Congenital Diaphragmatic Hernia
Congenital Diaphragmatic Hernia (CDH) is a birth defect where there is an abnormal opening or hole in the diaphragm, the muscle that separates the chest cavity from the abdominal cavity. This condition allows organs from the abdomen, such as the stomach, liver, or intestines, to move into the chest cavity, potentially putting pressure on the lungs and interfering with their normal development. CDH occurs during fetal development and is present at birth.
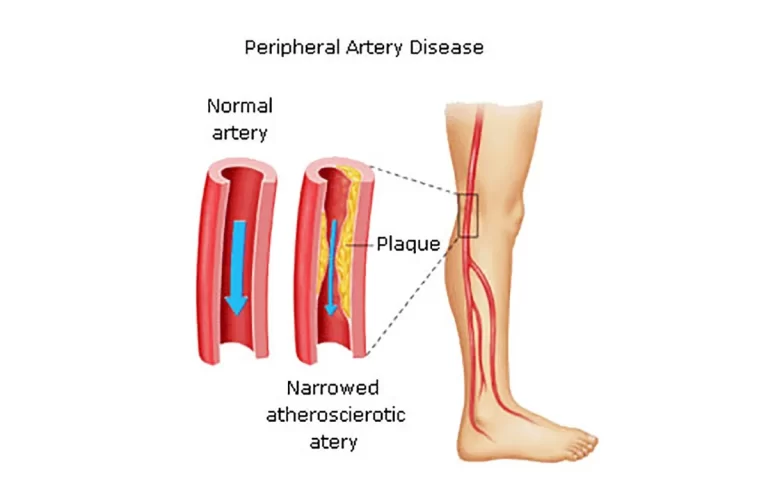
There will be less developed blood arteries and smaller than normal lungs (pulmonary hypoplasia). As a result, pulmonary hypertension—high blood pressure in the lungs—occurs.
One of the most common is a serious congenital condition termed CDH, which affects 1 in every 2,500 to 3,000 live births. CDH can occur on the left, right, or occasionally both sides. Due to the requirement for urgent care after delivery for neonates with CDH, early and accurate diagnosis is essential.
Table of Contents
What is a Congenital Diaphragmatic Hernia?
A rare disorder known as congenital diaphragmatic hernia (CDH) affects a newborn before birth. When a baby’s diaphragm, the muscle that separates the chest from the abdomen, malfunctions early in pregnancy, it causes miscarriage. The diaphragm sustains damage as a result. Hernia is the name of the hole.
The birth abnormality known as congenital diaphragmatic hernia (CDH) takes place during fetal development. It indicates that the fetus’s diaphragm, a muscle barrier that separates its chest cavity from the belly cavity, is either not fully developed or not strong enough to do so. That implies that organs can pass through them. A hernia occurs when an organ pushes through the muscular barrier.
What happens in a Diaphragmatic Hernia?
A diaphragmatic hernia that develops during fetal development has an impact on how the fetus’s body develops. While everything is still developing, its abdominal organs—the stomach, intestines, liver, gallbladder, pancreas, and spleen—can migrate upward into the chest cavity.
When this occurs, the fetus’s chest may get crowded with extra organs, which may hinder the lungs from developing appropriately.
The stomach, liver, intestines, and other abdominal organs may pass through the opening and enter the infant’s chest. The intestines do not form the normal connections that hold them in place in the abdomen if they are in the chest (malrotation). They could twist inward and stop receiving blood (volvulus).
The development of both lungs is impacted, even though the lung on the side of the diaphragm with the hernia is small. The lungs’ internal air sacs (alveoli) don’t grow as they ought to. Blood flow issues and a rise in blood vessel pressure inside the lung are the result of this. After birth, the newborn may have trouble breathing due to elevated blood pressure in the lungs. Additionally, some infants may experience issues with cardiac development.
Before birth, the placenta performs all lung functions to prevent hypoxia (low oxygen levels) in the womb while a fetus is growing. The newborn depends on the lungs after birth, thus if they are severely underdeveloped, artificial ventilation procedures will be required. The left, right, or very infrequently both sides of the chest may have CDH.
