Upper Respiratory Tract Infection
- An upper respiratory infection harms the upper part of your respiratory system, including your sinuses and throat. Upper respiratory infection symptoms involve a runny nose, sore throat, and cough.
- Treatment for upper respiratory infections often involves rest, fluids, and over-the-counter pain relievers. Infections commonly go away on their own.
Table of Contents
What is a respiratory infection?
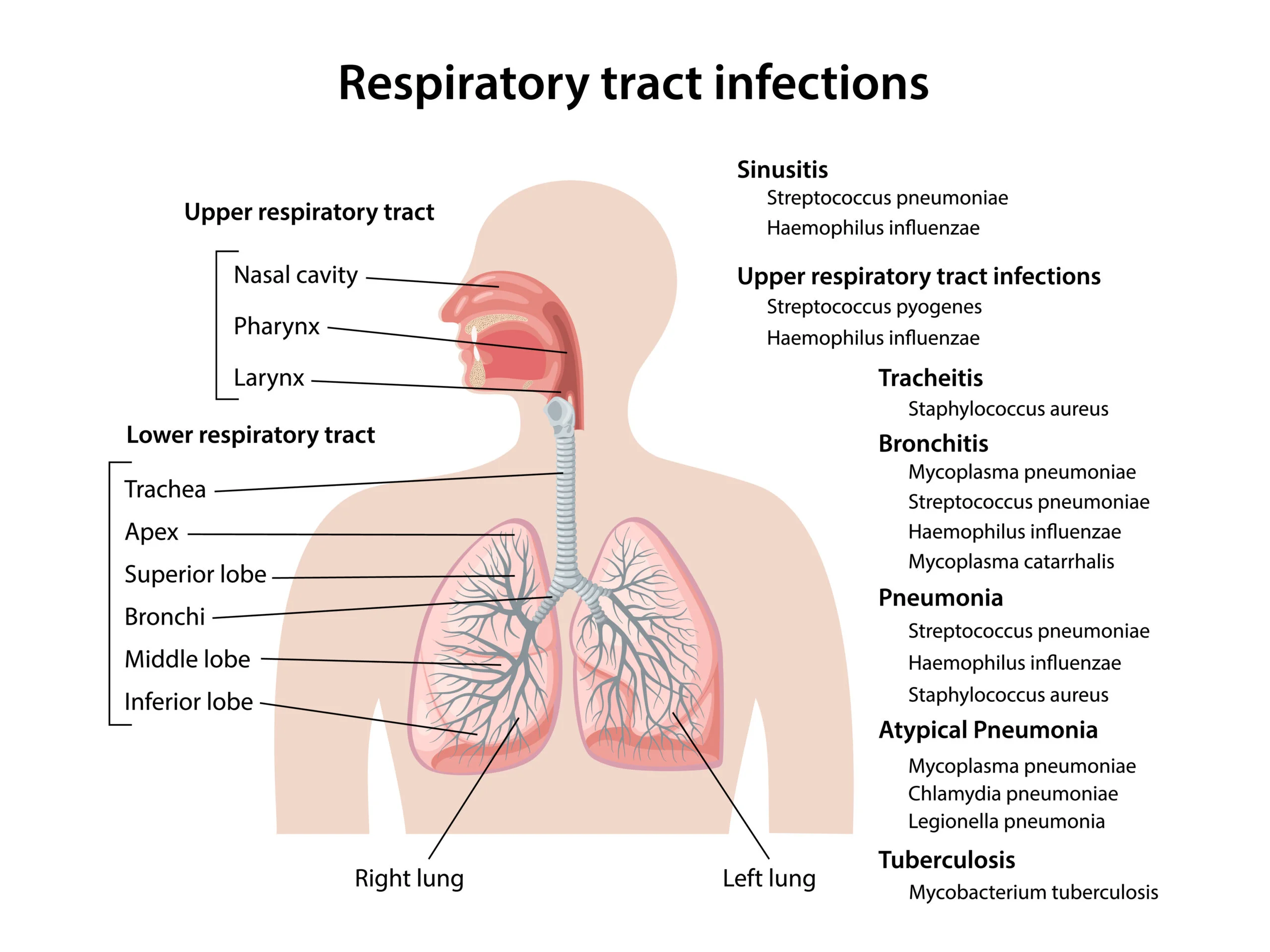
- A respiratory tract infection harms the respiratory system, the part of your body responsible for breathing. These infections can harm your sinuses, throat, lungs, or airways. There are 2 types of respiratory infections:
- Upper respiratory infections,
- Lower respiratory infections.
What is an upper respiratory infection?
These infections harm your sinuses and throat. Upper respiratory infections include:
- Common cold
- Epiglottitis
- Laryngitis
- Pharyngitis (sore throat)
- Sinusitis (sinus infection).
What is a lower respiratory infection?
