Spirometry
- Spirometry is a simple test that measures how much air you can breathe out in one forceful breath to help diagnose and monitor certain lung problems.
- It is done with a spirometer, which is a little machine attached by a cable to a mouthpiece.
- Spirometry can be done at your GP surgery by a medical professional or nurse, and Physiotherapist or it can be done during a brief visit to a hospital or clinic.
Table of Contents
Introduction:
Spirometry is the word used to describe the basic lung function tests that assess the amount of air that is exhaled and inspired Volume, time, and flow are the three main connected measures. Spirometry is objective, noninvasive, detects early changes, and is reproducible. With the availability of portable meters, it may be conducted practically anywhere and by anyone with the proper training.
It is used to detect the presence or absence of lung disease, quantify lung damage, monitor the impacts of occupational/environmental exposures, and determine drug effects.
The measures:
Spirometric measures include the following.
- Forced expiratory volume in 1 s (FEV1)
- Forced vital capacity (FVC), is the most amount of air exhaled when blowing out as rapidly as possible.
- Vital capacity (VC), is the most air that can be exhaled at a continuous rate.
- FEV1/FVC ratio
- Peak expiratory flow (PEF), is the maximum volume of air that can be exhaled while blowing out as soon as achievable.
- Forced expiratory flow, also known as mid-expiratory flow; rates are reported at 25%, 50%, and 75% FVC.
- Inspiratory vital capacity (IVC), is the maximum amount of air that can be inhaled following a complete expiration.
Why spirometry is carried out:
- If you have symptoms or your doctor believes you are at an elevated risk of developing a certain lung condition, spirometry can be used to help identify it.
- Spirometry may be advised if you have a recurrent cough or shortness of breath, or if you are over 35 and smoke.
Pulmonary function tests:
The main piece of equipment used for basic Pulmonary Function Tests (PFTs) is a spirometer. Asthma, bronchitis, and emphysema may be ruled out by the testing. Furthermore, a spirometer is frequently used to determine the reason for shortness of breath, examine the influence of pollutants on lung function, and the effect of medication, and evaluate disease treatment progress.
Reasons for testing:
- Certain types of lung illness (such as COVID-19, bronchitis, and emphysema) must be diagnosed.
- Determine the source of your shortness of breath.
- Determine whether workplace chemical exposure impacts lung function.
- Before a patient has surgery, their lung function should be evaluated.
- Examine the medication’s impact.
- Evaluate disease treatment progress.
Spirometry can detect and monitor the following conditions:
- Asthma – A long-term disorder in which the airways become inflamed (swollen) and narrowed on a regular basis
- Chronic obstructive pulmonary disease (COPD) is a series of lung diseases in which the airways narrow
- Cystic fibrosis – Cystic fibrosis is a congenital disease that causes the lungs and digestive tract to become clogged with thick, sticky mucus.
- Pulmonary fibrosis – pulmonary scarring
If you’ve already been diagnosed with one of these disorders, spirometry may be used to determine the severity of the condition or how well you’re responding to treatment.
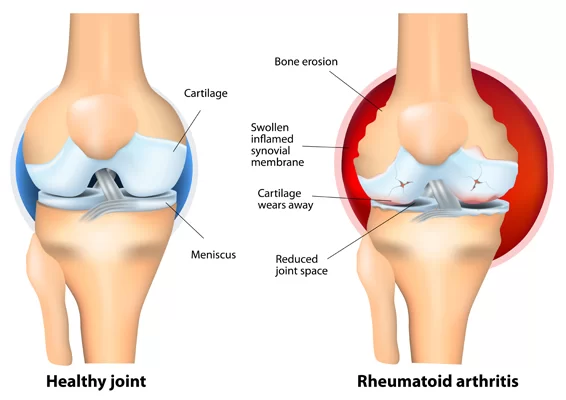
Spirometry is also used to assess the general health of persons who have various illnesses, such as rheumatoid arthritis, or for people who are considering surgery.
Preparing for the test:
- You’ll be taught what you need to do to prepare for the exam.
- If you use bronchodilators (inhaled medications that relax and open your airways), you may need to cease using them beforehand.
- You should also avoid smoking for 24 hours before the test, as well as drinking alcohol, excessive exercise, and eating heavy meals.
- On the day of the test, wear loose, comfortable attire.
What happens during a spirometry examination?
- During the test, you will be seated, and a soft clip will be placed on your nose to prevent air from escaping.
