Popliteal Artery Entrapment Syndrome
Table of Contents
Introduction
- Popliteal artery entrapment syndrome (PAES), described by Stuart in 1879, is an uncommon limb-threatening vascular entity comprising approximately 0.17%-3.5% of the common population in the United States (US). This embryological developmental anomaly results mainly from an aberrant relationship of the popliteal artery with the surrounding popliteal fossa myofascial structures. PAES predominantly affects active males without a previous history of cardiovascular disease risk factors. Furthermore, patients with PAES primarily present complaining of intermittent pain in the feet and calves that usually occurs after the exercise or vanishes at rest.
- Moreover, the advances in radiological imaging likewise allowed far good delineation or also enhanced sensitivity in detecting PAES. A combination of magnetic resonance imaging (MRI) with arteriography has been reported to be one of the many accurate diagnostic approaches for PAES. Additionally, the management of uncomplicated PAES usually includes surgical exploration with the addition of fasciotomy, myotomy, and the release of the popliteal artery by sectioning the fibrous bands.
- Likewise, if left not treated the PAES can lead to popliteal artery stenosis (PAS), popliteal artery thrombosis (PAT), as well as distal arterial thromboembolism (DAT). The current article discusses the underlying pathophysiology of PAES, highlights the relevance of a detailed history and also physical examination to illuminate the diagnosis of PAES, and also elaborates on the necessary information that leads to the identification of high-risk patients requiring urgent surgical intervention.
Etiology
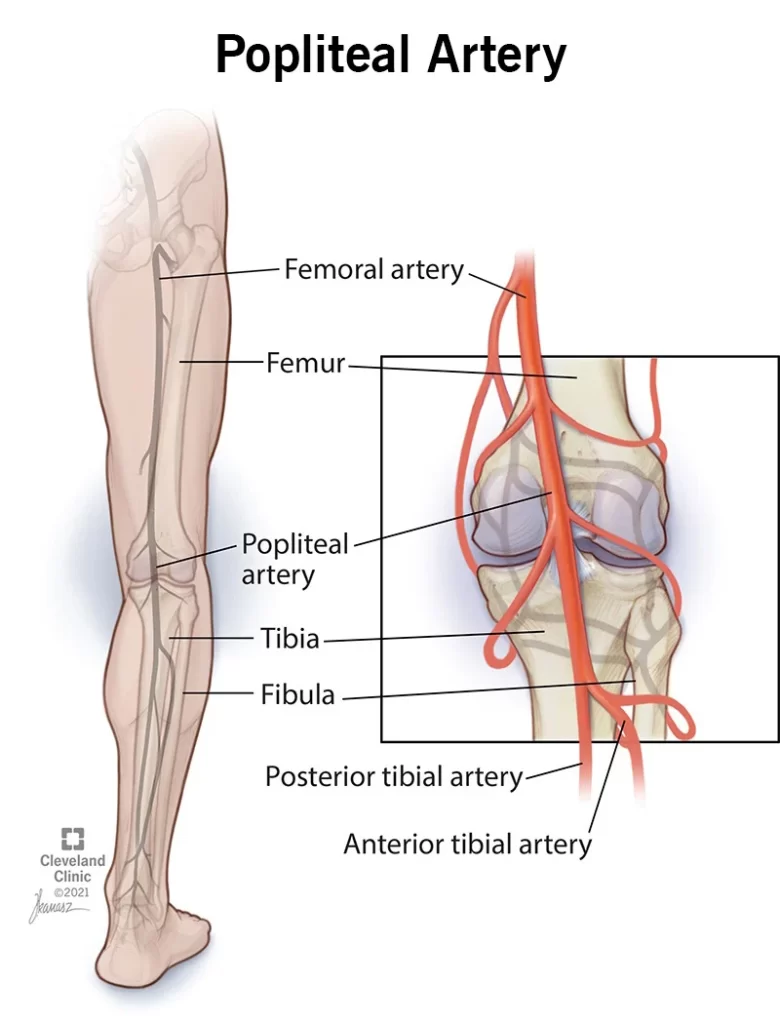
- Both congenital and acquired mechanisms have been proposed in the progress of PAES. An in-depth understanding of the various stages of human embryological progress has successfully demonstrated the precise etiology of congenital PAES. Developmentally, the popliteal artery or the medial head of the gastrocnemius muscle develops at about the same time. Both the femoral and sciatic artery contributes significantly to the development also the popliteal artery. It originates from the extension of the femoral artery proximally or the sciatic artery distally. Mainly, the sciatic artery contributes to the development of the tibial artery as well.
