The Sacral Plexus
Table of Contents
What is the sacral plexus?
The sacral plexus is placed on the posterolateral wall of the pelvic cavity, fibbing anterior to the Piriformis. The sacral subsidies part out of the anterior sacral foramina and course laterally & inferiorly on the pelvic wall.
A majority of the nerves originating from the sacral plexus pass through the greater sciatic foramen – inferior to the piriformis muscle – and join the gluteal region of the lower limb. The remaining observe different roots or do not exit the pelvic cavity.
Root of Sacral plexus
The sacral plexus is constructed by the anterior rami of S1 to S4 as well as the lumbosacral trunk (anterior ramus of L4 & L5).
The lumbosacral trunk routes vertically into the pelvic cavity from the abdomen and passes immediately anterior to the sacroiliac joint.
Spinal Nerves
The spinal nerves S1 – S4 build the base of the sacral plexus.
At each vertebral level, paired spinal nerves exit the spinal cord through the intervertebral foramina of the vertebral column.
Each nerve then separates into anterior and posterior nerve fibers.
The sacral plexus forms as the anterior fibers of the spinal nerves S1, S2, S3, and S4. They are joined by the 4th and 5th lumbar roots, which connect to form the lumbosacral trunk. This plunges into the pelvis to meet the sacral roots as they arise from the spinal cord.
Origin
The sacral plexus is a nerve network contained in the lumbosacral trunk and sacral spinal nerves. The lumbosacral trunk is developed by the lumbar spinal nerves L4 and L5. The trunk then plunges into the pelvis to meet the roots of sacral spinal nerves S1 – S4, as they emerge from the spinal cord. Note that the S4 root only partly donates to the formation of the sacral plexus.
| Nerve | Segment | Innervated muscles | Cutaneous branches |
| Superior gluteal | L4-S1 | Gluteus medius Gluteal minimus Tensor fasciae late | |
| Inferior gluteal | L5-S2 | Gluteus maximus | |
| Posterior cutaneous femoral inferior cluneal nerves perineal branches | S1-S3 | ||
| Perforating cutaneous | S2-S3 | ||
| Direct branches from plexus | |||
| Piriformis | S1-2 | Piriformis | |
| Obturator internus | L5, S1-2 | Obturator internus and Superior gemellus | |
| Quadratus femoris | L4-5, S1 | Quadratus femoris and Inferior gemellus | |
| sciatic | |||
| Sciatic | L4-S3 | Semitendinosus (Tib) Semimembranosus (Tib) Biceps femoris • Long head (Tib) • Short head (Fib) Adductor magnus (medial part, Tib) | |
| Common fibular | L4-S2 | ||
| Superficial fibular | Fibularis longus Fibularis brevis | ||
| Deep fibular | Tibialis anterior Extensor digitorum longus Extensor digitorum brevis Extensor hallucis longus Extensor hallucis brevis Fibularis Tertius | The lateral cutaneous nerve of the big toe intermediate dorsal cutaneous | |
| Tibial nerve | L4-S3 | Triceps surae (gastrocnemius, soleus) Popliteus Plantaris Tibialis posterior Flexor digitorum longus Flexor hallucis longus | Medial sural cutaneous Medial calcaneal Lateral dorsal cutaneous |
| Medial planter | Abductor hallucis Flexor digitorum brevis Flexor hallucis brevis (medial head) Lumbrical (first and second) | Proper digital planter | |
| lateral planter | Flexor hallucis brevis (lateral head) Quadratus Plantae Abductor digiti minimi Flexor digiti minimi Lumbrical (third and fourth) Planter interossei (first to third) Dorsal interossei ( first to fifth) Adductor hallucis | Proper planter digital | |
| Pudendal ( Pudendal plexus ) | S2-S4 | Muscles of the pelvic floor: Levator ani superficial transverse perineal Deep transverse perineal Bulbospongiosus Ischiocavernosus Sphincter anus externus Urethral sphincter | Inferior rectal perineal Posterior scrotal/labial Dorsal penis/clitoris prostatic urethra./vagina |
| Coccygeal (Coccygeal plexus) | S5-Co1 | Coccygeus | Anocccygeal Dorsal branches |
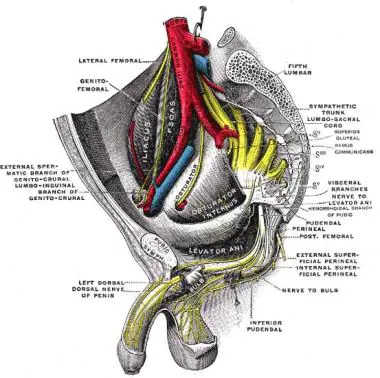
Location
The spinal nerves that form the sacral plexus arise from the lateral (side) areas of the spinal cord. Each of these nerves travels via its corresponding spinal foramen (opening) before they join in their various mixtures to form the sacral plexus in the back of the pelvis.