- The examiner will explain what you need to accomplish, and you may be asked to practice for a few minutes first.
- A nurse stands next to a man who is sitting. The man is blowing into a tube that is attached to a handheld recording device.
You will be asked to take a deep breath and blow into a small tube (spirometer) during spirometry.
When you’re finished, you’ll be prompted to:
- Close your lips tightly around the mouthpiece and fully inhale until your lungs are totally filled with air.
Exhale as swiftly and strongly as you can, making sure your lungs are completely empty.
This should be done at least three times to get a consistent result. - The test may need to be repeated roughly 15 minutes after inhaling bronchodilator medication.
- This can indicate whether you have a lung ailment that responds to these medications.
- Your appointment should last between 30 and 90 minutes. After the tests are completed, you will be permitted to return home and resume your daily activities.
Your outcomes:
- Typically, the individual doing the test will not be able to provide you with your results right away.
- Before being forwarded to the doctor who referred you for the test, the results must first be examined by a specialist, who will discuss them with you a few days later.
- A spirometer measures how much air you can exhale in a single vigorous breath and in one second.
- These measurements will be compared to a normal result for someone your age, height, and gender to determine if your lungs are functioning normally.
The tests will also identify whether your lungs have an “obstructive” or “restrictive” condition or a combination of both:
- Obstructive airway disease – a condition in which your capacity to breathe out quickly is impaired due to the narrowing of the airways, but the volume of air you can hold in your lungs is normal (as in asthma or COPD).
- Restrictive lung disease occurs when the amount of air you can breathe in is limited due to your lungs’ inability to fully expand (as in pulmonary fibrosis).
Risks and adverse effects:
- Spirometry is a simple test that is usually regarded as highly safe. For a short time afterward, some people may feel dizzy, faint, shaky, nauseated, or fatigued.
- Most people are able to take a spirometry test. However, because the test raises the pressure within your brain, chest, stomach, and eyes when you exhale, it may need to be postponed or avoided if you have a condition that could be worse by it.
- If you have or have recently had unstable angina, a heart attack, uncontrolled high blood pressure, or surgery on your head, chest, stomach, or eyes, for example, spirometry may be dangerous.
- A spirometer is a device that monitors the amount of air that the lungs take in and expel. The passage of air into and out of the lungs is measured with a spirometer. The spirogram will detect obstructive and restrictive abnormal ventilation patterns. Spirometers are classified according to their measurement method (pressure transducers, ultrasonic, or water gauge).
Performing spirometry:
Calibration
- Before doing spirometry, the equipment must be calibrated, or the calibration must be confirmed at the start of the session. Depending on the type of equipment, this is accomplished with either a 3-L syringe pumped a liter at a time to a maximum of 7 L, testing the linearity as well as the volume measurement’s center point. Many spirometers also provide linear calibration, in which the volume is measured at various flows. Some portable meters, such as those that utilize ultrasound technology, may not require calibration. Calibration is a checking function in many meters, and if the calibration is incorrect, the meter must be returned to the manufacturer for repair. There is one exception: some more advanced equipment, such as that found in a lung function laboratory, can update its output based on calibration. Spirometric results should also be evaluated on a weekly basis using a biological control (a healthy laboratory worker).
- Flow is extremely difficult to calibrate and is not performed on a regular basis. To mimic forced expiration, a sophisticated computer-driven syringe is required.
Before testing:
- Prior to doing spirometry, verify the patient’s identification, measure their height without shoes or boots, and weigh them (if scales are available, as this is not used in prediction equations). but is useful to know, as volume may be limited in obese patients), and their age, gender, and race record. If the patient is unable to stand, an arm span might be utilized to approximate their height.
Prior to spirometry, the following factors should be avoided by the patient:
- If inhalers are used within the times specified above for reversibility testing, a true assessment may not be possible because the effect of the provided medicine will be decreased. Normal medication should be documented for general testing so that it is known how the patient’s lung function is on and off therapy, as well as whether spirometry is being used. to be repeated throughout time, conditions can be kept the same. To reduce variability in recent bronchodilator usage, several centers do post-bronchodilator longitudinal assessments.
Contraindications:
If any of the following events have occurred recently, it may be best to postpone spirometry until the patient has fully recovered.
