WPI) score on a scale from 0 to 19. The areas that qualify include the:
- Hip
- Upper and lower back
- Shoulder girdle
- Upper and lower arm
- Upper and lower leg
- chest
- Neck
- Abdomen
- Jaw
- Some doctors and providers may also use these criteria to rule out other conditions.
Symptom severity scale-
- A doctor can also use a symptom severity (SS) scale, which extracts into account other FM symptoms, like fatigue and depression.
- They will rank the seriousness of each symptom on a scale from 0 to 3, with 0 described as no symptom at all and 3 describes as a severe presentation of this symptom.
- On an equal scale, doctors will also rank the presence of no-pain symptoms. Receiving a score of 0 describe no other symptoms, whereas a 3 would suggest a large number of symptoms.
- They will then merge these SS scores and find out the final score out of 12.
People who meet up with the following criteria are likely to have FM:
- A WPI score of greater than 7 out of 19 and an SS scale score of 5 or higher, or a WPI score between 3 and 6, and an SS scale score of 9 or higher the existence of symptoms at a similar level for 3 months or longer.
- There is no other condition or disorder present that appropriately explains the areas and extent of the pain.
- Some doctors use altered criteria in which they rank the presence of other features as a yes or no choice, rather than having their patients describe the severity of these symptoms.
- These criteria account far better for the presence of no-pain symptoms in people with FM.
What Is the Treatment for pressure Points?
- Treating pressure points involves treating the fibromyalgia condition as a whole and may involve several prescriptions and recommendations for lifestyle modifications.
- Physicians may also advocate the following types of medication to help with fibromyalgia symptoms and pressure point pain:
- Antidepressants
- Anti-seizure medications
- Non-steroidal anti-inflammatory drugs
- Injections of steroids or other medications
- Within these classes, some other medications are approved, which are specifically for fibromyalgia: duloxetine (Cymbalta®), milnacipran (Savella™), and pregabalin (Lyrica®).
- “If there’s one particular muscle group that is more painful than another, then that is where an injection would play a role,”
- The doctor says they might use a local anesthetic and a little amount of cortisone on the affected area.
- “If the muscle continues to be in spasm and does not respond to any kind of exercise and stretching, the person could actually use Botox to keep up the muscle paralyzed.”
- The pain management specialist may recommend a trigger-point injection or myofascial injection with a local anesthetic and steroids, As well, lifestyle modifications are critically necessary for managing fibromyalgia symptoms, especially exercise.
- Exercise can help to address many issues related to fibromyalgia, including anxiety and depression, pain, and fatigue. Getting daily aerobic exercise and doing muscle strengthening can help,”
- “Controlling stressors is a too much necessary thing., Because we know that stress is a crucial determinant in some individuals with fibromyalgia.”
- Alternative therapies to manage fibromyalgia pain include acupuncture, massage, acupressure, physical therapy, yoga, and cognitive behavioral therapy.
Self-help tips and home remedies-
- As well as medication, some complementary treatments can also help some people with FM.
- For example, massage therapy, acupuncture, and yoga can all help individuals better manage their physical and emotional symptoms.
- There are too many steps a person with FM can take to manage their symptoms at home, including exercise-
- Gentle exercise- Gentle rhythmic exercise may help decrease symptoms of FM.
- The National Fibromyalgia Association generally recommends exercise for people who have FM.
- Aerobic exercise — Like walking, swimming, and biking — may improve symptoms. If an individual with FM wants to start an exercise regimen, they should start gently and gradually increase their tolerance to exercise.
Effective sleep hygiene-
- Going to bed at the same time each night and waking at the same time every morning may help a person to create a regular sleep pattern.
- The physician also recommends avoiding caffeine close to bedtime.
- Taking these steps may decrease the impact of FM on sleep hygiene for some individuals.
Relaxation techniques–
- It is useful to find methods to relax each day. As an example, deep breathing, meditation, and yoga may all be beneficial.
- Relaxing may enhance mood, decrease fatigue, and reduce pain.
Getting support-
- Accepting help from family and friends may help, as may seeking professional assistance from a counselor.
- Support groups are also accessible through organizations such as the National Fibromyalgia Association.
FAQ
This is because although the cause of fibromyalgia is said to be not known, scientists have found most to be caused by (myofascial) pressure points. Pressure points are those tender lumps in muscles that therapists find, and massage is an effective pressure point therapy.
If the person has fibromyalgia, one of the main symptoms is likely to be widespread pain. This may be felt throughout the body but could be worse in particular areas, like the back or neck. The pain is likely to be constant, although it may be better or more severe at different times.
Fibromyalgia is a disorder distinguished by widespread musculoskeletal pain accompanied by fatigue, sleep, memory, and mood issues. Scientists believe that fibromyalgia amplifies painful sensations by affecting the way the brain and spinal cord process painful and nonpainful signals.
Various triggers including trauma and stress as well as infections can precipitate the development of FMS. few types of infections including hepatitis C virus, HIV, and Lyme disease have been temporally associated with the development of FMS.
Unusual Symptoms of Fibromyalgia
Paresthesia. One of the symptoms of fibromyalgia is paresthesia.
Brain Fog. Also known as“fibro fog,” this symptom is one of the most frustrating ones and it leads many patients to distress.
Allodynia.
Smell and Sound Sensitivity.
Extreme Sweating.
Lipomas.
Dystonia.