- Over time, the sciatic artery regresses, or the femoral artery becomes the main contributor to the progress of the popliteal artery. The embryological phases of the plantar muscle play a significant contribution to congenital PAES. The plantaris muscle is related to the superficial group of the posterior crural muscular tissues or has a pivotal function in the plantar flexion of the ankle joints. However, this muscle is almost vestigial or assumed to act in combination with the gastrocnemius.
- Furthermore, it reported being aberrant in approximately 10% of the cases as well. When this muscle develops aberrantly, it has the potential to trap the popliteal arteries leading to the sign and symptoms of claudication. Furthermore, different anomalies regarding the relative position of the popliteal artery, medial head of the gastrocnemius muscle(MHG), or popliteus muscles define the multiple types of PAES. Also, the aberrant migration of the main medial head during embryological improvement can result in the malpositioning of the muscles concerning the nearby vessels. Interestingly, most of the people born with this congenital disease anomaly mainly remain asymptomatic, suggesting a likely multifactorial process contributing to disease progression
- Although this pathology is present from birth, it appears late, likely due to changes related to, the use of the main gastrocnemius muscle in activities such as running and marching causing muscles hypertrophy with external compression and impingement of the main popliteal artery by the medial head.
Epidemiology
- Although PAES remains an essential cause of vascular compromise, over the last few decades, the incidence of this uncommon abnormality has increased. In a recent case report published on this different clinical entity, Wady et al. reported the overall incidence of PAES to be in the range of 0.17% to 3.5% common population. Furthermore, 85% of patients affected with this condition are males, with mainly 60% of cases occurring in young athletes during the third decade of life. Moreover, in about 30% of the case, the disease also has a bilaterally symptomatic presentation.
Types
- Generally, the majority of PAES cases are due to embryological anomalies while fewer patients have been documented having acquired (fibrous bands) causes for PAES. Additionally, the PAES are further classified into six different types based on the relationship of the main medial head of the gastrocnemius muscle with the popliteal artery.
- Type I: An aberrant medial course of the main popliteal artery around a normally positioned MHG.
- Type II: MHG attaches abnormally or more laterally on the femur causing the popliteal artery to pass medially and inferiorly.
- Type III: Abnormal fibrous band and accessory muscle arising from the medial or lateral condyle encircling the popliteal artery.
- Type IV: Popliteal artery lying in its primitive deep or axial position within the fossa, becoming compromised by the popliteus muscle and fibrous bands.
- Type V: The entrapment of both the popliteal artery or vein due to any of the causes mentioned above.
- Type VI: Muscular hypertrophy, resulting in a functional compression of main the popliteal artery and vein.
What is mainly popliteal artery entrapment syndrome (PAES)?
- Popliteal artery entrapment syndrome (PAES) is a mainly vascular disease that affects the legs of some young athletes. When you have this syndrome, the muscles behind your knee compress your popliteal artery — the main artery that runs from your thigh to your calf. The attachments of your gastrocnemius muscle to your thigh bone cause compression. When your gastrocnemius muscle contracts during foot plantar flexion movement (pushing down), your muscle compresses your artery.
- During exercise, repetitive compression leads to spasms in your artery. This decreases blood flow. The decreased blood flow leads to a buildup of lactic acid or carbon dioxide in your muscles and nerves, which produces heaviness, achiness, tiredness, and sometimes numbness in your calf muscle and foot. Symptoms typically increased three to five minutes after stopping the exercise. Without treatment, over time, mainly the spasm tends to occur quicker and last longer. Symptoms occur after a shorter distance or it takes longer to recover.
Whom does popliteal artery entrapment syndrome affect?
- PAES occurs mainly often in athletes between the ages of 15 and 25 years old, particularly those who take part in activities or sports that involve running. These include:
- Track.
- Cross country.
- Soccer.
- Lacrosse.
- Field hockey.
How mainly common is popliteal artery entrapment syndrome?
- According to estimates, less than 1% of peoples has PAES. It is difficult to know the true number of people who have this condition.
Are there other main conditions that may mimic popliteal artery entrapment syndrome?