In 95% of cases, a diaphragmatic hernia (also known as a Bochdalek hernia) develops in the posterolateral region of the diaphragm, and in 85% of cases, it is on the left side. In 2% of cases, it is bilateral. Incidence estimates range from 1 to 4 per 10,000 live births. Only 5% of people have an anterior hernia, also known as a Morgagni hernia. Adrenal insufficiency is relatively frequent, and other congenital abnormalities are present in roughly 50% of cases.
On the affected side, loops of the stomach, liver, spleen, small and large bowel, and stomach may protrude into the hemithorax. The lung on the affected side will be hypoplastic if the hernia is extensive and there is a significant volume of herniated abdominal contents; nevertheless, the lung on the opposite side may also be negatively impacted.
Underdevelopment of the pulmonary vasculature, which causes an increase in pulmonary vascular resistance and, ultimately, pulmonary hypertension, are other pulmonary side effects. Even with oxygen supplementation or mechanical breathing, persistent pulmonary hypertension causes right-to-left shunting at the level of the foramen ovale or through a patent ductus arteriosus, which precludes proper oxygenation. The main cause of death in newborns with congenital diaphragmatic hernias is persistent pulmonary hypertension.
Causes of Congenital Diaphragmatic Hernia:
There is no known cause of CDH. CDH is normally an isolated finding, though it can occur in association with heart disease or a genetic defect that might add to the challenges. In rare instances, a genetic condition or haphazard gene alterations known as mutations can be connected to CDH. In these situations, the infant may be born with additional difficulties, such as heart, eye, arm, or limb defects, or stomach and intestine problems.
A birth anomaly called congenital diaphragmatic hernia (CDH) occurs. Although its precise cause is uncertain, it might be connected to:
- Genetics.
- Environmental hazard exposure while pregnant.
- Malnutrition in utero.
What brings on CDH?
By 10 weeks of gestation, the diaphragm is fully developed in a developing embryo. However, the process that results in the creation of the diaphragm is hampered in CDH instances. Abdominal contents can enter the chest once the diaphragm has a hole in it. It’s known as a herniation. As pregnancy progresses, the frequency and intensity of fetal activity and breathing motions increase, which causes the herniation’s size to vary or grow.
Sometimes a baby’s chromosome issue or a genetic disease results in CDH. If this is the case, the infant might also have other health issues or organ abnormalities. a genetically identified cause. The severity of the pulmonary hypoplasia brought on by the abnormality is the main issue in this case of isolated CDH. Genetic testing is necessary to ascertain whether CDH is isolated and to deliver the most accurate knowledge possible about the illness.
Signs and symptoms of CDH
In most cases, CDH is discovered during a routine prenatal ultrasound. According to the sonographer, the stomach, intestine, or liver may be visible in the baby’s chest where the lungs should be. The baby’s heart may also be shifted to one side by the additional organs in the chest. The degree of congenital diaphragmatic hernia varies. It could be minor and have little to no impact on the infant, or it could be more serious and impair the body’s ability to get oxygen. Children born with CDH could have
Babies with CDH may exhibit any of the following:
- Strange breathing or severe breathing difficulties brought on by underdeveloped,
- Quick heartbeat.
- Cyanosis is a blue discolouration caused by oxygen deprivation.
- Weak breath noises, typically coming from one side.
- The chest makes bowel sounds. the abdominal cavity and barrel chest. ache in the abdomen.
- Bowel obstruction-related constipation.
- Tiny lungs (pulmonary hypoplasia).
- Pulmonary hypertension
- A high blood pressure condition that affects the right side of the heart and the arteries in the lungs.
- Difficulties with cardiac development.
- If the intestines travel through the hernia and into the chest, they could cause harm to the liver, stomach, liver, and other abdominal organs.
In mild situations, respiratory distress might happen very away after delivery, although it usually develops over a period of many hours.
Following delivery, the neonate’s stomach and intestines quickly fill with air and enlarge, leading to acute respiratory compromise as the heart and mediastinal structures are pushed to the right (most common left-sided hernia), compressing the right lung. It is likely that the abdominal viscera will be displaced into the chest, resulting in a scaphoid abdomen.