A lower respiratory infection harms the airways and lungs. In general, lower respiratory infections last longer and are more severe. These infections involve:
- Bronchitis, a lung disease that causes coughing and fever
- Bronchiolitis, a lung infection that mostly harms young children
- Chest infection
- Pneumonia.
What causes upper respiratory infections?
- You get an upper respiratory disease when a virus (or bacteria) enters your respiratory system. For example, you might touch an infected area or shake hands with a person who’s sick. It may enter your body when you touch your mouth, nose, or eyes. The germs from your hands irritate and infect your body.
Who is at risk for upper respiratory infections?
- These infections are usual, and anyone can catch one. But certain groups of people are more at risk of catching infections. Children are at a high risk since they are sometimes with other children who may be carrying a virus. Children may also wash their hands less sometimes than adults. Plus, they are more likely to put their fingers in their eyes, nose, and mouth, allowing the germs to spread easily.
- People who have heart or lung problems are also at higher risk of acquiring an upper respiratory infection. Those who have weak immune systems (due to another disease) may get more serious infections.
How are upper respiratory infections diagnosed?
- Your healthcare provider (doctor) may diagnose the infection based on a physical exam and your symptoms.
- They will look in your nose, ears, and throat and listen to your chest to examine your breathing. You often do not need other tests.
If your provider (doctor) is concerned you may have a lung infection or another infection, you may need a:
- Lung (chest) X-ray
- Lung CT scan
- Lung (pulmonary) function test to look at how your lungs are working
- Nasal swab
- Throat swab
- Sputum test, when you cough up certain sputum (phlegm from your lungs) for examination.
Are upper respiratory infections contagious?
- Yes, upper respiratory infections are transmissible. They pass from person to person through a respiratory drop or hand-to-hand contact. People who have an upper respiratory infection can move it to others through:
- Sneezing or coughing without cowling their nose and mouth. This sprays microbes into the air. Other people can breathe in that germ-filled drop.
- Sneezing or coughing inside their hand and then touching someone else’s hand. The drop is now on the other person’s hand. When that person touches their or nose, mouth, or eyes, the infection enters their body.
What are the symptoms of upper respiratory infections?
You may get symptoms, involving:
- Cough
- Fever
- Hoarse voice
- Fatigue and loss of energy
- Red eyes
- Runny nose
- Sore throat
- lymph nodes swelling on the sides of your neck
How long do upper respiratory infections last?
- Upper respiratory infections typically last 1 to 2 weeks. Most of the time, they move away on their own.
- Over-the-counter pain medications can assist you to feel better. Make sure you drink plenty of fluids to remain hydrated.
- If your symptoms last longer than 2 weeks, talk to your healthcare provider.
- You may have another condition that is causing the symptoms, like pneumonia or bronchitis.
What is the common cold?
- The usual cold refers to at least 200 different viruses that cause a cold. Colds sometimes go away on their own.
Colds can:
- Occur at any age.
- Have a wide range of symptoms.
- Spread through direct contact with respiratory secretions, such as saliva, mucus, or phlegm.
- It last about seven to 10 days, though a cough can last up to three weeks.
- Lead to complications like ear infections, eye infections, sinus infections, and pneumonia.
Treating a cold can assist you to feel better:
- Use acetaminophen (Tylenol) if you have body aches and a fever.
- Stay hydrated. Make sure to drink a lot, especially fluids like water, tea, and broth.
- Get plenty of rest.
What is epiglottitis?
- The epiglottis is the top area of your trachea, your breathing tube. It sits far back in your mouth, at the below of your tongue. Epiglottitis is when the epiglottis gets inflamed. This condition can be severe.
- If the epiglottis swells from inflammation, it can stoke your airway. You may have a problem breathing. If you think you or a loved one has epiglottitis, get medical help immediately.
Symptoms of epiglottitis involve:
- Difficulty breathing or swallowing.
- Fever.
- Severe sore throat.
- Epiglottitis needs treatment at a hospital or medical facility. Healthcare providers (doctors) first need to check your oxygen levels and protect your airway. You may require supplemental oxygen if your oxygen levels are too low. You may also require:
- IV fluids to retain you hydrated until you can swallow without problems.
- Antibiotics, if your provider (doctor) thinks you may have a bacterial infection.
- Steroids to reduce swelling.
What is laryngitis?
- Your larynx is your voice box. Laryngitis is when the larynx becomes inflamed. Typically, a virus infects the upper airways, leading to laryngitis. The important symptom of laryngitis is a voice change. You may:
- Become very hoarse.
- Only be able to ask at a low volume.
- Lose your voice entirely.
- You may also get a fever, have difficulty swallowing, and have a sore throat. Your healthcare provider (doctor) can discuss treatment options with you. You most likely who not need antibiotics since the cause is usually viral, not bacterial. To treat laryngitis:
- Rest your voice. Try not to speak. If you need to say, talk in a low voice rather than a whisper. Whispering can irritate your larynx.
- Drink plenty of extra fluids.
- Breathe in steam.
