Spinal Fusion Surgery
Table of Contents
What is spinal fusion?
Spinal fusion is a surgical process utilized to correct problems with the vertebral bones in the spine. It’s basically a welding process. The initial idea is to fuse together two or other vertebrae so that they merge into one, solid bone. This is done to exclude painful stirs or to restore stability to the spine.
Spinal fusion is surgery to connect two or further bones in any part of the spine. Connecting them prevents movement between them. averting movement helps to avert pain.
Spine surgery is generally advocated only when the doctor can pinpoint the source of pain. To do this, doctors may use imaging tests, similar X-rays, computed tomography( CT) reviews, and glamorous resonance imaging( MRI) reviews.
This procedure can be performed at any position in the spine( cervical, thoracic, lumbar, or holy) and prevents any movement between the fused vertebrae. There are numbers of types of spinal fusion and each approach involves the utilization of bone graft, either from the donor( allograft), patient( autograft), or artificial bone backups to assist the bones merging together. fresh hardware( screws, plates, or cages) is frequently used to hold the bones in place while the graft fuses the two vertebrae together. The placement of metal plates can be guided by robotics, navigation systems, or fluoroscopy.
In spinal fusion, extra bone is utilized to fill the gap that is generally present between the two separate vertebrae. When the bone heals, there’s no longer gap between them.
Vertebral interbody fusion; Posterior spinal fusion; Arthrodesis; Anterior spinal fusion; Spine surgery- spinal fusion; Low back pain- fusion; Herniated fragment- fusion; Spinal stenosis- fusion; Laminectomy- fusion; Cervical spinal fusion; Lumbar spinal fusion
The most common reason for spinal fusion is to reduce mechanical discomfort and pressure on the spinal cord or on the vertebrae that occur when a disc (the cartilage between two vertebrae) wears out (degenerative disc complaint). It’s also utilized as an optional procedure for total disc relief surgery( intervertebral disc arthroplasty), in case patient anatomy prevents replacement of the disc. Other usual diseases that are managed by fusion involve spondylolisthesis, spinal stenosis, spondylosis, scoliosis, spinal fractures, & kyphosis.
What are the Indications of spinal fusion?
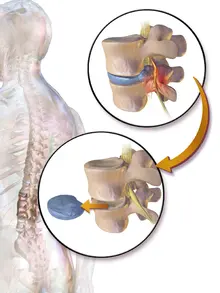
A herniated disc pressing on spinal nerves. Spinal fusion can be used to treat a variety of conditions affecting any position of the spine — lumbar, cervical, and thoracic. In general, spinal fusion is done to decompress and stabilize the spine. The topmost benefit appears to be in spondylolisthesis, while confirmation is less good for spinal stenosis.
The most common cause of pressure on the spinal cord/ nerves is degenerative disc complaints. Other usual causes include disc herniation, spinal stenosis, trauma, & spinal tumors. Spinal stenosis results from bony growths( osteophytes) or thickened ligaments that bring on the narrowing of the spinal canal over time. This leads to leg pain with increased activity, a condition called neurogenic claudication. Pressure on the nerves, as they exit the spinal cord( radiculopathy), causes pain in the region where the nerves originated( leg in lumbar pathology, arm in cervical pathology). In severe cases, this pressure can cause neurologic deficits, like apathy, tingling, bowel/ bladder dysfunction, and palsy.
Lumbar and cervical spinal fusions are more generally performed than thoracic fusions. Degeneration happens more constantly in these situations due to increased motion and stress. The thoracic spine is not that mobile, so most fusions are done because of trauma or defects like scoliosis, kyphosis, & lordosis.
Conditions, where spinal fusion might be considered, include the following
- Degenerative disc complaint
- Spinal disc herniation
- Discogenic pain
- Spinal tumor
- Vertebral fracture
- Scoliosis
- Kyphosis(e.g., Scheuermann’s complaint)
- Lordosis
- Spondylolisthesis
- Spondylosis
- Posterior rami syndrome
- spinal weakness or instability
- Other degenerative spinal conditions
- A condition that leads to instability of the spine
What are the risks of Spinal fusion?
