Triangular Fibrocartilage Complex (TFCC)
Table of Contents
Introduction
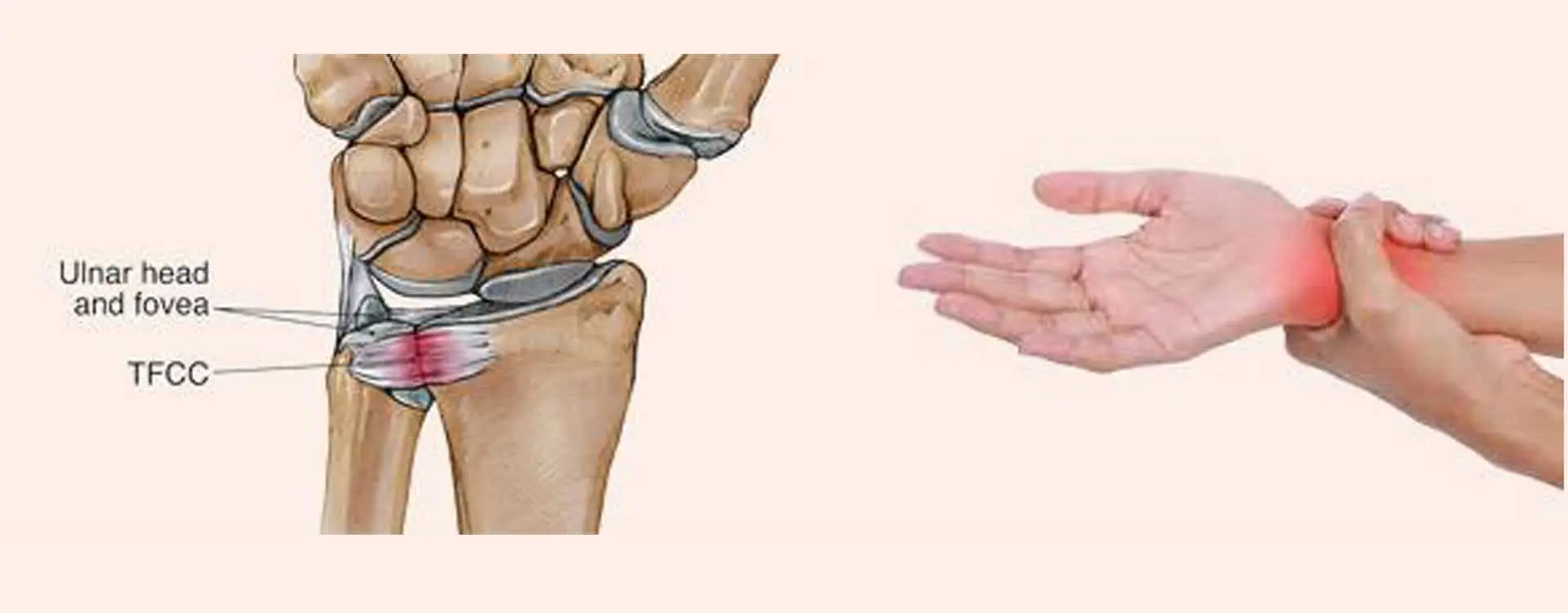
Between the lunate, triquetrum, and ulnar head lies a load-bearing structure termed as the triangle fibrocartilage complex (TFCC). The TFCC’s role is to stabilize the ulnar side of the wrist.
The TFCC is endangered by both acute and long-term degenerative damage. Positive ulnar variation and forced ulnar deviation are linked to TFCC damage. Patients who have had a TFCC injury will experience ulnar-sided wrist pain, which may be accompanied by clicking or tenderness at a specific spot between the pisiform and the ulnar head. 39 to 84% of instances of distal radius fractures are found to also have TFCC.
While arthroscopy is the gold standard for diagnosis, MRI imaging is beneficial as a preliminary diagnostic technique. In addition to surgical care, conservative therapies like rest, NSAIDs, and corticosteroid injections are also an option.
Injury to the TFCC has a usually positive prognosis.
What is Normal Triangular Fibrocartilage (TFCC)?
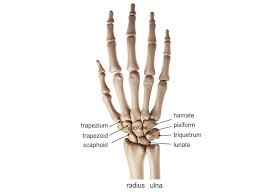
The TFC resembles the temporomandibular joint disk in shape; it is a fibrocartilaginous biconcave disk with an asymmetric bow-tie shape. Two thin bands of TFC tissue join the TFC to the ulnar styloid process on the medial side, where it is located in the ulnocarpal space. Hyaline cartilage exists between the TFC and the radius at its radial attachment, which should not be confused with a detached or torn TFC.