- Use cough suppressants.
What is pharyngitis?
Pharyngitis is known as a sore throat. It is usually caused by a virus. Sometimes, bacteria known as group A Streptococcus can cause a type of sore throat called strep throat. Strep throat is more usual in children between ages 5 and 15. Symptoms of a sore throat may involve:
- Severe throat pain.
- Difficulty swallowing and speaking.
- Ear pain.
- Tender lymph nodes in the neck.
- Swollen, red tonsils.
- Your healthcare provider (doctor)may do a throat swab (strep test) to find out if it is a bacterial infection. If the test is positive for strep throat, you will take a course of antibiotics, such as penicillin.
If the test is negative, your provider (doctor) may recommend:
- Over-the-counter pain relievers, such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs), help with throat pain.
- Gargling with warm salt water to soothe your throat.
- A single dose of a steroid helps with symptoms.
What is a sinus infection?
Sinusitis, or a sinus infection, is a usual problem. It happens when your sinuses become inflamed. Sinuses are hollow spaces located below the bones of your face. You have sinuses in your:
- Cheeks.
- Behind your forehead and eyebrows.
- On the sides of your nose bridge.
- Beyond your nose, in front of your brain.
- Most of the time, viruses infect the sinuses, causing inflammation.
You may feel or have:
- Postnasal drip is when you feel mucus dripping into your throat.
- Green mucus from your nose.
- Stuffiness or congestion.
- Pain when you press on your face, especially on the bones right under your eyes.
- Bad breath.
- Cough.
- Fatigue.
- Fever.
- Headaches.
- If you have these symptoms lasting longer than 7-10 days, or if your symptoms worsen later 5-7 days, you may have a bacterial infection. Please see your healthcare provider (doctor) for a diagnosis. Antibiotics may be required to clear up a sinus infection in this case
What are common respiratory infections in children?
- Respiratory infections are usual in children. They occur more often when children are in daycare or school. Siblings can infect each other as well.
- It is normal for kids to have up to six respiratory infections per year. And they can last up to two (2)weeks. Most of the time, at-home remedies are enough to assist your child feel better until the virus passes.
- Yet if you have any concerns, see your child’s healthcare provider. Certain infections need antibiotics. And if your child has worrying symptoms, such as a high fever or difficulty breathing, contact your provider (doctor) or go to the emergency room.
Common respiratory infections among children involve:
- Bronchiolitis is an infection that causes wheezing and coughing.
- Common cold, which usually involves a runny nose, cough, and feeling run-down.
- Croup, which causes a hoarse cough that sounds such as a seal.
- Ear infections, when bacteria infect the middle ear, causing pain.
- Pink eye is an eye infection, usually bacterial, that can cause a thick yellow discharge from the eye.
- Sinus infection is when viruses or bacteria infect and inflame the sinuses, causing pain.
- Sore throat, which can be viral or bacterial (strep throat).
Can antibiotics treat upper respiratory infections?
- Most of the time, microbes cause upper respiratory infections. Viruses do not respond to antibiotics. You can most likely cure the symptoms at home through pain relievers, rest, and drinking fluids.
- If you have a bacterial infection, such as strep throat, you will take antibiotics. Penicillin or amoxicillin are sometimes prescribed for strep throat.
When should I see a healthcare provider for an upper respiratory infection?
If you have any of these symptoms, contact your healthcare provider or seek medical assistance:
- Lack of consciousness,
- High fever (higher than 103 F),
- Rapid breathing or difficulty breathing,
- Frequent, serious coughing, may come with vomiting,
- Wheezing, a high-pitched whistling sound when you breathe out,
- Dizziness.
- Retractions, are when you see a deeper outline of your ribcage or ribs than you normally do. (This sign may be more obvious in children).
- Stridor is a harsh raspy vibrating when you breathe in that sometimes sounds like a seal. (Stridor is more usual in children than adults).
What is the common cold?
The common cold refers to at least 200 various viruses that cause a cold. Colds often go away on their own. Colds can:
- Occur at any age,
- Have a wide range of symptoms,
- Spread through direct contact with respiratory secretions, such as saliva, mucus, or phlegm,
- It last about 7 to 10 days, though a cough can last up to three weeks,
- Lead to complications like ear infections, eye infections, sinus infections, and pneumonia.
Treating a cold can assist you to feel better:
- Utilize acetaminophen (Tylenol) if you have body aches and fever,
- Stay hydrated. Make sure to drink a lot, especially fluids like water, tea, and broth,
- Get plenty of rest.
What is epiglottitis?
- The epiglottis is the top area of your trachea, your breathing tube. It sits a long way back in your mouth, at the base of your tongue. Epiglottitis is when the epiglottis gets infectious. This condition can be severe. If the epiglottis swells from inflammation, it can check your airway. You may have trouble breathing. If you think you or a loved one has epiglottitis, get medical assistance right away.