- Unknown cause of hemoptysis
- Pneumothorax
- Cardiovascular instability, recent myocardial infarction, or pulmonary embolism
- Aneurysms in the thoracic, abdominal, or brain regions
- Recent ophthalmic surgery
- Acute conditions that impair test performance, such as nausea or vomiting
- Recent thoracic or abdominal operations
Positioning the patient:
The proper measuring stance is as follows.
- Sit up straight: As long as the patient is sitting up straight and there are no constraints, there should be no difference in the volume of air the patient can exhale from a sitting posture compared to a standing one.
Feet flat on the floor, legs uncrossed: no need for abdominal muscles to maintain leg position.
- Loosen tight-fitting clothing: Tight clothing can provide restrictive spirometry images (lower volumes than are true).
Dentures are typically left in place since it is preferable to retain some structure in the mouth area unless the dentures are too loose.
Use an armchair: When exhaling maximally, patients may become light-headed, sway, or faint.
Infection prevention:
Between patients, hands must be cleansed. Bacterial-viral filters should be used for all patients and discarded at the end of testing. If testing is required for an infected patient, it should be done at the end of the session, and the equipment should be stripped down and sterilized/parts replaced (depending on what is utilized) before being used again.
Technique:
- Spirometry can be performed using a variety of approaches.
- Tidal (normal) breaths can be taken first, followed by a deep breath while still using the mouthpiece, and then another quick, complete inspiration.
- Alternatively, take a big breath in and then close your mouth tightly around the mouthpiece before performing a full expiration.
- The patient can be instructed to thoroughly empty their lungs before inhaling a rapid full inspiration followed by a full expiration.
*The latter approach is effective in patients who have a bigger inspiration after expiration.
- For FVC and FEV1, the patient takes a huge, deep breath in and blows out as strongly and quickly as possible, continuing until no air remains.
- The FEV1 and FVC maneuvers are used to calculate PEF.
- For VC, the patient takes a large, deep breath in and blows steadily for as long as possible until no air remains. Because of the low flow rate, nose clips are required for VC.
- The IVC maneuver is performed at the end of the FVC/VC (depending on the kind of equipment used) by inhaling deeply and quickly after completely exhaling.
- Encouragement is really important, therefore don’t be afraid to use your voice to encourage the patient, especially at the finish of the movement. The patient should continue to blow until no more air comes out and the volume-time trace hits a plateau with 50 mL exhaled in 2 seconds [1]. Some patients, particularly those with obstructive illness, may struggle to completely exhale during a forced maneuver. In this situation, a more relaxed VC may yield superior outcomes.
Quality:
- A number of criteria for acceptable spirometry quality have been published. Three appropriate motions are recommended by the American Thoracic Society (ATS)/European Respiratory Society (ERS) Task Force. The following is a definition of an appropriate maneuver.
- With a back-extrapolation volume of 150 mL, you get an abrupt start (no hesitation or sigmoid curve).
- The maneuver was carried out with maximum inspiration and expiration.
- During the maneuver, there was no glottis closure or stopping of airflow (e.g., by hesitation or blocking the mouthpiece).
- There were no coughs (especially in the first second), inspirations during the trace, or evidence of leakage.
- The technique should meet the end-of-test standards (exhaling for at least 6 seconds and exhaling 50 mL in the last 2 seconds).
- Back-extrapolation along the steepest region of the curve, where flow is peak expiratory flow (PEF), to determine the new time zero in an expanded version of a subject’s volume-time spirogram. FVC (forced vital capacity): 4.291 L; EV (back extrapolated volume): 0.123 L (2.9% FVC). —-: line of back extrapolation through PEF.
- The best two measurements must meet the reproducibility requirements.
- The best two FEV1 and FVC readings should be within 5% or 150 mL of each other, whichever is greater. The values should be within 100 mL if FVC is 1.0 L.
- Different techniques can be used to obtain the greatest FEV1 and FVC.
- More maneuvers will be required if this is not achieved. As executing forced exhalations is exceedingly taxing, and the patient is unlikely to acquire higher readings after this point, there is normally an upper limit of eight maneuvers.
- There may be reproducibility issues: forceful expiration might produce bronchoconstriction, thus there must be at least 30 seconds between maneuvers. Some people, particularly asthmatics, may require several minutes. However, full inspiration can promote bronchodilation, so continue until there is no further improvement.