Over the affected hemithorax, bowel sounds (and a lack of breath sounds) may be audible. In less severe situations, a minor diaphragmatic defect causes belly contents to gradually herniate, leading to the development of mild breathing trouble a few hours or days later. Rarely, presentation occurs later in childhood, occasionally following an episode of infectious enteritis that results in a rapid protrusion of the colon into the chest.
Diagnosis:
A high-volume fetal facility should perform additional testing on a prenatal ultrasound that reveals CDH.To assess the CDH and general fetal anatomy, use high-resolution fetal ultrasonography.
Fetal echocardiography and ultrafast fetal MRI will assess the structure and function of the heart. With the aid of these specialized tests, we are able to determine the side of the diaphragm that CDH affects (left, right, or both), the organs that are housed in the chest (stomach, intestines, and/or liver), and the size of the lungs in order to calculate the potential impacts on the unborn child.
To make the most precise assessment possible, specialized imaging methods are required, such as magnetic resonance imaging (MRI). After delivery, a congenital diaphragmatic hernia may also be identified, frequently when an infant exhibits breathing difficulties.
Most frequently, a congenital diaphragmatic hernia is identified during a normal fetal ultrasound examination performed before the birth of your child. Sound waves are used in prenatal ultrasound exams to create images of your uterus and developing child. Sometimes the diagnosis is not made until after the baby is born. Occasionally, CDH may not be identified until a kid or later in life. This could be due to the absence of symptoms or the mildness of symptoms including digestive and respiratory issues.
Prenatal ultrasounds and other tests are used by your doctor to monitor the development and operation of your unborn child’s heart, lungs, and other organs throughout your pregnancy.
Prenatal ultrasound: Prenatal ultrasonography can sometimes be used to diagnose a diaphragmatic hernia. A diaphragmatic hernia may be suspected in the birth room when neonates with respiratory difficulties have scaphoid abdomens. Typically, during the first few months (first trimester) of your pregnancy, you receive your first fetal ultrasound. It verifies your pregnancy and reveals the quantity and size of your unborn child or unborn children.
You often undergo a second ultrasound during the second trimester, which lasts from months four to six. Your baby’s growth and development are monitored by your doctor. Your doctor examines the position, size, and other organs of your unborn child. Your healthcare professional could recommend more frequent ultrasound tests if your infant exhibits CDH symptoms. This can demonstrate the severity of CDH and whether it is escalating.
A routine ultrasound may detect CDH if it finds extra amniotic fluid and/or abdominal contents in the fetal chest cavity. Doctors may perform a highly thorough ultrasound, run chromosome testing on the fetus, and measure the size of its lungs to confirm a prenatal diagnosis of CDH. Doctors concentrate on particular ultrasound examination results that can indicate the existence of a condition.
X-ray: A chest X-ray taken after delivery is used to diagnose cases when the stomach and intestine protrude into the chest. The hemithorax of a big defect is filled with multiple air-filled intestinal loops, and the heart and mediastinum are displaced contralaterally. The abdominal contents show up as an opaque, airless mass in the hemithorax on an x-ray obtained immediately after delivery before the newborn has swallowed air.
Amniocentesis is used to do the genetic testing. The lung size is then measured and contrasted with the size that would be anticipated at this point in the pregnancy.
Observed/expected lung area to head circumference ratio (o/e LHR) comparison or lung area to head circumference ratio (LHR) measurement can be used to do It’s also critical to check to see if the liver has entered the chest.
- Additional tests:
Evaluate the organ function of your infant, more tests could be performed. These may consist of:
- Magnetic resonance imaging (MRI) of the fetus. A magnetic field and radio waves produced by a computer are used in this medical imaging procedure to produce precise pictures of the baby’s organs and tissues.
- Liver herniation into the chest has been confirmed by this rapid fetal MRI. The location of the liver is the best indicator of CDH severity. More pulmonary hypoplasia (small lungs) is present when the liver is positioned higher up in the chest. Predictions of the degree of pulmonary hypoplasia can be made using measurements obtained during foetal ultrasonography and MRI.
- Echocardiography of the fetus: An echocardiography creates images of the baby’s heart beating and pumping blood using sound waves. An echocardiogram’s scans can reveal issues with the heart’s development.
