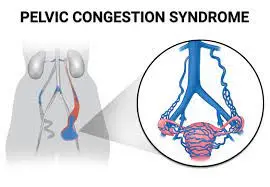
Pelvic Congestion Syndrome
Table of Contents
What is a Pelvic Congestion Syndrome?
Pelvic Congestion Syndrome (PCS) is a condition that is seen mainly in women when the veins in the pelvic region become swollen and engorged. This can result in chronic pain and discomfort in the lower abdomen, pelvis, lower back, and legs. Pelvic Congestion Syndrome is also known as ovarian vein reflux syndrome or pelvic venous insufficiency.
- The disorder known as Pelvic Congestion Syndrome (PCS) causes persistent pelvic discomfort because compromised ovarian veins cause blood to flow backward rather than forward or upward toward the heart. Due to discomfort brought on by venous distension and congestion, an inadequate or ineffective vein valve in the pelvic area is also linked to PCS. Ovarian varicocele and “varicose veins of the ovaries” are other terms and phrases connected to this illness.
- A chronic illness known as pelvic vein incompetence or pelvic congestion syndrome is thought to be caused by swollen veins in the lower abdomen. The problem may result in persistent pain, such as a dull aching that never goes away and is made worse by standing or having sex.
Prevalence
- Women who are older or of reproductive age seem to experience this problem more frequently. The majority of afflicted women have a history of having multiple pregnancies. Men can also get this condition, which can be identified by the presence of obvious varicosities on the scrotum Cavallo. Additionally, it is the reason for roughly 10 to 15 percent of referrals to gynecologists or other pain clinics.
Symptoms of Pelvic Congestion Syndrome
- The pelvic congested syndrome may not have any symptoms and frequently goes undetected. Lower abdomen or pelvic discomfort, varying in intensity from a dull ache to a sharp, acute pain, can be a constant or sporadic symptom of this illness. Pain may last for longer than six months. PCS-related lower abdomen or pelvic discomfort may be experienced unilaterally, on one side, or bilaterally. The discomfort typically gets worse at night and after spending a lot of time standing or sitting. Additionally, the beginning of menus may be connected to discomfort.
The following list of additional PCS symptoms is provided:
- Ovarian point tenderness with thorough palpation
- Dyspareunia
- lower extremities or the buttocks having varicose veins
- Headache
- gastrointestinal discomfort or pain
- bowel and bladder changes
- Fatigue
- Insomnia
- The feeling of heaviness in the lower abdomen or the pelvis
- The ache in my lower back got worse when I stood up.
- Lethargy
- Depression
- Virulent discharge
- Dysmenorrhea
- enlarged vulva
- A lumbar neuropathy
- Uncomfortable rectus
Signs and symptoms
- The chronic pain that many women suffer may be mild and painful, but it can also occasionally be more severe. Those who experience it find comfort when they lie down. The pain is greatest at night and after extended periods of standing. The discomfort is greatest before the start of the menstrual cycle, during, or just after sexual activity.
- The uterus and endometrium are thicker in women who have pelvic congestion syndrome. 56% of women experience cystic ovaries, and many also experience dysmenorrhea, back pain, vaginal discharge, abdominal bloating, mood swings or sadness, exhaustion, and other symptoms.
Causes of Pelvic Congestion Syndrome
- Women who give birth to two or more children (multiparous) may be more prone to PCS. A woman’s intravascular volume might rise by as much as 60% throughout each pregnancy. Venous distension can occur as intravascular volume rises. Valvular incompetencies can develop in ovarian veins that have undergone severe distension, which can lead to PCS. Additionally, it has been proposed that estrogen may contribute to the thinning of venous walls. As a result, while managing hormones therapeutically, caution should be given.
- Anatomical malformations with an obstruction-like character can also produce PCS. Pelvic varices can develop as a result of an ovarian vein being blocked by a retro aortic renal vein [3]. The renal or ovarian vein may experience compression from the superior mesenteric artery. The term “Nutcracker Syndrome” has been used in the literature to characterize this specific compression [3]. Between the spine and the pelvic brim, the common iliac vein may experience additional compression from the common iliac artery. Iliofemoral deep vein thrombosis or even pelvic varices may arise from the compression cascade that follows.
- Additionally, PCS might occur as a result of surgical complications. Nephrectomy is the procedure most commonly associated with surgery. The danger of damaging the ovarian vein during this surgery is enhanced.
- Local hormonal pelvic environment
- Venous outflow blockage, such as that caused by left renal vein thrombosis, the May-Thurner syndrome, the Nutcracker syndrome, or the Buddy Chiari syndrome.
- External compression brought on by a tumor (including endometriosis or fibroids) or scarring
Diagnosis
- Testing by laparoscopy or ultrasound can be used to get a diagnosis. In addition, a venogram, CT scan, or MRI can be used to identify the illness. The most often employed diagnostic tool is ultrasound. According to several studies, transvaginal duplex ultrasonography is the most effective diagnostic to diagnose pelvic venous reflux.