Symptoms of epiglottitis involve:
- Difficulty breathing or swallowing
- Fever
- Severe sore throat.
- Epiglottitis needs treatment at a hospital or medical facility. Healthcare providers first require you to check your oxygen levels and protect your airway. You may need supplemental oxygen (O2) if your oxygen levels are too low.
You may also require:
- IV fluids to retain you hydrated until you can swallow without problems.
- Antibiotics, if your provider (doctor) thinks you may have a bacterial infection.
- Steroids to decrease swelling.
What is laryngitis?
- Your larynx is your voice box. Laryngitis is when the larynx flatters inflamed. Commonly, a virus infects the upper airways, leading to laryngitis. The important symptom of laryngitis is a voice change.
You may:
- Become very hoarse
- Only be able to talk at a decreased volume
- Lose your voice entirely.
- You may also get a fever, have hard swallowing and have a sore throat. Your healthcare provider (doctor) can discuss treatment options with you. You most likely who not need antibiotics since the cause is usually viral, not bacterial.
To treat laryngitis:
- Rest your voice. Try not to speak. If you do need to speak, talk in a decreased voice rather than a whisper. Whispering can irritate your larynx.
- Drink plenty of fluids.
- Breathe in steam.
- Utilize cough suppressants.
What is pharyngitis?
- Pharyngitis is also called a sore throat. It is usually caused by a virus. Sometimes, bacteria called group A Streptococcus can cause a type of sore throat known as strep throat. Strep throat is more usual in children between ages 5 and 15.
Symptoms of a sore throat may involve:
- Severe throat pain
- Difficulty swallowing and speaking
- Ear pain
- Tender lymph nodes in the neck
- Swollen, red tonsils.
- Your healthcare provider (doctor) may do a throat swab (strep test) to find out if it is a bacterial infection. If the test is positive for strep throat, you will take a course of antibiotics, such as penicillin.
If the test is negative, your provider (doctor) may recommend:
- Pain relievers, like acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs), to help with throat pain
- Gargling with hot salt water to soothe your throat
- A single dose of a steroid to assist with symptoms.
Who is at risk for acute upper respiratory infection (URI)?
- The usual cold is the most typical cause of doctor visits in the United States. URIs extend from one person to another through aerosol droplets and direct hand-to-hand contact.
The riskTrusted Source goes up:
- when someone who’s sick sneezes or coughs without covering their nose and mouth, & droplets containing the viruses are sprayed into the air
- when people are in a closed-in part or crowded conditions, like in hospitals, institutions, schools, and daycare centers,
- if you have a medical condition, like asthma or allergic rhinitis,
- if you have a weakened immune system, involving cystic fibrosis and HIV
- in those who smoke,
- in those who use corticosteroids, like prednisone.
What are the symptoms of acute upper respiratory infection (URI)?
- A runny nose, nasal congestion, sneezing, and cough are the hallmark symptomsTrusted Source of URIs (upper respiratory infections). Symptoms are caused by inflammation of the mucous membranes in the upper respiratory tract (URT).
Other symptoms involve:
- fever
- fatigue
- headache
- pain during swallowing
- wheezing.
How is acute upper respiratory infection diagnosed?
- Most people with URIs (upper respiratory infections) know what they have. They may visit a doctor for comfort from symptoms. Most URIs (upper respiratory infections) are diagnosed by looking at a person’s medical history and doing a physical exam.
Tests that may be used to diagnose URIs (upper respiratory infections) are:
- Throat swab: Rapid antigen detection can be used to diagnose group A beta-hemolytic strep fastly.
- Lateral neck X-rays: This test may be ordered to rule out epiglottitis if you have a problem breathing.
- Chest X-ray: The doctor may order this test if they guess pneumonia.
- CT scans: This test may be utilized to diagnose sinusitis.
What is a sinus infection?
Sinusitis, or a sinus infection, is a usual problem. It occurs when your sinuses become inflamed. Sinuses are hollow spaces located back to the bones of your face. You have sinuses in your:
- Cheeks
- Behind your forehead and eyebrows
- On the sides of your nose bridge
- Beyond your nose, in the anterior of your brain
- Most sometimes, viruses infect the sinuses, causing inflammation.
You may feel or have:
- Postnasal drip is when you feel mucus dripping into your throat.
- Green mucus from your nose.
- Stuffiness or congestion.
- Pain when you press on your face, especially on the bones right below your eyes.
- Bad breath.
- Cough.
- Fatigue.
- Fever.
- Headaches.
- If you have these symptoms lasting longer than 7 to 10 days, or if your symptoms worsen after 5 to 7 days, you may have a bacterial infection. Please see your healthcare provider (doctor) for a diagnosis. Antibiotics may be required to clear up a sinus infection in this case.
What are common respiratory infections in children?
- Respiratory infections are usual in children. They occur more often when children are in daycare or school. Siblings can infect one another as well.