- DNA analysis; Genetic testing can reveal genetic abnormalities or other variations in the genome that are occasionally linked to CDH. You can learn more about your baby’s condition and how to understand these test findings with the aid of genetic counseling. assessing CDH severity prior to birth scans of CDH
Treatment of Congenital Diaphragmatic Hernia
Congenital or acquired diaphragmatic hernias typically require prompt surgery.
Surgery is required to remove the abdominal organs from the chest and return them to the abdomen. The surgeon will next repair the diaphragm.
Surgeons may conduct surgery for a CDH as soon as 48 to 72 hours after delivery. In an emergency, Surgery may be carried out sooner or later in an emergency. Every situation is unique. The infant must first be stabilized and have its oxygen levels raised. The baby is stabilized and given breathing assistance using a range of drugs and methods. A facility with a highly specialized Neonatal Intensive Care Unit (NICU) is the ideal place to care for these infants. After the infant has stabilized, surgery can be performed.
Every little thing counts and has an effect on CDH infants’ outcomes. It’s crucial that your baby get care from a group with expertise in caring for infants with CDH.
Your baby’s CDH therapy may involve surgery as well as the use of specialist tools like the oscillator ventilator, heart-lung machine (ECMO), or nitric oxide. Even if they don’t require these alternatives, it’s crucial that they have quick access in case they do.
ECMO:
If the infant is unstable, extracorporeal membrane oxygenation (ECMO) may be used.
With ECMO, the baby’s lungs may take a break as a machine replaces the heart and lungs, providing oxygen while eliminating carbon dioxide, a waste product of respiration.
Congenital repair of a diaphragmatic hernia:
Surgery to correct CDH after delivery depends on how each individual infant does in the first few days after birth.
The time of the diaphragm repair will be decided by the multidisciplinary team, which is headed by the pediatric surgeon and neonatologist who will care for your infant. In our opinion, it is advisable to hold off until the kid has transitioned off ECMO and the lungs exhibit reduced resistance due to pulmonary hypertension. To improve this procedure, our skilled staff uses a variety of drugs and inhalation treatments.
Due to the acute sensitivity of babies with CDH to noise and movement, surgical CDH repair is frequently carried out in the N/IICU. The surgical team converts your baby’s N/IICU bedside into an operating room when it’s time for the repair. By doing this, the infant won’t experience the added stress of needing to be relocated.
A pediatric anesthesiologist will keep an eye on your infant when general anaesthesia is administered. Just below the baby’s ribcage, a cut is made, and the diaphragm hole is closed after the organs in the baby’s chest are guided back into the abdomen. The lungs can expand farther because of the extra room in the chest.
The hole is sealed with a GORE-TEX® patch or muscle flap for infants who have significant abnormalities or are born without a diaphragm at all. Doctors will keep a close eye on the patch’s health as your child develops to make sure it stays intact.
Surgery of unborn child:
The patient must normally be stabilized before surgery when there is an ADH. Since injuries are the primary cause of ADH, other issues including internal bleeding might arise. Consequently, the procedure should be performed as quickly as feasible
Depending on the severity of the problem and when it is discovered, congenital diaphragmatic hernias are treated differently. Your medical team assists you in making the best choice for you and your unborn child.
- Care before delivery:
Before the birth of your child, your healthcare team regularly monitors you. In order to monitor your baby’s health and growth, you normally undergo frequent ultrasounds and other procedures.
Fetoscopic endoluminal tracheal occlusion (FETO) is a newly developed therapy for severe CDH that is currently being researched.
.While you are still pregnant, your baby will have this procedure. The objective is to encourage the baby’s lungs to expand as much as possible before birth.
There are two ways to do FETO:
First method: The first surgery takes place early in the final few months of your pregnancy (third trimester). Your abdomen and uterus are cut in a tiny incision by the surgeon. A fetal endoscope is a special tube with a camera at one end that the surgeon inserts into your baby’s mouth and into the trachea. Your infant’s trachea is the location of a little balloon that is inflated.
Amniotic fluid, which is produced naturally by the uterus during pregnancy, enters and exits your baby’s lungs through the mouth. The balloon’s inflation maintains the amniotic fluid in the baby’s lung The fluid causes the lungs to expand, aiding in lung development.