Correction to BTPS:
Body temperature and ambient pressure saturated with water vapor (BTPS) should be taken into account when doing spirometry. This is done to compensate for the discrepancy between the volume of air in the lungs (at 37°C) and the volume measured by the spirometer (at room temperature). In the absence of barometric pressure, the spirometer should have a pressure range for the correction factor utilized.
Testing for reversibility:
Reversibility testing is commonly used to diagnose asthma. Spirometry is conducted, followed by the administration of a bronchodilator, which can be a short-acting ß-agonist or other drugs such as anticholinergics. For the former, 4100 g salbutamol is indicated via a spacer device, with 15 minutes between tests, and for the latter, 440 g ipratropium bromide is recommended, with 30 minutes between tests. There are several papers [2-5] with slightly varied criteria for what makes a considerable improvement in lung function to decide that the individual has reversed.
The combined ATS/ERS Task Force recommends at least a 12% increase from baseline and a 200-mL improvement in FEV1. According to the British Thoracic Society (BTS)/Association of Respiratory Technicians and Physiologists (ARTP) standards, FEV1 should be greater than 160 mL and FVC should be greater than 330 mL. These reversibility assessments reveal that the change is outside the 95% confidence range for repeat spirometry without any bronchodilator and has no bearing on diagnosis or the drug’s utility in everyday use. Reversibility is the distinguishing feature of asthma, and it distinguishes it from other forms of airway blockage. A post-bronchodilator increase in FEV1 of >400 mL is strongly suggestive of asthma in adults, although a lack of reversibility does not rule out asthma.
Equipment:
There are several types of spirometers available, ranging from desktop portable devices to big, less portable models. Most measure flows directly and calculates volume via pneumotachographs, turbines, or other technology, while the wedge bellows spirometer measures volume directly and calculates flow. The equipment you choose is determined by your service requirements. Although larger equipment is more stable, there are now some highly useful hand-held devices that hold flow-volume loops, have built-in quality control, and measure all spirometric indices. Some of them can also print, while others must be connected to a computer to do so.
Spirometry interpretation:
- Normal lung function
The results of lung function tests have little importance unless they are matched to reference or expected values. There are several reference values available that have been equated in various methods, but the equations from the European Community for Coal and Steel (ECCS) are frequently used in studies comparing different European communities. Reference values are produced using reference equations containing population survey data. The survey population is preferably quite big, and data is collected on respondents’ height, weight, age, gender, ethnic origin, smoking habits, environment, working conditions, and physical fitness. The existing ECCS equations are linear, while lung function change is a nonlinear process. In some cases, the reference values provided may be unrepresentative of the person being evaluated. In the near future, new equations will be provided that should address these concerns. - The main factors of spirometric reference values in adults are age, height, gender, and race.
- Age Lung function normally improves with age up to the age of 25, then falls with age. Unfortunately, certain lung function equipment gives patients above the age of 25 higher anticipated results than patients under the age of 25. To prevent significantly overestimating the expected value for patients 25 years of age, enter the subject’s age as 16 years and then 25 years. If the expected value is greater at 16 years, use the value for 25 years.
Sex Males and females have similar lung function before puberty, but after puberty, the expansion of the thorax is greater in males, resulting in significant disparities in lung sizes. - Height The larger the lungs, the taller the individual.
- Weight Weight is used in certain reference equations to calculate reference values. Weight influences lung function by increasing lung function until obesity is attained, at which point it has the reverse impact.
- ethnic background As a multiethnic community develops, this aspect becomes more difficult to incorporate. According to the BTS/ARTP guidelines, reference values increased by 0.90 should be used for Japanese, Polynesian, Indian, Pakistani, and African individuals, as well as those of African origin. This is related to either physical structure (Africans having longer legs and shorter bodies than Caucasians) or a lack of nourishment in poorer areas. Because many various races are now born in richer nations, nutrition is likely to be less of a concern, and as a general rule, adjustment for race is not normally required by the second generation after immigration. The flow measurements are unaffected.
- Smoking This can result in a faster deterioration in lung function over time when compared to nonsmokers. It should not be accounted for in projected equations because any decrease is anomalous.
Summary:
Spirometry is a powerful tool for detecting early illness changes and providing physiological confirmation of diagnoses. It can be used to assess disease progression and response to medication when done correctly. With the emergence of portable meters, it is now possible to conduct it anywhere and by anyone with adequate training.
Spirometer Types
- Plethysmograph for the whole body
- When compared to other conventional spirometers, this form of spirometer provides a more precise measurement of the components of lung volumes. When the measurement is taken, a person is enclosed in a small space.