- It is normal for kids to have up to six respiratory infections per year. And they can last up to two (2) weeks. Most of the time, at-home remedies are enough to assist your child feel better until the virus passes.
- But if you have any concerns, see your child’s healthcare provider (doctor). Certain infections need antibiotics. And if your child has worrying symptoms, like a high fever or difficulty breathing, contact your provider (doctor) or go to the emergency room.
Common respiratory infections among children involve:
- Bronchiolitis, an inflammation that causes wheezing and coughing,
- Common cold, which usually includes a runny nose, cough, and feeling run-down,
- Croup, which causes a hoarse cough that sounds such as a seal,
- Ear infections, when bacteria infect the middle ear, causing pain,
- Pink eye is an eye infection, commonly bacterial, that can cause a thick yellow discharge from the eye,
- Sinus infection is when viruses or bacteria infect and inflame the sinuses, causing pain,
- Sore throat, which can be viral or bacterial also known as strep throat.
Is the flu an upper respiratory infection?
- Influenza, or the flu, is not considered an upper respiratory infection. That is because it is systemic — it affects more than one system in the body. It usually harms the upper and lower respiratory system. The cold and flu have the alike symptoms.
- The flu sometimes comes along with symptoms such as achiness and a high temperature, in addition to upper respiratory symptoms such as a cough and sore throat. See your healthcare provider (doctor) if you think you may have the flu. You can take steps to cure the flu, such as getting the flu vaccine every year.
Is pneumonia an upper respiratory infection?
- Pneumonia is a lung infection. Symptoms can resemble those of an upper respiratory tract infection. You may have a serious cough that brings up phlegm (mucus), shortness of breath, and chest pain. See your healthcare provider (doctor) if you think you may have pneumonia.
How can I prevent upper respiratory infections?
Retain you and your family healthy. Take steps to cure upper respiratory infections:
Practice good hygiene:
- Wash hands, especially previous eating or preparing food,
- Sneeze and cough into your arm or a tissue and wash your hands after.
Live a healthy lifestyle:
- Avoid contact with people who are sick
- Drink plenty of fluids
- Get enough sleep
- Stop smoking.
See your provider:
- Retain up with routine checkups and immunizations.
- Ask your provider if you should get the pneumococcal vaccine, which cures pneumonia.
- Call your healthcare provider (doctor) if you have symptoms lasting longer than two weeks, a high fever, or any other concern.
Should I worry about an upper respiratory infection?
- Most of the time, these inflammations go away on their own. You will likely make a full recovery. However, certain higher-risk groups should take extra precautions when it comes to upper respiratory infections.
These infections can be great dangerous for:
- Children, especially babies
- Older adults
- People with immune system disorders.
- If you are in a high-risk group and get a cold or another respiratory infection, contact your healthcare provider (doctor).
How is acute upper respiratory infection treated?
- URIs (upper respiratory infections) are mostly treated for the relief of symptoms. Certain people benefit from the use of cough suppressants, expectorants, vitamin C, and zinc to decrease symptoms or shorten the duration.
Other treatments involve:
- Nasal decongestants can increase breathing, but they may be less effective with repeated use and can cause rebound nasal congestion.
- Steam inhalation and gargling with salt water are safe ways to get relief from URI (upper respiratory infection) symptoms.
- Analgesics like acetaminophen (Tylenol) and NSAIDs can assist reduce fever, aches, and pains.
Physiotherapy Treatment
Aims of Chest Physiotherapy
The purpose of chest physiotherapy are:
- To facilitate the transfer of retained or profuse airway secretions.
- To optimize lung compliance and the ventilation-perfusion ratio/ increase gas exchange.
- To reduce the work of breathing.
- Increase exercise tolerance
- Cure secondary complications.
The Physiological Mechanism of Airway Clearance
- Normal Clearance: A normal clearance needs an open airway, a functional mucociliary escalator, and an effective cough. Airways commonly are kept open by structural support mechanisms and kept clear by the proper function of their ciliated mucosa. The normal human bronchial tree is lined by a thin (5 micrometers) layer of mucus which is motioned over the airway surface by the mucociliary escalator. The ciliated epithelium which lines the airways is responsible for the constant flow of mucus over the airway surface to the upper respiratory tract. The mucus is moved via a coordinated movement of ciliary motion toward the trachea and larynx, where excess secretions can be swallowed or expectorated.
- An effective cough is a should for normal airway clearance.
- Cough is one of the most main protective reflexes. By ridding the bigger airways of excessive mucus and foreign matter, the cough assists the normal mucociliary clearance and assists ensures airway patency. There are four (4) distinct phases to a normal cough: irritation, inspiration, compression, and expulsion.