The sacral plexus is divided into smaller nerves within the pelvis. Some of the nerves stay in the pelvis and some develop down the leg. Some nerves of the sacral plexus leave the pelvis via the greater sciatic foramen—a large opening formed of pelvic bones that contain muscles, nerves, and blood vessels—and then travel down the leg.
Anatomical Variations
There are several natural deviations in the structure of the sacral plexus. These deviations generally do not lead to any clinical problems, but they may be noticed in an imaging study, or they can be observed during a surgical procedure.
Periodically, nerves of the sacral plexus may be larger or smaller than average, or a spinal nerve that typically donates nerve fibers to a nerve of the sacral plexus might not do so. The plexus may form or separate at a higher or lower region in the pelvis than desired.
Branches and supply
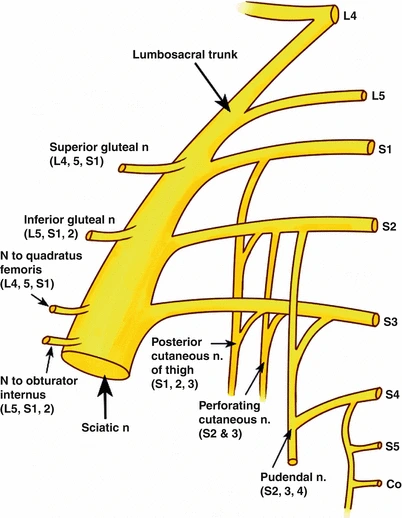
The sacral plexus supplies motor and sensory innervation via the following nerves:
- Sciatic Nerve (L4 – S3)
- Nerve to Obturator Internus (divisions of L5 – S2)
- Pudendal Nerve (ventral divisions of S2 – S4)
- Superior Gluteal Nerve ,dorsal divisions of L4 – S1
- Nerve to Quadratus Femoris
- Posterior Femoral Cutaneous Nerve
- Obturator Nerve (L2 – L4)
- Nerve to Quadratus Femoris
- Perforating Cutaneous
- Nerve to Piriformis
- NerveInferior Gluteal Nerve, dorsal divisions of L5 – S2
The sacral plexus supplies an enormous number of branches that can be separated into posterior, anterior, and terminal branches. The posterior branches arise from the posterior branches of the anterior rami of spinal nerves, while the anterior branches are derived from the anterior divisions.
The largest and only terminal branch is the sciatic nerve which produces two divisions:
- The tibial nerve and the typical fibular (peroneal) nerve.
- Posterior branches
- Superior gluteal nerve
- Nervus gluteus superior
The superior gluteal nerve is formed from the posterior branches of the anterior rami of the L4, L5, and S1 spinal nerves. It accumulates entrance to the gluteal area by coursing over the superior border of the piriformis muscle via the greater sciatic foramen. Afterward, the superior gluteal nerve crosses laterally beneath the gluteus medius and innervates the tensor fasciae latae, gluteus medius, and gluteus minimus.
Inferior gluteal nerve
The inferior gluteal nerve accepts contributions from the posterior branches of the anterior rami of the L5, S1, and S2 spinal nerves. It carries a similar route via the greater sciatic foramen but is inferior to the piriformis muscle. It crosses superficial to the sciatic nerve and innervates the gluteus maximus muscle.
Perforating cutaneous nerve
The perforating cutaneous nerve is also constituted of morally posterior branches, this time arising from the fibers of the anterior rami of spinal nerves S2 and S3. It passes via the greater sciatic foramen, superior to the Gemelli and obturator internus, shooting the sacrotuberous ligament and gluteus maximus. This nerve delivers cutaneous supply to a small area of skin on the inferior medial part of the buttock.