- Pneumotachometer
- This spirometer detects pressure variations via thin mesh to determine the flow velocity of gases. The subject can breathe fresh air during the experiment, which is an advantage of this spirometer.
- Fully electronic spirometer
- Electronic spirometers that compute airflow rates in a channel without the use of fine meshes or moving parts have been created. They work by monitoring the speed of the airflow using ultrasonic transducers or by sensing the pressure difference in the channel. These spirometers are more accurate because they eliminate the momentum and resistance inaccuracies associated with moving devices used for flow measurement, such as windmills or flow valves. They also increase hygiene by allowing for completely disposable air flow conduits.
- Incentive spirometer
- This spirometer is specifically intended to facilitate lung function improvement.
- Peak flow meter
- This instrument can be used to assess how well a person’s lungs expel air.
- Windmill-type spirometer
- This type of spirometer is specifically intended for measuring forced vital capacity without the use of water; it has a wide range of measurements ranging from 1000 ml to 7000 ml. It is smaller and lighter than standard water-tank spirometers. Because of the existence of a rotating disc, this spirometer should be held horizontally when taking measurements.
- Spirometry (measurement of breath) is the most common pulmonary function test (PFT). It assesses lung function by determining the amount (volume) and/or rate (flow) of air that can be breathed and expelled. Spirometry is useful in identifying illnesses such as asthma, pulmonary fibrosis, cystic fibrosis, and COPD by examining breathing patterns. It is also useful as part of a health surveillance system that measures breathing patterns throughout time.
- Spirometry produces pneumotachographs, which are charts that show the volume and flow of air entering and exiting the lungs during a single inhale and expiration.
Testing:
- A contemporary USB PC-based spirometer.
- Spirometry instrument. The patient’s lips are wrapped around the blue mouthpiece. The teeth fit between the nubs and the shield, while the lips cover it. A nasal clip ensures that all breathing will be done through the mouth.
- Right, a screen for spirometry readouts. Body plethysmography can also be performed in the chamber.
- Spirometer
The spirometry test is carried out with the use of a spirometer, which comes in a variety of models. Most spirometers show the following graphs, known as spirograms:
A volume-time graph with volume (liters) on the Y-axis and time (seconds) on the X-axis
A flow-volume loop that illustrates the rate of airflow on the Y-axis and the total volume inspired or expired on the X-axis visually - Procedure
Depending on the equipment used, the basic forced volume vital capacity (FVC) test varies slightly. It can take either a closed or open circuit configuration. Regardless of variances in testing procedures, practitioners are advised to adhere to the ATS/ERS Spirometry Standardisation. The standard approach ensures that data is collected accurately and objectively, based on a consistent reference, to limit the compatibility of results when shared across different medical groups.
The patient is instructed to wear soft nose clips to prevent air escape and to place a breathing sensor in their mouth to make an airtight seal. The patient is guided step by step by a technician to take an abrupt maximum-effort inhalation, followed by a maximum-effort exhale lasting at least 6 seconds. When checking suspected upper airway obstruction, the technician will instruct the patient to complete the round with another fast inhalation. The timing of the second inhale varies based on the length of the previous exhale. In certain situations, each session of testing will be followed by a time of regular, soft breathing to gather more information.
Limitations
- Clinically meaningful results rely heavily on patient participation and effort and must be repeated at least three times to assure reproducibility, with a recommended limit of 10 attempts. Because an effort output of more than 100% is not achievable with varying rates of effort, the results can only be underestimated.
- Due to the requirement for patient compliance and the ability to understand and follow directions, spirometry is normally only performed on cooperative children who are at least 5 years old or adults who do not have physical or mental impairments that hinder effective diagnostic results. Furthermore, general anesthesia and other forms of sedation are incompatible with the testing procedure.
- Another disadvantage is that people with intermittent or mild asthma can have normal spirometry values between severe exacerbations, decreasing the efficacy of spirometry as a diagnostic tool in these cases.
- Printout of a contemporary PC-based spirometer.Additional diagnostics
Spirometry can also be performed as part of a bronchial challenge test, which is used to detect bronchial hyperresponsiveness to intense exercise, cold/dry air inhalation, or a pharmaceutical substance such as methacholine or histamine. - A bronchodilator can be supplied before another round of testing to determine the reversibility of a certain disease. This is known as a reversibility test or a post-bronchodilator test (Post BD), and it is crucial in distinguishing asthma from COPD.