- Abnormal Clearance: The flow of air through the tracheobronchial tree and its interactivity with the mucus lining is complex because of the branching geometry of the airways, collapsible airway walls, constantly changing the velocity of airflow, and differing viscoelastic properties of mucus. This physiology of flow in the liquid line airway is known as a two-phase gas-liquid flow. In endobronchial diseases, the mucus layer may exceed five mm in thickness and ciliary clearance becomes ineffective. Two-phase flow now becomes a main mechanism of clearance, and at a particular combination of airflow, mucus viscosity, and thickness there is a very strong gas-liquid interaction which 1st exacerbates the pressure decrease and then detaches liquid from the airway wall. this conducts to the narrowing of the lumen of the tube causing a much greater resistance, thus affecting airway clearance.
- One of the mechanisms by which cough harms sputum clearance in endobronchial diseases is two phases of gas-liquid flow: the transfer of momentum and energy from the high-speed flow of air to the mucus that lines the bronchi. The high transmural pressure produced during cough conducts to dynamic compression of the airway inhibiting mucociliary clearances. Thus, the forced expiratory technique (FET) was introduced to resolve this problem.
Classification
- There are different physiotherapy treatments incorporated within chest physiotherapy. Chest physiotherapy techniques can be categorized as conventional, modern, or instrumental techniques based on making research.
Conventional Techniques
- Conventional chest physiotherapy is also called traditional chest physiotherapy. It was advocated 1st in 1915. It includes manual handling techniques to facilitate mucociliary clearance. Postural drainage along with percussion and vibration ( PDPV) was before widely named Chest Physiotherapy.
- After, coughing exercises and forced expiratory techniques (huffing) were included within it. Postural drainage along with percussion and vibration (PDPV) with huffing has shown an effective outcome.
- It can be self-administered or performed with the assistance of other people (a physiotherapist, parent, or caregiver). Postural drainage along with percussion and vibration (PDPV) works better if applied with bronchodilator therapy.
Postural drainage
- Postural drainage (PD) includes positioning a person with the assistance of gravity to aid the normal airway clearance mechanism. Postural drainage positioning differs based on specific segments of the lungs with a large number of secretions. Postural drainage is the drainage of secretions, by the effect of gravity, from 1 or more lung segments to the central airways (where they can be removed by a cough or mechanical aspiration).
- Each position consists of placing the select lung segment(s) superior to the carina. Positions should commonly be held for 3 (three) to 15 minutes (longer in special situations). Standard positions are adjusted as the patient’s condition and tolerance permit.
- Previous to determining the postural drainage position, it is very main to auscultate the lungs and identify the lung segments where added sound (Crepitus, Ronchi) is heard. Postural drainage (PD) can be facilitated with percussion and vibration in the postural drainage (PD) position.
Percussion
- Percussion is referred to as cupping, clapping, and tapotement. The purpose of percussion is to intermittently put kinetic energy into the chest wall and lungs.
- This is accomplished by rhythmically striking the thorax with a cupped hand or mechanical device straight over the lung segment(s) being drained.
Vibration
- Vibration includes the application of a fine tremorous action (manually performed by pressing in the direction that the ribs and soft tissue of the chest move during expiration) over the draining area.
- In this technique, a fast vibratory impulse is transmitted through the chest wall from the flattened hands of the therapist by isometric alternate contraction of the forearm flexor and extensor muscles, to loosen and dislodge the airway secretions.
Coughing
- Coughing includes directed coughing and different assisted coughing techniques.
Forced Expiratory Technique (FET)
- Forced expiratory techniques include diaphragmatic inspiration, relaxing the scapulohumeral region, and expiring forcefully from mid to decrease lung volumes whilst maintaining an open glottis (“huffing” exercises).
- It is more operative than coughing.
Indication of Conventional techniques
Postural drainage positioning
- Inability or reluctance of the patient to exchange body position. (eg, mechanical ventilation, neuromuscular disease, drug-induced paralysis).
- Poor oxygenation allianced with the position (eg, unilateral lung disease).
- Potential for or presence of atelectasis.
- Presence of artificial airway.
Postural drainage along with percussion and vibration (PDPV)
- Difficulty clearing secretions with expectorated sputum production bigger than 25-30 mL/day (adult).
- Evidence or suggestion of kept secretions in the presence of an artificial airway.
- Presence of atelectasis caused by or douted of being caused by mucus plugging.
- Diagnosis of diseases like cystic fibrosis, bronchiectasis, or cavitating lung disease
- Presence of foreign body in the airway.
- Patient with profuse sputum or with central consolidation.
Frequency
- Positioning: Ventilated and critically ill patients: as required with the goal of once each hour or every other hour as tolerated, around the clock. Less acute patients should be turned every 2 (two) hours as tolerated.
Postural drainage along with percussion and vibration (PDPV)
- In critical care patients, involving those on mechanical ventilation, PDT should be performed every 4 to every 6 hours as indicated. PDT orders should be re-evaluated at least every 48 hours based on assessments from personal treatments.
- In voluntarily breathing patients, frequency should be determined by assessing patient response to therapy.
- Acute care patient orders should be re-evaluated based on patient response to therapy at least every 72 hours or with an exchange of patient status.