The distal radioulnar joint’s articular cartilage and the cartilage along the ulnar portion of the radius are adjacent, and this is where the TFC connects. The amount of ulnar variation is inversely correlated with the TFC thickness. To put it another way, patients with positive ulnar variance have TFCs that are thinner, making them more likely to rip, whereas patients with negative ulnar variance have TFCs that are thicker.
The coronal MR scans show the TFC the best. Regardless of the pulse sequence, it may have a diffusely low signal strength or, due to asymptomatic myxoid degeneration, a substance with an intermediate signal intensity.
Clinically relevant anatomy:
The distal radioulnar joint and the radiocarpal wrist are separated by the triangular fibrocartilage complex, which is an articular and cartilaginous structure. The TFCC consists of the articular disc, its meniscal counterpart, the ulnar, dorsal, and volar radioulnar ligaments, and the extensor carpi ulnaris.
Origin: Medial edge of distal radius
Insertion: Base of ulnar styloid
Vascular supply: the central disc is avascularized, and peripheral blood vessels penetrate the edges of the TFCC.
The function of the TFCC: Stabilizer of the head of the distal radioulnar joint (the volar part of the TFCC resists dorsal displacement of the ulna and is rigid in pronation, and the dorsal part of the TFCC resists volar displacement of the ulna and is rigid in supination). Promotes ulnar carpal stability
Structure
Anatomy of the triangular fibrocartilage complex (TFCC)
- Triangular fibrocartilage disc
The distal ulna’s pole is home to the triangular fibrocartilage disc (TFC), an articular disc. It is triangular in shape with a biconcave body, with the perimeter being thicker than the center. Chondroid fibrocartilage, a kind of tissue frequently found in constructions that can withstand compressive loads, makes up the TFC’s thin middle part. This middle region is usually nonexistent, or at least extremely thin to the point of being translucent. While the center region of the TFC lacks a blood supply, the periphery is extensively vascularized.
This disc is attached by thick tissue to the base of the ulnar styloid and by thinner tissue to the edge of the radius, just proximal to the radiocarpal articular face.
- Ligaments:
The TFCC is situated between the lunate and triquetrum of the proximal carpal row on the ulnar face of the wrist joint. It has an elongated triangular shape, with the apex pointing at the radius bone.
The complex, formed by multiple ligamentous and fibrocartilaginous components, consists of:
- Triangular fibrocartilage disc proper and triangular ligament
- Radioulnar ligaments:
- Volar radioulnar ligament
- Dorsal radioulnar ligament
- Ulnocarpal ligaments:
- Ulnotriquetral ligament
- Ulnolunate ligament
- Ulnocapitate ligament
- Meniscal homologue
- The tendon sheath of the extensor carpi ulnaris and the ulnar collateral ligament
Radioulnar ligaments:
The radioulnar ligaments( RULs) are the foremost stabilizers of the distal radioulnar joint( DRUJ). The palmar and dorsal radioulnar ligaments are the two RULs.
The ulna styloid and the fovea, a groove that divides the ulnar styloid from the ulnar head, are the two discrete and different places where these ligaments insert after emerging from the distal radius medial border. Each ligament has a deep component and a superficial component. The ulna styloid is directly inserted by the outside components. The deep components fit more anteriorly into the fovea, right next to the distal ulna’s dome’s articular surface.
The ligaments have a good circulatory supply to promote healing and are made of longitudinally oriented lamellar collagen to resist tensile pressure.
Ulnocarpal ligaments:
The ulnolunate and ulnotriquetral ligaments make up the ulnocarpal ligaments (UCLs). They arise from the ulnar styloid and insert into the carpal bones of the wrist; the ulnolunate ligament inserts into the lunate bone, and the ulnotriquetral ligament into the triquetrum bone. These ligaments prevent the dorsal migration of the distal ulna. Supination causes the ulnar styloid to migrate away from the carpal bones on the volar side, making them tight.
Function:
The primary functions of the TFCC are:
- The distal radius’ articular surface is extended to cover the ulna head.
- Ulnocarpal joint load transfer and partial load absorption
- Gives a strong yet flexible connection between the distal radius and ulna, allowing forearm motion. The ulnar section of the carpus is also supported by it.