- Plethysmography and nitrogen washout are two further lung function tests.
- Investigation of individuals with pulmonary illness symptoms/signs/investigations (e.g., cough, wheeze, shortness of breath, crackles, or abnormal chest x-ray)
Monitoring the progression and response to treatment of patients with known pulmonary disease (e.g., interstitial fibrosis, COPD, asthma, or pulmonary vascular disease).
Patients with conditions that may have respiratory consequences (e.g., connective tissue disorders or neuromuscular diseases) are being investigated.
Prior to lung resection, abdominal surgery, or cardiothoracic surgery, a preoperative examination is performed.
Evaluating people who are at risk of developing lung disorders (for example, exposure to pulmonary toxins such as radiation, medicine, or environmental or occupational exposure)
Following lung transplantation, patients are monitored for signs of acute rejection, infection, or obliterative bronchiolitis.
Indications
Spirometry should be used for the following reasons:
- Asthma diagnosis or management to detect respiratory disease in patients With complaints of shortness of breath and separate respiratory disease from heart disease as the cause
- To assess bronchial reactivity in patients suspected of suffering from asthma
- To Identify and distinguish between obstructive and restrictive lung disease
- To track the progression of disease in respiratory conditions
- To assess occupational asthma impairment
- To identify those who are in danger of pulmonary barotrauma while scuba diving
- To do a pre-operative risk assessment prior to anesthesia or cardiothoracic surgery
- To assess responsiveness to therapy of diseases detected by spirometry
- To diagnose the vocal cord impairment.
Contraindications
Some medical disorders may be exacerbated by forced expiratory maneuvers. Spirometry should not be performed if the patient has any of the following conditions:
- Hemoptysis of undetermined cause
- Pneumothorax
- Cardiovascular instability (angina, recent myocardial infarction, etc.)
- Aneurysms in the thoracic, abdominal, or brain regions
- Cataracts or recently performed eye surgery
- Recently performed thoracic or abdominal surgery
- Nausea, vomiting, or a serious disease
- A recent or ongoing viral infection
- Hypertension that has gone undiagnosed
Spirometry is a type of Pulmonary Function Test; it is beneficial in the therapy of individuals with respiratory disease or respiratory weakness caused by neurological disability. They help with diagnosis, monitoring treatment response, and guiding treatment and intervention decisions. Except for residual volume, spirometry can measure all lung volumes.
Definitions of measurements
The measurement definitions are as follows:
FEV1 (forced expiratory volume in one second) is the amount of air expelled forcibly after full inhalation in the first second.
Forced vital capacity (FVC) is the amount of air expelled forcibly following full inspiration.
FEV1/FVC is the ratio of the two volumes. This computation identifies obstructive or restrictive ventilatory problems. FEV1/FVC 70%, when FEV1 is lower than FVC, indicates obstructive pathology. In restrictive pathology, FEV1/FVC is greater than 70%, indicating that FVC is lowered more than FEV1.
Vital capacity (VC) The largest volume of air that can be exhaled when blowing out as quickly as possible.
Peak expiratory flow (PEF) is the maximum amount of air that can be exhaled when blowing out at a constant rate.
Parameters
- Spirometry’s most common parameters are Vital capacity (VC), Forced vital capacity (FVC), Forced expiratory volume (FEV) at timed intervals of 0.5, 1.0 (FEV1), 2.0, and 3.0 seconds, forced expiratory flow-maximal voluntary ventilation (MVV), often known as maximum breathing capacity, and 25-75% (FEF 25-75). Other tests may be conducted in certain circumstances.
- The test result is typically presented in both raw data (liters, liters per second) and % predicted—the test result as a percentage of the “predicted values” for patients with similar characteristics (height, age, sex, and, in some cases, race and weight). The results can be interpreted differently depending on the physician and the source of the anticipated numbers. In general, results closest to 100% expected are the most typical, and results greater than 80% are frequently deemed normal. Multiple articles have predicted values that can be derived based on age, gender, weight, and ethnicity. However, a doctor’s review is required for a precise diagnosis of any unique circumstance.
- In some cases, a bronchodilator is also administered, and the efficiency of the bronchodilator is assessed via a pre/post-graph comparison. See the printout for an example.
- FRC (Functional residual capacity) cannot be measured using spirometry, but it can be measured with a plethysmograph or dilution tests (for example, helium dilution test).