Spinal fusion is a high-risk operation and complications can be serious, including death. In general, there is more risk of complications in an older population with elevated body mass index (BMI), other medical problems, poor nutrition, & nerve symptoms (numbness, weakness, bowel/bladder issues) before surgery. Complications also depend on the type or extent of spinal fusion surgery performed. There are three main time phases where complications typically occur:
During surgery
- Patient positioning on the operating table
- Blood loss
- Damage to nerves & surrounding structures during the procedure
- Insertion of spinal hardware
- Harvesting of bone graft which is autograft
Within a few days
- Moderate to severe postoperative pain
- Wound infections – risk factors involve diabetes, old age, obesity, smoking, & prior surgery
- Deep vein thrombosis (DVT)
- Pulmonary embolism (PE)
- Urinary retention
- Malnutrition
- Neurologic deficit
Weeks to years following surgery
- Infection – sources of bacterial bioburden that infiltrate the wound area are several, but the latest research highlights repeated reprocessing of implants prior to surgery & exposure of implants such as pedicle screws to bacterial infection in the “sterile region” during surgery as major risk factors.
- Deformity – loss of height, alignment, & failure of fusion
- Pseudarthrosis – nonunion between fused bone segments. Risk factors include tobacco usage, nonsteroidal anti-inflammatory drug use, osteoporosis, revision procedures, & decreased immune system.
- Adjacent segment disease –vertebrae that are above or below the level of the fused segments may degenerate as a result of changed biomechanical pressures or a patient’s propensity for gradual degenerative change.
- Epidural fibrosis – scarring of the tissue surrounding the spinal cord
- Arachnoiditis – inflammation of the thin membrane surrounding the spinal cord, commonly caused by infection or contrast dye.
How to prepare for spinal fusion surgery?
Typically, the preparation for spinal fusion is the same as other surgical techniques. It needs preoperative laboratory testing.
Before spinal fusion, you should inform the physician about any of the following:
- cigarette smoking, which might decrease your ability to heal from spinal fusion
- alcohol use
- any disease you have, including colds, the flu, or herpes
- any kind of prescription or over-the-counter medications you’re taking, including herbs & supplements
- You’ll want to discuss how the medications you’re taking should be utilized before & after the procedure. The doctor might give special instructions if you’re taking medications that could influence blood clotting. These include anticoagulants (blood thinners), such as warfarin, & nonsteroidal anti-inflammatory drugs, including ibuprofen and aspirin.
You’ll be given general anesthesia, so you’ll require to fast for at least eight hours previous to your procedure. On the day of surgery, drink only a sip of water to take any medications physician has recommended.
What is the procedure of spinal fusion surgery?
Surgeons perform spinal fusion by giving general anesthesia to the patient. There are many ways to do spinal fusion surgery. The approach the doctor selects depends on the patient’s complaint about where the bones need to be fused on the spine, the cause for the spinal fusion, & conceivably, the general health & body condition of the patient.
Lumbar & cervical spinal fusion have been done for decades. There are several different ways that may be used to fuse the spine. There are also different” approaches” surgeons can take to reach the spine.
There are numerous types of spinal fusion ways. Each approach varies depending on the position of the spine and the place of the compressed spinal cord/ nerves. A bone graft or artificial bone overlay is inserted between the vertebrae after the spine has been decompressed to aid in the healing process. In general, fusions are done moreover on the anterior( stomach), posterior( back), or both sides of the spine. present, utmost fusions are supplemented with hardware( screws, plates, rods) because they’ve been shown to have advanced union rates than non-instrumented mixtures. Minimally invasive ways are also getting more popular. These ways use advanced image guidance systems to fit rods and screws into the spine through lower incisions, allowing for lower muscle damage, blood loss, infections, pain, and length of stay in the medical center. The ensuing list gives examples of common types of fusion ways performed at each level of the spine
Anterior Approach to the cervical spine
Cervical spine:
Anterior cervical discectomy and fusion( ACDF)
Anterior cervical corpectomy and fusion
Posterior cervical decompression and fusion
Thoracic spine:
Anterior decompression and fusion
Posterior instrumentation and fusion – Sublaminar wiring, pedicle screw-rod systems, transverse process hooks, pedicle, and vertebral body plate systems, among others, can be used to hold the spine in place.