- Due to the supine posture that is frequently utilized for testing and may result in a reduction in venous distention, Pelvic Congestion Syndrome is frequently overlooked. Laparoscopy, hysteroscopy, or other imaging procedures (such as computed tomography, magnetic resonance imaging, or ultrasound) can detect the presence of PCS.
- As additional criteria for sonographic diagnosis.
- pelvic veins with varicose veins, such as:
- Pelvic While computed tomography is used to diagnose varicose veins in the lower abdomen area and is more sensitive than ultrasonography, ultrasound gives a more dynamic view of the blood flow.
- more than 4-mm-diameter ovarian veins
- Retrograde blood flow is reduced by 3 cm/s, along with dilated and tortuous
- Arcuate veins that connect with bilateral pelvic veins, especially the left ovarian vein.
Treatment of Pelvic Congestion Syndrome
Medical Management
The primary line of treatment for PCS is analgesics, which includes non-steroidal anti-inflammatory medicines for pain control. If symptoms do not go away or become better after taking medication, a referral to an interventional radiologist may be necessary. Embolization of the problematic arteries is the most effective medical treatment for PCS, with a success rate of 98–100%. An interventional radiologist may lessen or eliminate PCS symptoms by the outpatient technique of embolization of varices. Only after the doctor has conducted a full history take, physical examination, and assessment of imaging is this surgery carried out. The surgery is carried out under anesthesia and is guided by imaging while the patient is asleep. 2-4 weeks after surgery, there should be a reduction in symptoms, which has been seen in 75-80% of patients.
Ignacia and associates identified a number of medicinal interventions for PCS, such as:
- Analogs of hormones
- surgical ovarian vein ligation
- Hysterectomy
- Using a catheter to embolize
- psychological counseling
- Progestins
- Phlebotomists
- Combined hormone replacement treatment (HRT) with gonadotropin receptor agonists (GnRH)
- Dihydroergotamine
- NSAIDS
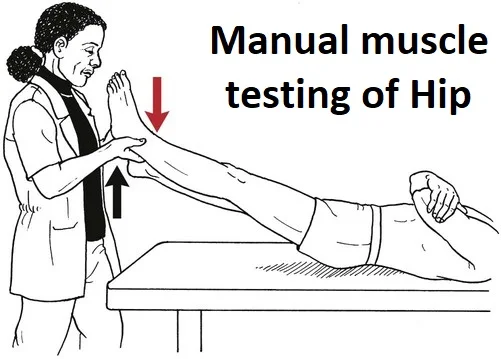
Physical Therapy Treatment
Physical therapy’s function in PCS treatment has not yet been the subject of any literature. Regardless, someone with persistent discomfort or incontinence difficulties may look for a physical therapist that specializes in pelvic dysfunction. Based on a person’s disabilities, a physical therapist will be able to do a complete examination and create a rehabilitation program. The muscle of the pelvic floor might be impacted often as a result of PCS’s near proximity. In this situation, physical therapists might offer particular workouts to enhance the pelvic floor musculature’s optimal performance.
Differential Diagnosis
Due to the clinical presentation, PCS has a long list of differential diagnoses that must be eliminated before the diagnosis can be made.
- GI Pathology
- Cancer
- Endometriosis
- Fibroids
- Fibromyalgia
- ovarian cancer
- Pelvic Disorder with Inflammation
- Porphyria
- Abdominal Prolapse
- The pathology that is orthopedic, neurological, or orogenic
- Leiomyoma
- Adenomyosis
- Case of the Nutcracker
- Bowel Inflammation Syndrome
- Meckel’s diverticulum, diverticulitis, and diverticulosis
- Cystitis interstitial
- Fascitis
- Mental and sexual dysfunction
- Depression
FAQ
What contributes to pelvic congestion syndrome?
Similar to varicose veins in the legs, pelvic congestion syndrome happens when varicose veins form around the ovaries. The vein valves stop working normally after that. Backflow of blood results from this.
Can pelvic obstruction be treated?
Although there is no known treatment for pelvic congestion syndrome, medicines, and surgical treatments can help you feel better.
How is pelvic obstruction identified?
A pelvic venogram is carried out by injecting X-ray dye into the pelvic veins to make them visible on an X-ray and is considered the most accurate technique of diagnosis. The best non-invasive technique to diagnose pelvic congestion syndrome may be an MRI.
How much pelvic congestion be treated without medication?
As it maintains blood flow, exercise can assist to reduce congestion and fluid gathering in the pelvic region. It might be better to go for a brisk early run or stroll because there is typically less discomfort and congestion then. Cycling or swimming may also be suitable substitutes.
What is a syndrome of 3 pelvic congestion?
Women of reproductive age frequently have persistent pelvic discomfort due to pelvic congestion syndrome (PCS). Chronic pelvic pain is defined as abdominal or pelvic discomfort that lasts for three to six months, is present, occurs throughout the menstrual cycle, and has no connection to pregnancy.



One Comment