The following activities are performed by the triangular fibrocartilage complex:
- The distal radioulnar joint’s primary stabilizer
- Supporting buttress for the proximal carpal row
- Allowing for the passage of 20% of the force—the remainder being transmitted through the radiocarpal joint—of the axial load from the carpus to the ulna.
Load transmission:
The TFCC is vital in load transmission across the ulnar aspect of the wrist. Compressive pressures are transmitted and absorbed by the TFC.
The amount of stress transmitted via the distal ulna is influenced by the ulnar variance. This ulnar variance is exactly related to the load transmission. About 20% of the load is transmitted in neutral ulnar variance. The load across the TFC is reduced by ulnar variation that is negative. Supination causes this because the radius displaces laterally on the ulna, resulting in a negative ulnar variance. With positive ulnar variance, it is reversed. Then, there is an increase in the load that is transmitted across the TFC. Pronation causes the positive ulnar variance to occur.
Rotation:
RULs Supination
The DRUJ is significantly stabilized by the TFCC. Together with the proximal radioulnar joint, the DRUJ regulates forearm rotation. The distal radius and distal ulna are connected, maintaining the congruency of the DRUJ. The RULs of the TFCC are primarily responsible for this attachment. Through the joint’s arc of rotation, these ligaments provide support.
It is debatable how the TFCC affects pronation and supination. Some writers (Schuind et al.) came to the conclusion that the palmar and dorsal TFCC fibres contract during supination and pronation, respectively.
In reality, both sides are correct because the RULs are made up of two ligaments, the superficial and deep ligaments, each of which has two parts. The deep dorsal and superficial palmar ligaments are contracted during supination, preventing the ulna from being translated palmarily. The superficial dorsal and deep palmar ligaments are tightened and stop the ulna from translating dorsally in pronation, which is the opposite of supination.
Clinical significance
Due to its intricate anatomical structure and many functions, the TFCC is significantly vulnerable to damage and ageing.
The majority of TFCC traumatic injuries are caused by the application of an extension-pronation force to an axial-load wrist, such as in a fall on an extended hand.
Traumatic injuries can also result via dorsal rotation, such as when a drill binds and rotates the wrist rather than the bit.
A distraction force applied to the volar forearm or wrist may potentially cause injury. Finally, patients with distal radius fractures frequently discover rips of the TFCC.
Not all TFCC perforations and flaws are painful. Lesions in the TFCC are correlated with aging, but many of these flaws are asymptomatic. The majority of patients with positive ulnar variance have these abnormalities.
Degenerative TFCC tears are brought on by prolonged and severe loading through the ulnocarpal joint. Ulnar impaction syndrome includes these tears as one of its symptoms.
Despite the fact that spontaneous deterioration of the ulnocarpal joint occurs frequently, it must be recognized. In cadaveric examinations, TFCC perforations and chondromalacia of the ulnar head, lunate, and triquetrum were seen in 30% to 70% of the patients. Less degenerative alterations were seen in cases with ulnar-negative variance.
TFCC lesions are classified according to Palmer:
The Palmer classification, which classifies TFCC lesions into traumatic and degenerative types, is the most well-known categorization system. This classification just serves to anatomically describe tears; it does not suggest a course of action or offer a prognosis.
Class 1: Traumatic
Class 1A: Central perforation
Class 1B: Ulnar avulsion, with or without a styloid fracture, is a Class 1B injury.
Class 1C: Distal avulsion (from carpus)
Class 1D: Radial avulsion (with or without sigmoid notch fracture) is an injury
Class 2: Degenerative (ulnar impaction syndrome)
Class 2A: TFCC wear
Class 2B: TFCC wear with ulnar head chondromalacia and/or lunate
Class 2C: Ulnar head chondromalacia and TFCC hole in the lunate
Class 2D: Lunotriquetral ligament perforation, lunate and/or ulnar head chondromalacia, and TFCC perforation
Class 2E: TFCC perforation with ulnocarpal arthritis, perforation of the lunotriquetral ligament, and lunate and/or ulnar head chondromalacia.
Therapeutic Presentation:
- Patients often complain of ulnar wrist discomfort, which typically gets worse with activities.
- Patients who have had a TFCC injury often experience pain or discomfort on the ulnar side of the wrist, frequently just above the ulnar styloid. However, some individuals also have widespread pain in the wrist as a whole.