Pelvic splanchnic nerves
The pelvic splanchnic nerves arise from the anterior rami of spinal nerves S2, S3, and S4. They supply both parasympathetic and motor innervation to muscles of the pelvic cavity and pelvic floor. The parasympathetic flow binds the inferior hypogastric (pelvic) plexus. Its motor component supplies the bladder and the distal part of the large intestines (from the left colic flexure, along). It also participates in a clitoral (or penile) erection.
Nerve to piriformis
The nerve to piriformis usually originates from the dorsal branches of the anterior rami of spinal nerves S1 and S2 and
joins the anterior surface of the piriformis muscle and provides it.
Anterior branches
Nerve to quadratus femoris
The nerve to quadratus femoris originates from the anterior divisions of the anterior rami of the spinal nerves L4, L5, and S1. The nerve travels inferiorly underneath the sciatic nerve and passes toward the quadratus femoris. Along its route, it supplies the inferior gemellus muscle and supplies an articular branch to the hip joint.
Nerve to obturator internus
The nerve to obturator internus originates from the anterior divisions of the anterior rami of spinal nerves L5, S1, and S2. The nerve crosses inferior to the piriformis and leaves the pelvis via the greater sciatic foramen, where it gives off a branch to innervate the superior gemellus muscle. It then runs around the ischial spine and reenters the pelvis via the lesser sciatic foramen and pierces the obturator internus.
The posterior cutaneous nerve of the thigh
The posterior cutaneous nerve of the thigh (also known as the posterior femoral cutaneous nerve) is the best component of the sacral plexus that accepts fibers from both the anterior and posterior branches of the anterior rami.
Its fibers originate from:
- Posterior branches of the anterior rami of spinal nerves S1 and S2.
- Anterior branches of the anterior rami of spinal nerves S2 and S3.
Inferior gluteal artery, and superior to the Gemelli, obturator internus, and sciatic nerve. The nerve has an anteroposterior and superoinferior field of cutaneous and fascial supply between the anterior and posterior axillary cords from the buttock to the middle of the calf muscles. The posterior femoral cutaneous nerve also provides uprise to gluteal departments that supply cutaneous supply to the contour of the buttock and perineal branches that innervate the skin of the lateral perineum (two-thirds of the posterolateral part of the scrotum in males, or labium majus in females) and the adjacent part of the upper medial thigh.
Pudendal nerve
The anterior branches of the anterior rami of spinal nerves S2, S3 and S4 connect on the anterior surface of the piriformis (posterior to the inferior gluteal artery) to form the pudendal nerve. The pudendal nerve crosses inferiorly around the sacrospinous ligament to enter the pudendal canal with the pudendal vessels.
The pudendal nerve gives uprise to:
- The inferior rectal nerve innervates the external anal sphincter, anal canal, and perianal skin.
- The perineal nerve supplies cutaneous supply to part of the posterior scrotum (vulva), mucus membrane of the urethra and vagina, and motor innervation to the muscles of the perineum.
- The dorsal nerve of the clitoris/penis supplies cutaneous innervation to this region. Nerve to levator ani and iliococcygeus muscles
- The last two branches of the sacral plexus are the nerve to levator ani and iliococcygeus muscle. It supplies motor innervation to the pelvic part of the muscles for which they are called.
Sciatic nerve
The sciatic nerve is the terminal and largest branch of the sacral plexus originating from both anterior and posterior branches of the anterior rami of spinal nerves L4 to S3. The nerve leaves the pelvic cavity by the course of the greater sciatic foramen. In the gluteal region, it crosses deep to the gluteus maximus and the inferior gluteal artery. It runs over the posterior surface of the Gemelli, piriformis, quadratus femoris, and the ischial fibers of the adductor femoris. The sciatic nerve forms branching at about the center between the ischial tuberosity and the greater trochanter to provide the hamstring muscles and the ischial fibers of the adductor Magnus.
At the apex of the popliteal fossa, the nerve generally separates into the common peroneal and tibial nerves. These two nerves are responsible for innervating the muscles and joints of the leg and foot. The sciatic nerve must accept vasa nervorum (small artery supplying arterial blood to peripheral nerves) from the inferior gluteal artery.