Lumbar spine:
Posterolateral fusion is a bone grafting between the transverse processes in the spine. Metal rods are used to hold the spine in place with the help of screws.
Interbody Fusion is a graft where the entire intervertebral disc between vertebrae is removed and a bone graft is placed in the space between the backbone. A plastic or titanium device might be placed between the vertebra to maintain spine alignment & disc height. The types of interbody fusion are
- Anterior lumbar interbody fusion( ALIF) – the disc is penetrated from an anterior abdominal incision
- Posterior lumbar interbody fusion( PLIF) – the slice is penetrated from a posterior incision
- Transforaminal lumbar interbody fusion( TLIF) – the disc is penetrated from a posterior incision on one side of the spine
- Transpsoas interbody fusion( DLIF or XLIF) – the disc is penetrated from an incision through the psoas muscle on one side of the spine
- Oblique side lumbar interbody fusion( OLLIF) – the disc is penetrated from an incision through the psoas muscle diagonally
Stabilization rods are used after spinal fusion surgery.
Generally, the process involves the following
Getting to the spine. To get to the bones being fused, the surgeon makes a cut in one of three places. Cut from the posterior, these cuts are in the neck or back straight over the spine or on either side of the spine. To get to the spine from the anterior, the surgeon cuts into the stomach area or throat.
Getting the bone graft ready. Bone grafts come from a bone bank or from the body of the person having the surgery, generally from the pelvis. occasionally surgeons use mortal-made material rather than bone grafts. In autograft, the surgeon cuts near the pelvic bone eliminates a little segment of it, and also closes the cut.
Fusion. To connect the spinal bones, the doctor places the bone graft material in between the bones. The doctor might insert rods, screws, or metal plates to assist hold the bones tightly until the bone graft fuse.
The right procedure for you’ll depend on the nature and position of your disease.
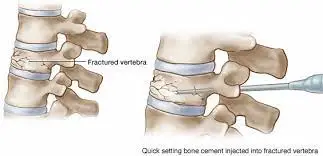
Bone Grafting
All spinal fusions use some kind of bone material, called a bone graft, to assist promote the fusion. Generally, small particles of bone are placed into the space between the vertebrae to be fused.
A bone graft is primarily utilized to stimulate bone healing. It increases bone production & helps the vertebrae combine together into a solid bone. sometimes larger, solid pieces are also used to give structural support to the vertebrae.
In history, a bone graft gathered from the patient’s pelvis was the only option for increasing the material demanded to fuse the vertebrae. This kind of graft is called an autograft. Harvesting a bone graft requires a fresh incision during the operation. It lengthens surgery & can cause elevated pain after the operation.
still, the surgeon may harvest your bone from the location of the decompression and use it as the graft, If you’re having a decompression procedure. This kind of graft is called an original autograft. The bone is basically recycled; it’s moved from where it’s entrapping nerves to the region the surgeon wants to fuse.
One choice for harvesting a bone graft is an allograft, which is from cadaver bone. An allograft is generally acquired through a bone bank. These tissues are largely processed, and the chance of infection or disease from this tissue is really low.
Today, many artificial bone graft materials have also been developed:
Demineralized bone matrices (DBMs). Calcium is eliminated from cadaver bone to create Demineralized bone matrices. Without the mineral, the bone can be turned into a gel-like consistency. Demineralized bone matrices are commonly combined with other grafts and might contain proteins that assist in bone healing.
Bone morphogenetic proteins (BMPs). These most powerful synthetic bone-forming proteins found a solid fusion. They are approved by the U.S. Food & Drug Administration for usage in the spine in certain circumstances. Autografts might not be needed when Bone morphogenetic proteins are used.