- Patients with TFCC injuries frequently also experience oedema, a weakening of their grip, instability, and grinding or clicking noises (crepitus) when using their wrists. Additionally, there can be clicking, instability, or grip brittleness.
- Rest can ease discomfort, but exercise can exacerbate it, especially when the wrist is rotated (supinated or pronated) when the hand is moved sideways in the ulnar direction.
- Some aspects of history can arise in connection with particular sports, such as baseball-specific acute injuries caused by forced wrist extension during a head-first slide or when a hitter tries to hit an inside pitch but gets “jammed.”
- Because of the stress the swing imposes on the wrist, baseball players are prone to long-term injury. Even if these athletes don’t have positive ulnar variance, they can nevertheless have TFCC injuries.
- In gymnastics, overuse injuries to the TFCC can result from both support skills and hanging components. This region may become inflamed with repeated weight bearing (both compressive and tensile), and the anchoring wrist ligaments may develop tendonitis or tendonosis (commonly misinterpreted as a wrist sprain).
Diagnosis
Anamnesis: Falls on pronated outstretched arms, rotational injuries to the forearm, axial load trauma to the wrist, or distraction injuries to the wrist in the ulnar direction can all lead to injuries to the TFCC. However, not every patient is able to recall when a prior trauma happened.
Physical examination of the body:
Palpation: The extensor carpi ulnaris (ECU) and flexor carpi ulnaris (FCU), distal to the ulnar styloid and proximal to the pisiform bone, are the optimum places to palpate the TFCC.This area’s soreness could be indicative of a TFCC lesion.
Piano key symbol: Dorsal DRUJ instability may result in an outstretched ulna head that is pressable. Once you relax the pressure, it will automatically spring back into place, just like a piano key.
The DRUJ stress test involves holding the wrist in a pronated or supinated posture while the doctor tries to move the distal ulna in a dorsal and volar direction. Painful laxity signals RUL pathology and DRUJ instability.
Ulnar grind test: The wrist is held in dorsiflexion while the forearm is fixed. The doctor next rotates and deviates the wrist in the ulnar direction while applying an axial load. During this provocation technique, discomfort and crepitations point to arthritis or DRUJ instability.
Imaging
A central triangular fibrocartilage complex (TFCC) rip as seen under the microscope
- X-ray: There are two ways to take X-rays of the wrist: posterior-anterior (PA) and lateral. Radiographs are helpful for diagnosing or excluding osteoarthritis, a positive ulnar variance, and potential bone fractures. X-rays cannot show the TFCC, regardless of its state.
- MRI: Using the results of a thorough physical examination and an MRI, a doctor can determine the TFCC’s status. Nevertheless, false-positive and false-negative MRI results occur often.
- Arthrography: A dye is injected into the wrist joint during arthroscopy. The dye will leak from one joint compartment to another if there is a TFCC lesion.
- Wrist arthroscopy: Even though wrist arthroscopy is an invasive diagnostic method, it is still the most reliable means to locate TFCC abnormalities.
There are other potential explanations for ulnar-sided wrist discomfort aside from a TFCC injury.
Treatment:
Conservative (nonsurgical) therapy is the first line of treatment for both traumatic and degenerative TFCC lesions with a stable DRUJ. For a period of four to six weeks, patients may be instructed to keep their wrist and forearm immobile by donning a temporary splint or cast. As a result of the immobility, scar tissue can form and aid in TFCC healing. Also available for pain treatment are oral NSAIDs and corticosteroid joint injections. After immobilization or surgery, patients can benefit from occupational and physical therapy. In moderate cases, wrist support straps can be utilized to compress and reduce mobility in the area.
- Rest, activity adjustment to eliminate the injury’s stimulus, use of ice, and immobilization in a splint for three to six weeks should all be included in the rehabilitation regimen.
- The patient should get physical therapy after being immobilized.
A visibly unstable DRUJ or the presence of other unstable or displaced fractures are indications for urgent TFCC surgery. TFCC surgery is also recommended when non-surgical treatment fails after 8 to 12 weeks.
Damage to the TFCC is frequently linked to fractures of the radius bone. It is advised to assess and, if necessary, repair the TFCC if the fracture is treated surgically. A cast is used to treat closed fractures of the radius bone that do not require surgery; the immobilization also promotes TFCC healing.
Surgical Intervention:
If non-surgical measures are unsuccessful or there is DRUJ instability, surgical options should be taken into account. Surgical intervention will rely on the injury’s Palmer classification.