Function of Sacral plexus
The sacral plexus has comprehensive functions throughout the pelvis and legs. Its branches supply nerve stimulation to severa muscles. The nerve branches of the sacral plexus also obtain sensory messages from the skin, joints, and structures throughout the pelvis and legs.
Motor Function
Motor nerves of the sacral plexus obtain their transmissions from the motor area of the brain, which transmits the messages down the ventral (front) column of the spine, out to the sacral plexus, and ultimately to the motor nerve branches of the sacral plexus to stimulate muscle compaction (movement).
Motor nerves of the sacral plexus include:
Superior gluteal nerve: This nerve supplies stimulation to the gluteus minimus, gluteus medius, and tensor fascia lata, which are muscles that support moving the hip laterally (out from the center of the body).
Inferior gluteal nerve: This nerve supplies stimulation to the gluteus maximus, a large muscle that drives the hip laterally.
Sciatic nerve: The sciatic nerve has a tibial part and a common fibular part, which have a motor and sensory functions.
The tibial part stimulates the adductor, Magnus, on the internal part of the thigh as well as muscles in the back of the thigh, which carry the upper part of the leg towards the body. The tibial part also activates muscles in the back of the leg and the sole. The common fibular part of the sciatic nerve stimulates the short head of the biceps femoris, which drives the thigh and knee. This typical fibular nerve also stimulates muscles in the front and sides of the legs and the extensor digitorum brevis, which extends toes to straighten their release.
Pudendal nerve: The pudendal nerve (which also has sensory functions) provokes the muscles of the urethral sphincter to control urination and the muscles of the anal sphincter to control elimination (pooping). The nerve to the quadratus femoris provokes the muscle to move your thigh. The nerve to the obturator internus muscle provokes the muscle to rotate the hip and stabilize your body when you walk.
The nerve to the piriformis muscle provokes the muscle to move your thigh away from your body.
Sensory Function
The sensory fibers of the sacral plexus obtain nerve transmissions from the skin, joints, and muscles. These messages are sent up via the nerves of the sacral plexus and to the spine, where they travel in the dorsal (back) column of the spine and up to the sensory areas of your brain to make you conscious of your senses.
Sensory nerves of the sacral plexus include:
Posterior femoral cutaneous nerve: This nerve accepts sensory transmissions from the skin on the back of the thigh and leg, as well as the pelvis.
Sciatic nerve: The tibial and common fibular parts of the sciatic nerve both obtain sensory information from the leg. The tibial part accepts sensory information from most of the foot. The common fibular part receives sensory messages from the front and sides of the leg and the back of the foot.
Pudendal nerve: This nerve obtains sensory information from the skin of the genital regions.
Associated Conditions
The sacral plexus, or parts of the sacral plexus, can be impacted by the condition, traumatic damage, or cancer. Because this network of nerves has many components and parts, the symptoms can be confusing. You may participate in sensory loss or pain in areas in your pelvis and leg, with or without muscle weakness. The way might not necessarily correspond to a single nerve, making it challenging to determine which aspects of the sacral plexus are affected.
Imaging investigations, such as pelvic computerized tomography (CT) or magnetic resonance imaging (MRI) may determine cancer or traumatic injuries.
Electrical examinations such as nerve conduction studies (NCV) or electromyography (EMG) can often determine the specific nerve branches that have been damaged or have been impacted by conditions such as neuropathy.
Conditions that impact the sacral plexus include:
Neuropathy: Nerve impairment can affect the sacral plexus or regions of it. Diabetic neuropathy is a nerve disease that results from diabetes, especially diabetes that is not well retained. Neuropathy can also happen due to vitamin B12 deficiency, certain medications (such as chemotherapeutic medications), toxins (such as lead), alcohol, and metabolic illnesses.
Cancer: Cancer occurring in the pelvis or extending to the pelvis from somewhere else in the body can compress or penetrate the sacral plexus, impairing nerve function.
Injury: Traumatic damage to the pelvis can stretch, tear, or harm the nerves of the sacral plexus. Bleeding may compress the nerves, interrupting their function.
Infection: An infection of the spine or the pelvic area may extend to nerves of the sacral plexus or may deliver an abscess inducing symptoms of nerve impairment, as well as pain and tenderness of the infected region.