Synthetic bone. Synthetic bone grafts are made up of calcium or phosphate materials and are frequently called “ceramics.” They are the same in shape and consistency as autograft bone.
the surgeon will discuss with the patient the type of bone graft material that will work best for their condition and procedure.
Immobilization:
After bone grafting, the vertebrae require to be held in place to assist the fusion progress.
In many cases, surgeons will use plates, screws, & rods to help hold the spine still. This is called internal fixation and might increase the rate of successful healing. With the extra stability from internal fixation, most patients are able to move sooner after surgery. the surgeon might advocate that you wear a brace to assist protect the welding process.
What happens after Spinal fusion surgery?
A medical center stay of two to three days is generally needed following spinal fusion. Depending on the location and extent of your surgery, you may witness some pain and discomfort but the pain can generally be controlled well with drugs.
After you go home, communicate with the doctor if you exhibit signs of infection, similar as
- reddishness, tenderness, or swelling
- Wound drainage
- Shaking chills
- Fever advanced than100.4 F( 38 C)
It might take a few months for the affected bones in the spine to heal and fuse together. the doctor might advocate that patients wear a brace for a time to keep their spine aligned rightly. Physical remedies can educate you on how to move, sit, stand, and walk in a manner that keeps your spine properly aligned.
After surgery, you’ll feel some pain. This is a natural process of the recovery phase. Your doctor and nurses will work to reduce your pain, which can help you recover from surgery briskly.
Following surgery, medications are usually administered for momentary pain relief. many kinds of drugs are present to assist manage pain, including nonsteroidal anti-inflammatory medicines, opioids, & original anesthetics. doctor might use a combination of these medications to enhance pain relief, as well as minimize the need for opioids.
Be apprehensive that although opioids help relieve pain after surgery, they’re a narcotic and can be addicting. Opioid dependence and overdose have become critical public health issues in the U.S. It’s important to use opioids only as directed by your doctor and to stop taking them as soon as your pain begins to enhance. Inform the doctor if your pain has not started to improve within many days later surgery. However, talk to your surgeon before your procedure so you can plan your postoperative pain regimen together If you’re formerly taking anesthetics previous to surgery.
Surgery doesn’t always improve pain, and in some cases, can make it worse. still, in some people, surgery can be effective for severe pain that doesn’t get better with other treatments.
nevertheless, you’ll probably still have some pain subsequently, If you had habitual back pain before surgery. Spinal fusion is doubtful to take away all your pain and other symptoms.
It’s hard to prognosticate which people will improve and how important relief surgery will give, indeed when using MRI reviews or other tests.
Losing weight and learning to exercise increases your chances of feeling better.
unborn spine problems are possible after spine surgery. After spinal fusion, the zone that was fused together can no longer bend. thus, the spinal column above and below the fusion is more likely to be stressed when the spine moves and may bring about problems latterly on.
During your stay, you will meet with physical and occupational therapists who’ll educate you on how to get out of bed, into a president, and walk again. Before your doctor sends you home, you will have spinal X-rays to make sure the fusion is doing OK. You will return to have stitches removed in about 10 days. After that, you’ll have follow-up appointments, generally in about 4 to 6 weeks, 6 months, 12 months, and 24 months.
Recovering from back surgery takes commitment and work. It could take 6 months to a time for your back to completely heal. You need to stick with physical therapy after you leave the clinic. the doctor will tell you how frequently you need to go. For the first six months, adhere to these recommendations to protect your back as you get better. Whenever possible, limit your twisting, bending, and heavy lifting to no more than a gallon of milk! So go ahead and leave the dishes & laundry to your partner or kiddies.
Recovery generally involves both restrictions on certain activities and rehabilitation training. Restrictions after surgery majorly depend on surgeon preference. A typical timeline for common restrictions after lumbar fusion surgery is listed below
- Walking – utmost people are out of bed and walking the day after surgery
- Sitting – can begin at 1 to 6 weeks later surgery
- Lifting – it’s generally recommended to avoid lifting until 12 weeks
- Driving – generally can start at 3 – 6 weeks
- Return to sedentary work – generally between 3 to 6 weeks
- Return to homemade work – in 7 – 12 weeks
- Rehabilitation after spinal fusion isn’t obligatory. There’s some proof that it improves functional status & low back pain so some surgeons might recommend it.