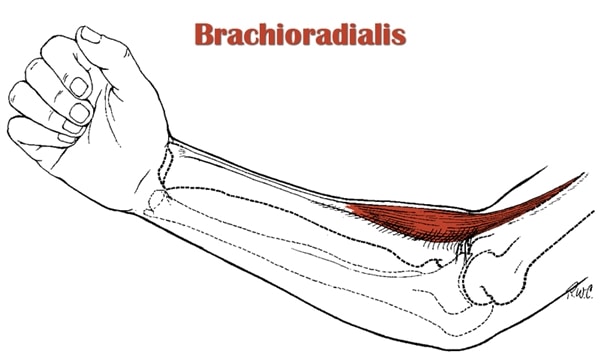
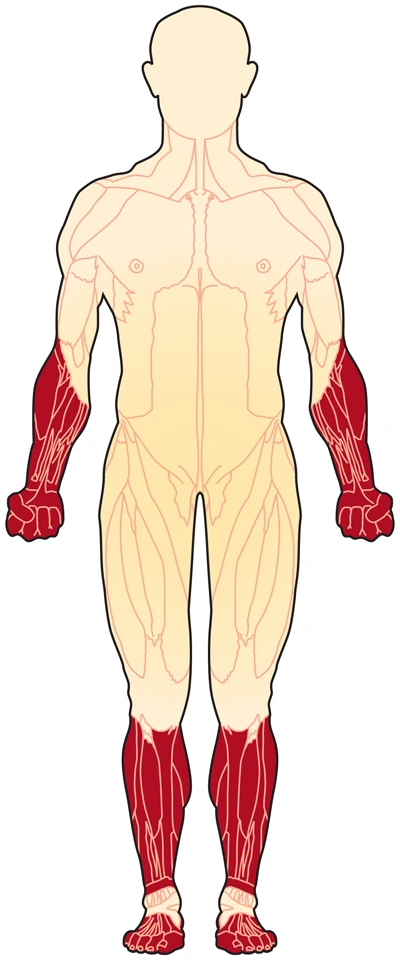
- Chronic exertional compartment syndrome (CECS) is many common conditions that are also an exercise-induced muscle or nerve condition. It causes pain, swelling, or sometimes disability in the affected muscles of your legs and arms. Anyone can develop main the condition, but it is more common in young adult runners or athletes who participate in activities that involve repetitive impact. Many people with popliteal artery entrapment syndrome may also have chronic exertional compartment syndrome. About 5% of people who do not improve after PAES treatment may find they also have CECS. It is possible to have both of these conditions at the same time.
What does main PAES feel like?
- Popliteal artery entrapment syndrome’s main symptoms in your calf and/or foot during exercise may include:
- Aching pain.
- Tiredness.
- Heaviness.
- Cramping.
- Numbness.
- Burning.
- Symptoms typically go away after three or five minutes of rest. Over time (without treatment), the symptoms tend to happen at shorter distances or take longer to go away.
What causes main popliteal artery entrapment syndrome?
There are two main types of compression popliteal artery entrapment syndrome:
- Anatomic compression: This type of compression accounts for about 10% of cases and seems to be many common in people assigned male at birth. It happens mainly in only one leg in about 70% of cases.
- Non-anatomic compression, functional and physiologic compression: These types of compression tends to occur more commonly in people assigned to female at birth. It happens mainly in both legs in more than 90% of cases.
- Anatomic compression:
- This happens because a part of your gastrocnemius muscle crosses over and under your artery. A tendinous band of your muscles can damage your artery. This leads to:
- An ulcer and sore in your artery.
- The buildup of a clot.
- Eventual occlusion (closing or blocking) of your artery and downstream arteries.
- There are four many different variants of the muscle location in relation to your artery.
- Non-anatomic compression, functional and physiologic compression
- Your muscles are all in the normal location, but typically insert higher up your thigh bone and on the inside notch of your thigh bone at the knee. This pulls your muscle to the inside with the plantar flexion compressing the muscle against your artery.
- A muscle mainly located underneath your artery (popliteus muscle) acts as another point of compression. Researchers do not associate physiologic compression with damage to your artery.
Radiographic features
Ultrasound
- May show arterial compression elicited by maneuvers such as plantar flexion or dorsiflexion 5. Doppler may demonstrate an improvement in peak velocity 8.
CT Scan
- CT angiography can help identify abnormal tendinous and muscular structures, diastasis between the popliteal artery or vein, an insertion anomaly, and/or arterial deviation. Aberrant muscular and fibrous attachments can be unique in almost every case and it is best evaluated on axial images.
MRI
- MRI is the best imaging modality to demonstrate the underlying anatomic types of entrapment, which helps guide surgical management 4. A medial slip of the mainly medial head of the gastrocnemius may be seen, compressing the popliteal artery.
Angiography (DSA)
- Lower limb angiography usually demonstrates medial deviation/compression mainly of the popliteal artery when the ankle is plantarflexed. Occlusion of the vessels with thrombus can be mainly seen in the acute presentation. Usually, the collateral vessels are present. Even slight irregularity of the vessels can indicate a degree of entrapment 2.
How do you test for main popliteal artery entrapment syndrome?
- Diagnostic tests measure blood flow through your knee, leg, or foot. Imaging can show:
- Normal artery.
- An ulcer forms mainly in your artery.
- Blood clots.
- Aneurysm of your arteries (dilation of the blood vessel to 50% of normal size).
- Muscles compress your artery.