- Domiciliary patients should be re-evaluated every 3 (three) months and with a change of status.
Modern techniques
- Over the years, so many additional noninvasive clearance methods have been developed to augment this traditional approach. Modern techniques use a different flow through breath control to mobilize secretions.
- It involves an active cycle of breathing and autogenic drainage.
Active cycle of breathing technique
- Active cycle of breathing technique (ACBT) is an active breathing technique performed by the patient and can be used to mobilize and clear extra pulmonary secretions and generally improve lung function.
- It has a series of three main phases: Breathing control, Thoracic expansion, and Forced expiratory technique (FET).
Autogenic drainage
- Autogenic drainage is a diaphragmatic breathing pattern used by patients with respiratory illnesses (e.g., cystic fibrosis, bronchiectasis) to clear the lungs of mucus and other secretion.
- Different techniques are used, all of which combine positive reinforcement of deep breathing and voluntary cough suppression for as long as possible previous evacuating the airways of mucus.
Instrumental techniques
Instrumental techniques such as non-invasive ventilation have been considered utilized as adjunct therapy to airway clearance and to provide respiratory support. Usual instrumental techniques are:
- Positive expiratory pressure (PEP): There are different positive expiratory pressure devices that provide resistance to expiration through a mouthpiece or facemask, followed by forced expirations. The inhalation is at tidal volume (TV), and the expiration is slightly active against devices. These devices assist to remove secretions by increasing functional residual capacity and thus enhancing collateral ventilation and removing secretions from collapsed airways. Certain of the devices are Flutter, Acapella, lung flute, etc.
- Continuous Positive Airway Pressure: created by exhalation against a constant opening pressure, this produces positive end-expiratory pressure (PEEP). Continuous positive airway pressure (CPAP) can also be delivered by commercially available pressure drivers. These generally need tightly fitting nasal prongs or a Continuous positive airway pressure (CPAP) face mask. Bubble Continuous positive airway pressure (CPAP) can be used in a low-resource environment and in the pediatric population. It involves an interface (nasal cannula), inspiratory tubing, and expiratory tubing immersed in an underwater battle system.
- High-Frequency Chest Wall Oscillation (HFCWO): an airway clearance technique in which external chest wall oscillations are applied to the chest utilizing an inflatable vest that wraps around the chest. These machines produce vibrations at variable frequencies and intensities, helping to loosen thin mucus and separate it from airway walls.
- HFCWO includes an inflatable jacket that is attached to a pulse generator by hoses that mechanically enable the equipment to perform at variable frequencies (5–25 Hz). The generator conveys air through the hose, which causes the vest to inflate and deflate rapidly. The vibrations not only separate mucus from the airway walls but also assist move it up into the large airways. Commonly, it is paused during the 20- to 30-minute HFCWO treatment every 5 minutes to cough out loosened mucus that has moved into the large airways.
- Intrapulmonary Percussive Ventilation (IPV): designed to promote mobilization of bronchial secretions and involve efficiency and distribution of ventilation, providing intrathoracic percussion and vibration and an alternative system for the delivery of positive pressure to the lungs. Each Intrapulmonary Percussive Ventilation (IPV) session lasted fifteen minutes and was performed twice a day (morning and afternoon). Intrapulmonary percussive ventilation (IPV) uses a pneumatic device to deliver a series of pressurized gas minibursts at rates of 100 to 225 cycles per minute to the respiratory tract, by a mouthpiece. The duration of each and every percussive cycle is manually controlled by a thumb button. During the cycle, continuous PAP is maintained in the airway. It incorporates a nebulizer for the delivery of the aerosol.
Assessment of need and outcome
The following should be assessed together to establish a requirement for chest physiotherapy:
- Excessive sputum production.
- Effectiveness of cough.
- History of pulmonary problems resulted successfully with PDT (eg, bronchiectasis, cystic fibrosis, lung abscess).
- Reduced breath sounds or crackles or rhonchi suggest secretions in the airway.
- Change in vital signs.
- Unusual chest x-ray consistent with atelectasis, mucus plugging, or infiltrates.
- Deterioration in arterial blood gas (ABG) values or oxygen saturation.
The following can be used as a result tool to determine the effectiveness of treatment:
- Change in sputum production.
- Change in breath sounds of lung fields.
- Patient subjective response to therapy.
- Change in vital signs.
- Change in a chest x-ray.
- Change in arterial blood gas (ABG) values or oxygen saturation.
- Change in ventilator variables.
- Change in Modified borg scale- dyspnea level.
- Change in Peak Expiratory Flow Rate.
Contraindications of Conventional Techniques
Positioning
All positions are contraindicated for:
- Intracranial pressure (ICP) > 20 mm Hg
- head and neck injury until stabilized (Absolute)
- Active hemorrhage with hemodynamic instability (Absolute)
- Recent spinal surgery (ex, laminectomy) or acute spinal injury
- Acute spinal injury or active hemoptysis
- Empyema
- Bronchopleural fistula
- Pulmonary edema associated with congestive heart failure
- Large pleural effusions
- Pulmonary embolism
- Aged, confused, or anxious patients who do not allow position changes
- Rib fracture, with or without flail chest
- Surgical wound or healing tissue.