- Forced vital capacity (FVC)
The volume of air that can be forcibly blown out after complete inspiration, measured in liters, is known as forced vital capacity (FVC). The most basic maneuver in spirometry examinations is FVC. - FEV1(Forced expiratory volume in one second)
FEV1 is the amount of air that can be forced out in the first 1-second after full inhalation. According to the graphic, average FEV1 values in healthy adults are mostly determined by gender and age. Normal values are between 80% and 120% of the average value. FEV1 predicted normal values can be determined and depend on age, gender, height, weight, ethnicity, and the research paper on which they are based. - The FEV1/FVC ratio
FEV1/FVC is the FEV1 to FVC ratio. This should be around 70-80% in healthy persons (decreasing with aging).In obstructive diseases (asthma, COPD, chronic bronchitis, emphysema), FEV1 is reduced due to increased airway resistance to expiratory flow; FVC may be reduced as well, but not in the same proportion as FEV1 (for example, both FEV1 and FVC are reduced, but the former is more affected due to the increased airway resistance). This results in a lower value (usually 70%, but sometimes 45%). In restrictive disorders (such as pulmonary fibrosis), both FEV1 and FVC are lowered proportionally, yet the value may be normal or even raised due to decreased lung compliance. - FEV1% predicted (FEV1%) is a derived value of FEV1, which is defined as the patient’s FEV1 divided by the average FEV1 in the community for any person of the same age, height, gender, and race.
- FEF stands for forced expiratory flow.
The flow (or speed) of air coming out of the lung during the middle section of a forced expiration is referred to as forced expiratory flow (FEF). It can be delivered at discrete moments, which are commonly characterized by the fraction of forced vital capacity (FVC) exhaled. The typical discrete intervals are 25%, 50%, and 75% (FEF25, FEF50, and FEF75), or 25% and 50% of exhaled FVC. - It can also be presented as a mean of the flow across an interval, which is commonly characterized by when specified fractions of FVC remain, often 25-75% (FEF25-75%). Average ranges in the healthy population are mostly determined by gender and age, with FEF25-75% depicted in the diagram at left. Normal values range from 50 to 60% and can reach 130% of the average. Predicted normal values for FEF can be determined and depend on age, gender, height, weight, ethnicity, and the research paper on which they are based.
- MMEF or MEF stands for maximal (mid-)expiratory flow and is the peak of expiratory flow as measured in liters per second from the flow-volume curve. It should ideally be the same as peak expiratory flow (PEF), which is often measured with a peak flow meter and expressed in liters per minute.
- According to recent research, FEF25-75% or FEF25-50% may be a more sensitive indicator than FEV1 in detecting obstructive small airway illness. Disparities in mid-range expiratory flow, however, may not be specific enough to be beneficial in the absence of concurrent alterations in the standard markers, and current practice guidelines advocate continuing to use FEV1, VC, and FEV1/VC as indicators of obstructive illness.
- Forced expiratory flow may be administered at intervals determined by how much total lung capacity remains. In such instances, it is typically denoted as FEF70%TLC, FEF60%TLC, or FEF50%TLC.
- 25-75% or 25-50% forced inspiratory flow
FIF 25-75% or 25-50% (FIF 25-75% or 25-50%) is comparable to FEF 25-75% or 25-50% in that it is measured during inspiration. - PEF stands for peak expiratory flow.
- Peak expiratory flow (PEF) normal values are presented on an EU scale.
Peak expiratory flow (PEF) is the maximum flow (or speed) achieved during the most forcefully driven expiration beginning at full inspiration, measured in liters per minute or liters per second. - TV stands for tidal volume.
Tidal volume is the amount of air regularly inhaled or expelled at rest. - TLC stands for total lung capacity.
Total lung capacity (TLC) is the greatest amount of air that can be held in the lungs. - DLCO stands for diffusing capacity.
The carbon monoxide uptake from a single inspiration in a standard time (typically 10 seconds) is referred to as diffusing capacity (or DLCO). During the test, the subject inhales a test gas combination made up of ordinary air, an inert tracer gas, and less than 1% CO. Because hemoglobin has a higher affinity for CO than oxygen, the breath-hold time can be as little as 10 seconds, which is sufficient for CO transfer. Because the amount of CO breathed is known, the amount transferred during the breath-hold period is calculated by subtracting the amount of CO exhaled. To assess the dispersion of the test gas combination, the tracer gas is analyzed concurrently with CO. This test will detect diffusion defects, such as those seen in lung fibrosis. Anemia (low hemoglobin concentration reduces DLCO) and pulmonary hemorrhage (extra RBCs in the interstitium or alveoli absorb CO and artificially enhance DLCO capacity) must be addressed. Because atmospheric pressure and/or altitude will alter observed DLCO, a correction factor is required to account for standard pressure. - MVV stands for maximum voluntary ventilation.