Contraindications
Bone morphogenetic protein (rhBMP) should not be used in any type of anterior cervical spine fusion surgery, mainly with anterior cervical discectomy and fusion. There are reports of this therapy causing soft tissue swelling, which in turn can cause life-threatening complications because of difficulty swallowing and pressure on the respiratory tract.
What are the Complications of spinal fusion?
As with any surgery, there are risks related to spinal fusion. the doctor will discuss each of the risks with you before your procedure & will take specific measures to help avoid potential complications. Complications of spinal fusion include:
- Infection. Antibiotics are routinely given to the patient before, during, & frequently after surgery to lessen the risk of infections.
- Bleeding. Some amount of bleeding is expected, but this is not typically significant. It is not commonly necessary to donate blood before spinal fusion.
- Pain at the graft site. A small percentage of patients will feel persistent pain in the bone graft region.
- Recurring symptoms. Some patients might experience a recurrence of their original symptoms. There are different causes for this. If original symptoms recur, inform the doctor so that he or she can determine what is causing your symptoms.
- Pseudarthrosis. This is a disease in which there is not adequate bone production to create a solid fusion. Patients who smoke are more prone to develop pseudarthrosis. Other causes include diabetes & older age. Moving too early before the bone is able to begin fusing might also outcome in pseudarthrosis. If this occurs, a second surgery might be needed.
- Nerve damage. It is possible that nerves or blood vessels might be injured during these surgeries. This complication is very rare.
- Blood clots. Another uncommon complication is the generation of blood clots in the legs. These pose significant danger if they dislodge and travel to the lungs.
Warning Signs:
It is important that you carefully follow any instructions from a doctor relating to the warning signs of blood clots & infection. These complications are most prone to occur during the first few weeks after surgery.
Blood clots. Warning signs of a possible blood clot involve:
- Swelling in the calf, ankle, or foot
- Tenderness or redness, which might extend above or below the knee
- Pain in the calf
- sometimes, a blood clot will travel through the bloodstream and might settle in the lungs. If this happens, you may feel sudden chest pain and shortness of breath or coughing. If you experience any of these symptoms, you should inform a doctor immediately. If you cannot reach the doctor, have someone take you to the hospital emergency room or call 911.
Infection. Infection following spine surgery takes place very rarely. Warning signs of infection include:
- Redness, tenderness, & swelling around the wound edges
- Persistent drainage from the wound
- Pain or tenderness
- Shaking chills
- Elevated temperature, generally above 101°F if taken with an oral thermometer
- If any of these symptoms take place, you should contact the doctor or go to the nearest emergency room immediately.
What is the result of spinal fusion surgery?
Spinal fusion surgery significantly works for managing broken bones, reshaping the spine, or making the spine more stable. But results of the research are mixed when the cause of the back or neck pain is not clear. Spinal fusion frequently works no better than nonsurgical treatments for back pain with a cause that is not clear.
Even when spinal fusion relieves symptoms, it does not prevent future back pain. Arthritis causes much back pain. Surgery doesn’t heal arthritis.
Having a spine that doesn’t bend in places puts more strain on the regions around the fused part. As a result, those regions of the spine might break down faster. Then the spine might require added surgery in the future.
Physiotherapy treatment
preoperative treatment of spinal fusion
This is the proper timing for evaluating functional outcomes & psychological support. This is possible with patient education, which includes:
- Stabilization-based exercises
- Postoperative precautions
- Bed mobility and transfers
- Initial postoperative exercises
- Gait training with any necessary assistive devices
- Donning and doffing any required braces
- Wound care
- General Overview & Prognosis of the postoperative rehabilitation process
- general checking of the facility & operating room along with meeting with patients who have undergone the same surgery might also be useful to decrease patient anxiety during the surgery & hospital experience.
The physical therapist should know about the process of surgery.