Clinical relevance
Lesions of the sacral plexus can be generated by pelvic fractures, hip surgery, malignant infiltration, local radiotherapy, and the use of orthopedic traction tables. These lesions are usually unilateral and do not result in powerful sexual dysfunction unless the sensory symptoms become disruptive.
Cancers can plague the sacral plexus causing pain-releasing pain syndromes similar to sciatic nerve lesions. Numbness in the perianal area as well as the involvement of sympathetic fibers causes “hot and dry foot” can be found.
The sacral plexus can be surprised by the fetal head at the pelvic brim during the final trimester of pregnancy or labor. The clinical syndrome will reach L5 radiculopathy and manifestation will usually resolve entirely on its own 4 – 6 months post-birth.
Lumbosacral Plexopathy
A lumbosacral plexopathy is a condition affecting either the lumbar or sacral plexus of nerves. They are irregular syndromes, generated by impairment of the nerve bundles. A plexopathy is asked if the signs cannot be localized to an unattached nerve. Patients may complain of neuropathic pains, numbness or weakness, and wasting of muscles.
One of the main causes of lumbosacral plexopathy is diabetic amyotrophy, also known as lumbosacral radioplexus autophagy. I this condition, high blood sugar levels impair the nerves. Idiopathic plexopathy is another reason, being the lumbosacral match of Parsonage-Turner syndrome (which affects the brachial plexus). Tumors and other local invasions can cause plexopathy due to the reduction of the plexus.
Treatment relies on what is causing the symptoms. For tumors and space-occupying lesions, they should be released if possible. For diabetic and idiopathic reasons, treatment with high-dose corticosteroids can be helpful.
Treatment
Recovery and rehabilitation of a condition or injury of the sacral plexus are possible. In available, rehab is better when the symptoms are caught early and the illness is analyzed before serious nerve injury has occurred. Less comprehensive damage and the involvement of fewer nerve branches are also associated with better healing.
Treatment of the Underlying Medical Problem
Rehabilitation begins with the treatment of the reason for the problem—such as treatment for cancer (surgery, chemotherapy, and/or radiation) or antibiotic treatment for an infection. Treatment of neuropathy is often complicated because the lead may be unclear, and a person can participate in several reasons for neuropathy at the same time. Healing after a major pelvic trauma (such as from a car accident) can take months, particularly if you have had multiple bone fractures.
Motor and Sensory Recovery
Physical therapy and occupational therapy can support you recover your strength and motor control as you are healing from a sacral plexus infection or injury. Adapting to sensory obligations is an important part of rehabilitation and recovery from a sacral plexus problem. Sensory problems can interrupt your ability to walk, as you might not be able to properly feel your position as you are driving.
Sensory deficiencies may make you less susceptible to pain, which can aggravate the consequences of injuries (when you don’t take care of them or bypass further trauma). And occasionally, rehabilitation for bowel and bladder function may need exercises, as well as medication that can help control these functions.
Physiotherapy – patients with severe neuropathic incontinence should first experience intensive conservative treatment including physiotherapy/pelvic floor retraining (biofeedback) before surgical treatment is considered.
Sacral Nerve Stimulation: there is good appearing evidence for the treatment of patients with end-stage fecal incontinence.
FAQ:
What causes damage to the Sacral nerve?
The most common causes of spinal cord injuries to the sacrum are Motor vehicle accidents. Trauma. Cascade.
Does the sacral nerve affect the bladder?
The sacral nerves, located near the tailbone, control the bladder and muscles related to urinary function. However, the bladder can not serve duly, which can beget bladder control problems, If the brain and sacral nerve don’t communicate rightly.
What happens when the sacral plexus is damaged?
A sacral plexus lesion may beget instantiations in the distributions of the gluteal, sciatic, tibial, and peroneal nerves. This manifests in the weakness of the hip extensors, hip abductors, knee flexors, and all bottom and toe functions.
What does the sacral plexus control?
The sacral plexus ( plexularis sacral) is a nerve plexus that provides motor and sensory nerves for the posterior thigh, the utmost of the lower leg, the entire bottom, and part of the pelvis.
What does the sacral plexus give rise to?
The sacral plexus gives rise to one major nerve and six contributory nerve branches. The sciatic nerve exits the pelvis through the lesser sciatic notch and also descends between the lesser trochanter of the femur and the ischial tuberosity.




One Comment