Trendelenburg position is contraindicated for
- Intracranial pressure (ICP) > 20 mm Hg
- Patients in whom improved intracranial pressure is to be avoided (eg, neurosurgery, aneurysms, eye surgery)
- Uncontrolled hypertension
- Distended abdomen
- Oesophageal surgery
- Latest gross hemoptysis related to current lung carcinoma treated surgically or with radiation therapy
- Uncontrolled airway at threat for aspiration (tube feeding or recent meal)
- Back Trendelenburg is contraindicated in the presence of hypotension or vasoactive medication.
External Manipulation of the Thorax
In addition to the contraindications listed
- Subcutaneous emphysema
- Recent epidural spinal infusion or spinal anesthesia
- Current skin grafts, or flaps, on the thorax
- Burns, open wounds, and skin contaminations of the thorax
- Currently placed transvenous pacemaker or subcutaneous pacemaker (particularly if mechanical devices are to be used),
- Suspected pulmonary tuberculosis
- Lung contusion
- Bronchospasm
- Osteomyelitis of the ribs
- Osteoporosis
- Coagulopathy
- Complaint of chest-wall pain.
Complications
- Hypoxemia
- Bronchospasm
- Increased Intracranial Pressure
- Acute Hypotension during Procedure
- Pulmonary Hemorrhage
- Pain or Injury to Muscles, Ribs, or Spine
- Vomiting and Aspiration
- Bronchospasm
- Dysrhythmias.
How can acute upper respiratory infections be prevented?
- The best protection against URIs (upper respiratory infections) is frequent handwashing with soap and water. Washing your hands decreases exposure to secretions that can spread infection.
Other strategies involve:
- Avoiding being in close touch with people who are sick.
- Wiping down objects such as remote controls, phones, and doorknobs that may be touched by people in the house who have a URI (upper respiratory infection).
- Covering your mouth and nose if you are sick.
- Staying home if you’re sick.
What complications can happen from upper respiratory infections?
- Severe complications can involve respiratory failure when there is too much carbon dioxide in your blood. The infection could also spread to another part of your body, such as your brain or heart.
- If you have any concerns about your symptoms, call your healthcare provider (doctor). If you are having difficulty breathing or other worrisome symptoms.
NOTE
- Upper respiratory infections are usual. Anyone can get an upper respiratory tract infection, though they happen more frequently among children. Upper respiratory tract infection symptoms include coughing, runny nose, sneezing, and throat pain.
- You may get a fever. These infections commonly go away on their own. You can utilize pain relievers to feel better.
- Make sure to drink plenty of fluids and need rest. If you are concerned about your symptoms, or they do not go away after two weeks, contact your healthcare provider (doctor).
FAQs
You get an upper respiratory infection when a virus (or bacteria) enters your respiratory system. For example, you might touch an infected surface or shake hands with a person who’s sick. You then touch your mouth, nose, or eyes. The germs from your hands enter and infect your body.
You can expect the symptoms of your cold or upper respiratory infection to last 14 to 21 days. A dry hacking cough may continue for up to three or four weeks. To help you recover: Drink more fluids
Complications of acute respiratory infection are extremely serious and can result in permanent damage and even death. They include respiratory arrest, which occurs when the lungs stop functioning. respiratory failure, a rise in CO2 in your blood caused by your lungs not functioning correctly.
The most common virus is the rhinovirus. Other viruses include the influenza virus, adenovirus, enterovirus, and respiratory syncytial virus.
To make yourself as comfortable as possible when you have a cold, Langer suggests trying to:
Drink plenty of fluids.
Eat chicken soup.
Rest.
Adjust your room’s temperature and humidity.
Soothe your throat.
Use saline nasal drops.
Take over-the-counter cold and cough medications.
The recommended first-line treatment is a 10-day course of penicillin. Erythromycin can be used in patients who are allergic to penicillin. Amoxicillin, azithromycin (Zithromax), and first-generation cephalosporins are appropriate alternatives.
A few warning signs that your cold has progressed from a viral infection to a bacterial infection are:
Symptoms lasting longer than 10–14 days.
A fever higher than 100.4 degrees.
A fever that gets worse a couple of days into the illness, rather than getting better.
White pus-filled spots on the tonsils.
An upper respiratory infection, or a URI, is a contagious infection in the upper respiratory tract, which includes the bronchi, larynx, pharynx, throat, and nose. Upper respiratory infections can be caused by viruses or bacteria. (In case you’re wondering, COVID-19 is considered a lower respiratory infection).
a cough – you may bring up mucus (phlegm) and sneeze. a stuffy or runny nose. a sore throat.