Note: During a posterior fusion, the multifidus is retracted from the spine. This partially tears the spinal nerves and denervates the multifidus. If an anterior fusion also has been done, then a midline skin incision will be evident & the abdominal muscular incision is lateral. The incision passes via the obliques, also partially denervating them. For this reason, the therapist should teach the patient the proper way to recruit the transverse abdominous, multifidi, & pelvic floor muscles and watch for any substitution patterns to promote proper spinal stabilization.
- ROM (Range of motion)
- Posture
- Balance
- Gait
- Strength
- Body mechanics
- Specific functional tasks
- Specific Neurological examination
- The diagnosis shouldn’t include Lumbar ROM or hip flexor mobility, especially at the first stages of rehabilitation.
post-operative treatment of spinal fusion
Phase I
1 to 5 days after surgery (inpatient) & up to 6 Weeks
Most patients are suggested for physical therapy anywhere between 4 to 7 weeks after their discharge from the hospital.
Physical therapy management during this phase contains educating patients on the proper way to bed transfers, dress and do other self-care activities, & walk (with the use of a walker for the first 1 or 2 days).
Light transverse abdominous and pelvic floor contractions to start to practice them in different positions.
The therapist can also instruct on basic and easy neural mobilization for the lumbosacral plexus nerves.
Patients and their families should leave the hospital with an understanding of the home care needed until they start their outpatient physical therapy.
Phase II
6 to 10 weeks after surgery
Cases should begin to approach normal activities while the therapist controls
cases should be sluggishly working up to 30 twinkles of exercise and physical exertion at least 5 days a week.
They can embark on a lightweight- training program, avoiding exercises that erroneously load the lumbar chine but making sure to include some exercise for the lumbar paraspinal and other muscles that attach to the thoracodorsal fascia.
Common restrictions are no lifting lesser than 10lb. and no overhead lifting.
Goals:
- Achieve good body mechanics during ADL
- Protect the surgical point from infection and mechanical stress
- nerve root mobility at the involved degrees
- Control pain and inflammation
- Begin a stabilization and reconditioning program
- enhance scar and encircling soft tissue mobility
- Treat restrictions of thoracic, UEs, and LEs that can lead to further strain on the lumbar spine
Body mechanics education:
bed mobility
pushing and pulling
lifting and carrying
Hip hinge approach
See Injury Prevention and Body Mechanics
Nerve root gliding manners:
Patients should extend the knee while lying supine with the spine in a neutral position and the hip flexed to a 90 ° angle. When tension is encountered, the therapist helps the patient work the knee or ankle gently back and forth, gradationally increasing the ROM. This stretch may bring on increased symptoms during the stretch, which should resolve instantly after relaxing.
Pain management:
Prescribed drugs and ice.
Ultrasound should not be applicable over a healing bony fusion.
Patients with severe pain complications can try using a home transcutaneous electrical nerve stimulation( TENS) unit or interferential unit (IFT).
Incisional pain can be anticipated to diminish gradually over 6 to 8 weeks.
Strength and Reconditioning:
Co-contraction of the transverse abdominous, multifidus, and pelvic floor muscles with and without using pressure biofeedback( BFB). See lumbar stabilization
Abdominal breathing
Abdominal bracing and marching in a supine are good exercises to start strengthening the trunk. Before bracing is initiated, it’s stylish to make sure the patient can isometrically contract the transverse abdominous, multifidi, and pelvic floor muscles.
Exercises are recommended to be rehearsed in sitting, standing, and quadruped.
General strength and conditioning exercises should also be initiated during this phase of rehab after it’s cleared by the physician and the patient demonstrates applicable stabilization. Examples of exercises would include
- Wall squats and sit to stand
- Half lunges
- Step ups and step downs
- Walking
Cardiovascular reconditioning( using a stair climber, brisk walking, and pool exercises once the incision is unrestricted)
Care should be taken when starting further vigorous strengthening activities because it’s recommended that the patient be suitable to use the applicable stabilization muscles during factors of the exercise before doing the full exercise.