The most used method for categorizing TFCC lesions is the Palmer classification. They are divided into the following two groups (plus some other smaller ones that are not the subject of this article):
Degenerative and traumatizing. This classification offers a precise anatomic description of tears but does not include treatment advice or prognostic information.
Wafer operation, ulnar shortening, arthroscopic repair, and arthroscopic debridement are common surgical alternatives.
Debridement, a surgical treatment, results in bleeding to encourage recovery. Debridement has been proven to have worse effects in degenerative tears or patients with larger positive ulnar variations, although it has positive outcomes for central TFCC tears.
Debridement of TFC discus tissue using an arthrometer
Without blood flow, the TFC’s central region is incapable of mending itself. This region of the TFC frequently develops an unstable flap of tissue that is susceptible to catching on other joint surfaces when a tear occurs there. Debridement is then advised in order to remove the injured tissue. Unfortunately, arthroscopic debridement has a poor prognosis for treating degenerative TFC tears linked to positive ulnar variation.
Repair of TFCC ligaments through arthroscopy
TFCC ligaments can occasionally be stitched arthroscopically. However, only if the ligaments and other supporting structures have not suffered any significant harm. Even after a short time, damaged ligaments have a tendency to retract, losing length. Retracted ligament ends cannot be stitched back together; a reconstruction may be required.
TFCC open surgical repair
For degenerative or more complicated TFCC injuries, or if a subsequent injury to the wrist or forearm caused instability or dislocation, open surgery is typically necessary. Compared to arthroscopic surgery, it is a more intrusive surgical approach, but the surgeon has superior visibility and access to the TFCC.
Surgery options:
- Suturing of the RULs. This is only achievable when the damage is not too severe and if neither of the torn ligament’s ends have yet been retracted, exactly like with arthroscopic suturing of these ligaments.
- Using a tendon graft, such as the palmaris longus, one can restore the RULs’ anatomy. Through bored holes in the ulnar and radius bones, the tendon transplant is inserted. When a TFCC is irreparably damaged, DRUJ instability is suggested by this method.
- Plication of the extensor or capsular retinaculum. By cutting the joint capsule or the extensor retinaculum shorter, this surgical procedure seeks to increase DRUJ stability.
Physiotherapy:
- Rest, physical therapy, and corticosteroid injections are all part of the first treatment.
- Various factors determine how long conservative measures should be used before moving on to surgical procedures.
- If the distal radioulnar joint is not unstable, six months of conservative therapy are feasible.
Post-Operative Rehabilitation:
Depending on the procedure, recovery takes anywhere from four to six weeks for arthroscopy and about three months for an open approach. Physical rehabilitation will be provided to patients following the surgery. The type of surgery performed and the surgeon’s discretion determine the precise start date and duration of physical therapy.
Regarding type 1 wounds
WEEK 1:
- Following the arthroscopy, the wrist will be immobilized for one week.
- Exercises for range of motion can be started after one week.
- Golf, boxing, tennis, water skiing, gymnastics, pole vaulting, and hockey are all sports that frequently result in TFCC tears.
WEEK 3-4
- Three weeks after the arthroscopy, golfers and tennis players with a stable TFCC tear can begin light ball contact. They can return to their normal sports activities in 4 to 6 weeks.
- When the symptoms remain, an ulnocarpal corticosteroid injection can be an option.
- For more severe injuries, post-operative immobilization in a Muenster cast for 4 weeks may be considered.
- After four weeks, the wrist is put in Versa’s wrist splint or short arm splint, which allows the wrist to move gradually.
- The wrist pain and aggravation will lessen due to immobilization, which can accelerate recovery.
- Some splint varieties will aid in wrist stabilization, which will enhance hand function.
- Exercises to improve range of motion and grip strength can then be introduced to patients.
- Because eccentric grip strengthening activities will affect the co-activation pattern of the wrist flexors, which aid in wrist stabilization, therapists are more likely to recommend them.
- To increase overall wrist stability, further co-activation exercises might be added.
8 weeks following surgery:
- Start your active muscle training regimen.
- It is advised to follow a pain-free workout routine.
- The administration of physical therapy should incorporate patient education and activity moderation.
- The area should be strengthened using isometric exercises to lower the possibility of instability.
- Particularly advantageous are unilateral isometric workouts, which have been shown to boost bilateral voluntary muscle activation. Additionally, neutral wrist position and controlled isometric activation of the pronator quadratus will help to stabilize the distal radioulnar joint (DRUJ). This may be because the motor cortex is stimulated, leading to stronger neuromuscular control. Patients with TFCC injuries can use this both pre-and postoperatively.