The maximum voluntary ventilation (MVV) is the amount of air that can be inhaled and expelled in one minute. This is done over a 15-second period for the patient’s comfort before being extrapolated to a figure for one minute expressed in liters/minute. Males and females have average levels of 140-180 and 80-120 liters per minute, respectively. - Measurement Estimated value
Male and female - Tidal volume (Vt) 4.8 L 3.7 L
Forced vital capacity (FVC)
Total lung capacity (TLC) 6.0 L 4.7 L Others 500 mL 390 mL - Others
- FET stands for Forced Expiratory Time.
The Forced Expiratory Time (FET) is a measurement of how long it takes to expire in seconds. - SVC stands for slow vital capacity.
SVC is the greatest volume of air that can be exhaled slowly after a gradual maximum inhalation. - Pmax and Pi (maximal pressure)
- Age 20 Male Female Spirometer ERV in cc (cm3) average
- Pmax is the asymptotically maximum pressure that the respiratory muscles can generate at any lung volume, and Pi is the highest inspiratory pressure that can be generated at specific lung volumes. Pressure transducers are also required for this measurement. It is considered normal if it is 60% to 140% of the population average for any person of similar age, gender, and body composition. The coefficient of retraction (CR), which is Pmax/TLC, is a derived metric.
- MTT (mean transit time)
The mean transit time is calculated by dividing the area under the flow-volume curve by the forced vital capacity. - MIP stands for maximum inspiratory pressure. The maximum pressure that may be generated against a blocked airway commencing at functional residual capacity (FRC), also known as negative inspiratory force (NIF), is known as MIP. It is a measure of the function and strength of the respiratory muscles. Measured with a manometer in centimeters of water pressure (cmH2O). Maximum inspiratory pressure is a significant and noninvasive indicator of diaphragm strength, as well as an independent diagnostic tool for many disorders.MIP = 142 – (1.03 x Age) cmH2O, where age is in years, can be used to calculate typical maximum inspiratory pressures in adult males.
Spirometers make use of many technologies:
- Spirometers with Volume
- Water chimes
- The bellows wedge
- Flow measurement Spirometers
- Fleisch-pneumotach
- (screen) Lilly pneumotach
- Turbine/Stator Rotor (often referred to mistakenly as a turbine. Actually, it’s a rotating vane that spins due to the subject’s airflow. The vane’s revolutions are noted when they break a light beam)
- The pitot tube
- Anemometer with a hot wire
- Ultrasound
FAQs
To assess how effectively your lungs are working, a common office test called spirometry, pronounced “spy-ROM-uh-tree,” monitors how much air you breathe in, how much you breathe out, and how quickly you exhale. Spirometry is used to diagnose breathing conditions such as chronic obstructive pulmonary disease (COPD), asthma, and others
An FEV1/FVC ratio of more than 0.70 with both FEV1 and FVC above 80% of the expected value are considered normal spirometry data. TLC exceeding 80% of the predictive value when lung volumes are performed is considered normal. A diffusion capacity that is greater than 75% of the projected value is regarded as typical.
A spirometry test is not uncomfortable. However, due to your deep breathing, you can experience fatigue, lightheadedness, or vertigo. You might cough if you blow into the tube. Soon after the test is over, these symptoms ought to be gone.
A healthy FEV1% is typically above 70% for adults and between 80 and 85% for youngsters.
Essentially 6 litres
Around 6 liters is the normal lung volume in healthy individuals. Age, gender, body composition, and ethnicity all have an impact on the different lung capacity ranges that exist among individuals. TLC grows quickly from childhood to adolescence before plateauing at age 25.TLC rapidly rises from infancy to adolescence and reaches a plateau at the age of 25.
The most typical of the pulmonary function tests (PFTs) is spirometry, which literally means the measurement of breath. It gauges the capacity of the lungs to inhale and exhale air, specifically the volume and/or rate of airflow.





One Comment