Hip flexor stretching should only start after the allowance of the surgeon. stretching should be very gentle & only pull to the point the patient can brace to avert lumbar movement.
one of the most stressful movements in the lumbar spine is rotation, which causes a shearing effect across the disc. Since the thoracic spine is designed to allow further rotation, the limited movement may increase strain on the lumbar spine during twisting movements. The PT can use homemade mobilization ways to increase thoracic spine mobility
Examples of other exercises( performed while bracing) initiated in the after stages of phase II include the following
- Bridging
- Heel lifts
- Superman( avoiding lumbar extension)
- Side pulls( light resistance with the blessing of the surgeon)
- The seated upright rowing machine
- Scapular depression( avoid defying further than 40 of body weight)
- Push-ups standing and leaning into the wall
- Stair climber
- Upper body ergometer(UBE)
What the therapist is making an effort to develop at this stage is not very important to muscle power as a kinesthetic sense of the muscles & their part in guarding the spine. thus the proper form of each exercise should be emphasized.
Scar and soft tissue mobility:
Through soft tissue mobilization manners.
Phase III
11 to 19 weeks after surgery
Goals:
Return to work
continue to advance/progress the exercise program,
practice specific skills programs,
initiate a resistance training program
They usually return to work on a part-time basis or with modified responsibilities.
the patient should be independent with self-care jobs and also with a moderately challenging home exercise program.
More demanding stabilization exercises like side planks and half-and-full front planks could be used.
The previous trunk stabilization exercises should be progressed within the patient’s tolerance with modifications according to the patient’s condition.
It is not suggested to do complex weight lifting tasks but to focus on light free weight activity & machine-based exercises that allow the patient to do them with proper posture, technique, & bracing.
Patients should be taken care of with overhead lifting because of the axial load & compressive forces placed on the spine.
Endurance and cardiovascular exercises should also be progressed at this stage & start to progress gradually.
For some individuals, it might be advised to do more cardiovascular or resisted exercises in an aquatic rehabilitation environment.
At this stage, the expectation is that pain continues to diminish and be at the least level. However, if pain persists and the surgeon reported an absence of physical explanation, then the therapist should reinforce the functional improvements & minimize the importance of pain as a marker of improvement.
Phase IV
20 weeks to 1 year after surgery
Goals:
Restore pre-injury status
Continue home program of conditioning & stabilization
Progressing to full restoration of their before-injury level of function and being independent with conducting their past home & gym program.
They should have a good grasp of not only the exercises and physical activity needed to reach their goals but also ways to modify those activities.
Patients with fusions often develop complications at the level above or below the fusion. For these reasons, the patient should know that spine care is now a lifetime concern and must be maintained through regular exercise & good mechanics during every daily activity.
Later in this phase (and with clearance from the surgeon) they might start agility and sport-specific drills, such as running, cutting, & jumping. If a more comprehensive weight training program is called for it should be again geared to the specific exercise faced by the patient.
FAQs
The recovery period for spinal fusion surgery differs significantly from patient to patient, but the average time period is between 3 & 6 months before the patient is back to their daily routine; traveling, working, & even exercising with more freedom & less pain than they could prior to the surgery.
After surgery, the patient can expect her back to feel stiff and sore. the patient might have trouble sitting or standing in one position for a very long time. It might take four to six weeks to get back to doing normal activities, such as simple housework. It might take 6 months to a year for the back to get better completely.
Spinal fusion is a surgical approach to joining 2 or more bones of the spine together permanently.
No, there are no hard & fast age criteria for spinal surgery. Because both old age patients and young patients can have problems with the spine, age is not the primary choosing factor in whether or not spinal surgery is a choice.
The spinal fusion technique permanently fuses the targeted vertebrae of the spine. This process also permanently eliminates all movements at the affected segment. So, patients do experience permanent restrictions in their mobility, such as an inability to twist, bend, & lift heavy objects.
Disc replacement surgery includes replacing the painful disc in the spine with an artificial disc. The aim of artificial disc replacement surgery is to preserve the normal movement of the spine (unlike fusion, which eliminates movement at the painful spinal segment).




One Comment