Second method: You undergo a second surgery four to six weeks later. In order for your baby to be ready to breathe after birth, the balloon is taken out.
If labour begins before the balloon has been taken out and balloon removal with an endoscope is not possible, a specific delivery technique may be performed. Ex utero intrapartum therapy, or EXIT, is the name of this technique. With placental assistance, a C-section is used for delivery. This implies that until the umbilical cord is severed, your baby will continue to get oxygen through the placenta.
Placental support lasts until a breathing tube is put in and the balloon is removed, allowing a machine to take over breathing.
For some people, FETO might not be the best option. The outcomes of surgery are also not guaranteed. To determine if you could be a candidate for this operation, your medical team assesses both you and your unborn child. Talk to your team about the advantages and potential drawbacks for you and your unborn child.
- Care during delivery
Typically, you have a choice between a vaginal delivery and a C-section. Which approach is best for you will be decided by you and your healthcare practitioner.
- After-delivery care:
The medical staff assists you in making postpartum treatment plans that are tailored to your baby’s requirements. The newborn intensive care unit (NICU) will most likely provide care for your infant.
Your child could require a breathing tube. Your baby’s breathing assistance equipment is connected to the tube. The heart and lungs have more time to grow and develop as a result.
Extracorporeal membrane oxygenation (ECMO) is a therapy that may be necessary for infants with life-threatening lung conditions. ECLS (extracorporal life support) is another name for this. Your baby’s heart and lungs are able to rest and recover thanks to the ECMO machine, which performs its functions.
Your baby’s response to therapy and other variables will determine how long they require assistance breathing.
The majority of infants with CDH get surgery to seal the diaphragm hole. Depending on your baby’s health and other conditions, this procedure may be performed at a later date. Chest X-rays are typically used as part of the follow-up treatment to make sure the repair is still intact.
Your infant could require more support after leaving the hospital. This could also entail more oxygen. Thin plastic tubes with prongs that go into the nostrils or thin tubes attached to a mask worn over the nose and mouth are used to provide oxygen. To encourage growth and development, feeding assistance could also be required. Acid reflux and pulmonary hypertension are two disorders that can be treated with medication if they are related to CDH.
Regular follow-up visits with your child’s doctor might help you catch issues early.
Recovery After surgery for CDH
After the operation, your baby will recuperate and start to wean off the ventilator. Feedings of either breast milk or formula will gradually start through the NG or OG tube once the infant is ready. A speech therapist and lactation specialist will help your infant to start eating by mouth once the breathing tube is removed.
The severity of your baby’s CDH and how well they respond to therapy will determine how long they need to stay in the hospital from birth until release. Social workers and psychologists accompany family members through all the highs and lows they go through while newborns get this thorough medical treatment.
We will arrange your child for follow-up treatment in our Pulmonary Hypoplasia Program (PHP) once they have been released to go home. To monitor and address any CDH-related issues, your kid will see several specialists in one place. Find out more about the long-term care that our PHP team offers.
FAQs:
A birth deformity of the diaphragm is known as a congenital diaphragmatic hernia (CDH).
Bochdalek hernias are the most prevalent kind of CDH, and there are also Morgagni
hernias, diaphragm eventrations, and central tendon abnormalities of the diaphragm.
Breathing can be difficult for a newborn due to underdeveloped lungs shortly after
delivery. It is for this reason that a diaphragmatic hernia is a serious condition. There
are millions of tiny air sacs (alveoli) in healthy lungs.
Most frequently, CDH only affects one side of the diaphragm. On the left side, it occurs
more frequently. Mostly, blood arteries and lung tissue also fail to grow normally. It is unclear if the undeveloped blood vessels and lung tissue are a result of
the diaphragmatic hernia or vice versa.
Primary or patch closure of the diaphragm using an open, endoscopic, abdominal, thoracic,
or mix of these approaches is often required for surgical repair. There is growing
evidence that laparoscopic diaphragmatic hernia repair is a suitable and secure
alternative to open surgery treatment.
Hernias in the diaphragm are frequently referred to by their location. The colon or
omentum is more at risk of passing through a Morgagni hernia and into the thoracic
cavity when it is farther forward in location. The kidney is more at danger when a
Bochdalek hernia occurs since it is situated closer to the back.