Tests may include:
- Ankle-brachial index with exercises: This test measures the blood pressure in your arms or legs before and after exercise.
- Normally, your blood pressure is the same in your arms and legs, or both rise with exercise. When running causes a spasm in your arteries, leg blood pressure drop after exercise to less than 90% of the arm pressure.
- Duplex ultrasound of the popliteal artery with plantar flexion: These tests use sound waves to image your artery or measure blood flow. It allows your provider to look at the arteries of your leg with plantar flexion or at rest to see muscle compression.
- Computed tomographic angiography (CTA) with plantar flexion: This is a type of CT scan that uses dye to look at your leg’s arteries with plantar flexion or at rest to see muscle compression.
- Magnetic resonance angiography (MRA) with plantar flexion: This test uses a magnetic field or pulses of radio wave energy to
- look at your leg arteries with plantar flexion or at rest to see muscle compression.
Differential Diagnosis
- Various surgical and non-surgical conditions mimic the PAES which adds an additional challenge in diagnosing this limb-threatening condition.
- Chronic exertional compartment syndrome
- Medial tibial stress syndrome
- Fibular stress fractures
- Tibial stress fractures
- Fascial defects
- Nerve entrapment syndrome
- Referred pain from the lumbar disc herniation
How is mainly PAES treated?
- Your healthcare provider can do surgery to remove a small portion of your gastrocnemius or popliteus muscle. This eliminates the compression of your artery or allows normal blood flow to your leg. The popliteal artery entrapment main syndrome surgery takes about an hour. You all be asleep under general anesthesia during the procedure.
- In more advanced cases of anatomic popliteal entrapment when the popliteal artery is damaged or blocked, your surgeon may need to clean out the artery and patch it or perform a bypass around the blocked part of the artery to re-establish blood flow.
- Surgery is the preferred treatment for popliteal artery entrapment syndrome because it gives excellent results for many people. More than 90% of people who have the surgery have good improvement in their symptoms afterward.
- The only non-surgical treatment mainly for the functional type of PAES uses injections of Botulinum toxin A. With CT and ultrasound guidance, your provider injects Botox® or Dysport® into the muscle that’s causing the compression. This temporarily paralyzes the muscle that is causing symptoms in hopes that the muscle shrinks permanently. However, this effect only lasts for three or six months. If the muscle does not get smaller, the symptoms will happen again. This has been a success in less than 60% of people a year after treatment.
How long does not it take to recover from this treatment?
- The main popliteal artery entrapment syndrome recovery time after surgery is four to six months. You all need to stay in the clinic overnight after your surgery. Then you may do main physical therapy (stretching and flexibility exercises) for the first two weeks as an outpatient to help you recover. After two weeks, you all do strength or conditioning exercises until you recover completely.
Prognosis
What can I expect if I have popliteal artery entrapment syndrome?
- If you have functional popliteal entrapment or your symptoms of leg pain with exercise are bothersome, you can limit your exercise activity. However, surgical treatment is great in more than 90% of people and it’s unlikely that they all have symptoms again. Many athletes return to normal activity after surgery.
- For anatomic entrapment, providers recommend mainly surgical removal of the abnormal muscle slips to prevent arterial damage that can occur over time. If you do not get treatment until after anatomic PAES has damaged your popliteal artery, you could be at risk of always having pain in your legs when you walk. It is possible to need to have a leg removed. However, this is mainly rare.
FAQ:
Surgery is the only way to correct the abnormal calf muscle or free the trapped artery. Your doctor will likely recommend surgery if your symptoms significantly affect your everyday and athletic activities.
As a secondary effect, in the long term, repetitive trauma to the artery in its abnormal course can physically damage the arterial wall and cause a progressive narrowing also known as stenosis. In many severe cases, permanent damage to the muscles or nerves of the leg is possible.
Popliteal artery entrapment syndrome occurs when the main popliteal artery, the main artery for the lower body, is compressed by muscles behind the knee, restricting blood flow through the legs. People with this condition develop pain with walking and during strenuous exercise.
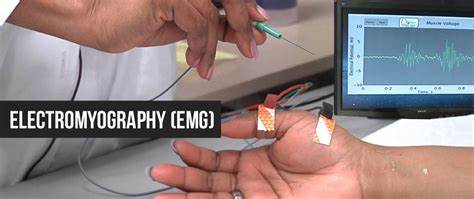
Ultrasound. Mainly Ultrasound is an initial screening examination to assess for entrapment. The popliteal artery is interrogated from above the knee joint to bifurcation, using a linear 12 MHz and 9 MHz vascular transducer.
To ‘unlock’ the knee, the popliteus muscle needs to contract, causing flexion or lateral rotation of the femur on the tibia, thereby giving the muscle the term – ‘key’ to the locked knee.