3 months:
- Patients are expected to resume normal exercise three months after surgery.
- To resume regular athletic activities, a further 3 to 4 months are required.
Passive Mobilization:
- An initial test to see if this causes discomfort is a Traction of the radiocarpal and midcarpal joints.
- An effective dorsal sliding technique can be utilized to encourage wrist flexion.
- Utilizing the volar sliding technique can help increase wrist extension.
- Utilizing the ulnar sliding technique can help increase radial deviation.
- Using the radial sliding approach, the ulnar deviation can be facilitated.
Exercises for General Mobility
The patient should carry out the following general mobility drills:
- Rotating wrists.
- Radial and ulnar deviations in the horizontal
- Supination and active pronation
- Wrist flexion and extension stretching
Strengthening exercises:
Continue with strengthening exercises after the therapy is finished. The workouts that follow can all be completed with a terra tire or a weighted handhold.
- Extension and flexion
- Both supination and pronation position is used.
Multiple Diagnoses:
- Hypothenar hammer syndrome: Differentiate from hypothenar hammer syndrome because the fourth or fifth digits may exhibit discoloration, fingertip ulcers, or splinter hemorrhages. This disease might be diagnosed with angiography.
- Ulnar carpal impingement: Differentiate when dealing with ulnar carpal impingement, which frequently results from ulnar shortening brought on by surgical resection following a prior accident.
- Ulnar extensor or flexor tendonitis: Pain is brought on by actions that activate the muscle. Depending on the level of inflammation, pain may radiate down the belly of the muscle.
- DRUJ chondral lesions or osteoarthritis: Differentiate between osteoarthritis and DRUJ chondral lesions using radiographic evidence that points to either condition.
Ulnar Styloid Impingement Syndrome: TFCC injury-like symptoms with an intact TFCC.
Prognosis:
Generally speaking, the prognosis for TFCC injury is positive. When combined with ulnar shortening osteotomy, arthroscopic repair, and debridement have both been demonstrated to be successful procedures. Children with surgical management also have a strong chance of recovering and returning to sport, as it has been proven to be effective in high-level pediatric and teenage athletes.
In one study, arthroscopic debridement resulted in a 70% satisfaction rate among 71 individuals with a central TFCC tear under the age of 45. They also discovered that outcomes were generally worse when there were degenerative rips and more positive ulnar variance. Negative results from the DRUJ stress test, being a woman, and having symptoms that last longer are some indicators of poor prognosis. When patients follow surgical guidelines, the prognosis over the long term is better.
Conclusion
When alternative causes of ulnar-sided wrist discomfort are ruled out and conservative therapy is started, the results of TFCC injuries will be optimal. The majority of TFCC injuries respond satisfactorily to conservative care. We’ll begin by immobilizing the wrist to allow the ligament time to repair.
After that, we’ll establish a schedule of stretches and exercises to help the muscles and tendon in the area become stronger and to gradually reestablish a normal range of motion.
A prompt surgical consultation is the next step if the patient doesn’t get better with conservative treatment.
If an MRI (read by a radiologist with knowledge of TFCC damage) is obtained.
The best follow-up care will be given by an interprofessional team consisting of a nurse, physical or occupational therapist, and doctor.
FAQs:
Bracing: You can help your TFCC recover by keeping your forearm and wrist stable with a brace or splint. Cortisone injections can assist to lessen the swelling of damaged tissue. Physical or occupational therapy: To help prevent further damage, exercises can help to strengthen the muscles in your wrist and forearm.
Older folks also have TFCC tears more frequently. TFCC tears frequently heal on their own, but a patient must refrain from using their wrist while the injury is healing. A doctor could advise surgery or physical therapy for tears that are serious or persistent.
Like most surgical procedures, TFCC repair procedures carry potential dangers, such as: Operative site infection. tendon and nerve injury. pain from scars, stiffness, and swelling.
Every time you move your wrist, you could experience pain, which makes performing simple chores difficult. The likelihood that a TFCC tear will lead to persistent instability increases the longer it is left untreated.
Acute peripheral TFCC rips that are treated within three months of the lesion produce results that are 60 to 90 per cent good to outstanding, with grip strength and range of motion that is 80 to 90 per cent higher than on the contralateral side.


6 Comments