Femoroacetabular Impingement
Table of Contents
What is a Femoroacetabular Impingement?
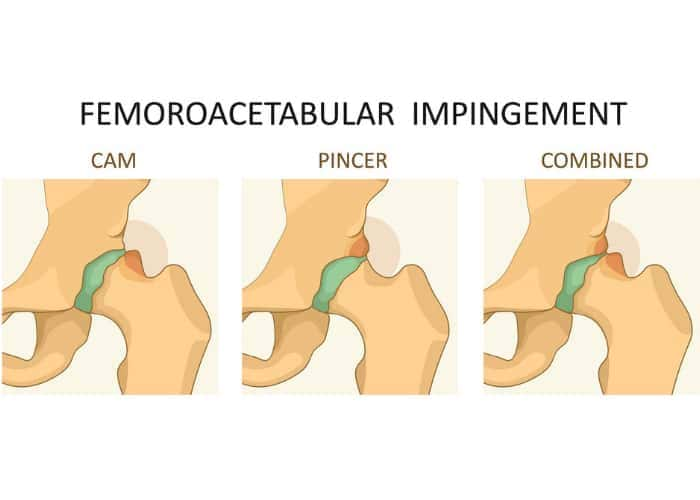
Femoroacetabular impingement (FAI) is a condition where the bones of the hip joint are abnormally shaped, causing friction and limited movement in the hip joint. It can lead to pain, and discomfort, and potentially contribute to hip joint damage. FAI is often categorized into three types: cam impingement, pincer impingement, and mixed impingement.
- Pincer Impingement: In pincer impingement, the hip socket (acetabulum) extends too far over the femur bone head. This excessive coverage can result in pinching of the soft tissues in the hip joint, causing pain and reduced mobility.
- Cam Impingement: This type occurs when the femoral head (the ball-shaped end of the thigh bone) has an irregular shape, usually resembling a cam or bump. This can lead to friction and limited hip movement when the femoral head rubs against the hip socket.
- Mixed Impingement: This type is a combination of both cam and pincer impingement, where there are abnormalities in both the femoral head and the acetabulum.
Causes of Femoroacetabular Impingement
- Genetics: There is evidence to suggest that genetic factors can play a role in the development of FAI. If someone has a family history of hip abnormalities or FAI, they might be more predisposed to developing the condition.
- Abnormal Hip Development: During childhood and adolescence, the hip joint undergoes growth and development. If there are disruptions or irregularities in this process, it can lead to the formation of abnormally shaped hip bones, increasing the risk of FAI.
- Hip Joint Mechanics: Certain activities or movements that involve repetitive hip flexion, rotation, or extreme ranges of motion can contribute to the wear and tear of the hip joint, potentially leading to the development of FAI.
- Sports and Physical Activities: Athletes who participate in sports that involve frequent hip movements, such as soccer, hockey, ballet, and martial arts, may be at a higher risk of developing FAI due to the repetitive stresses placed on the hip joint.
- Sedentary Lifestyle: Prolonged periods of sitting and lack of regular physical activity can affect hip joint mechanics and potentially contribute to the development of FAI.
- Hormonal Factors: Hormonal changes during growth spurts and puberty might influence the development of bone structures and contribute to the formation of abnormal hip shapes.
- Injury: Trauma or injury to the hip joint, especially during periods of rapid growth, can disrupt the normal development of the hip bones and increase the risk of FAI.
- Joint Disorders: Certain conditions, such as hip dysplasia (a misalignment of the hip joint), can alter the shape of the hip bones and lead to FAI.
Symptoms of Femoroacetabular Impingement
- Hip Pain: Persistent pain in the groin area, hip joint, or buttocks is a hallmark symptom of FAI. The pain might be dull, aching, or sharp, and can worsen with certain movements or activities.
- Limited Range of Motion: Individuals with FAI might experience restricted hip movement, particularly during activities that involve flexing, rotating, or moving the hip joint.
- Stiffness: Stiffness and discomfort in the hip joint, especially after periods of rest or inactivity, can be a symptom of FAI.
- Pain with Sitting or Driving: Prolonged sitting, especially in positions that flex the hip joint, can exacerbate hip pain and discomfort in individuals with FAI.
- Clicking or Snapping Sensation: Some people might notice a clicking, snapping, or catching sensation in the hip joint when moving, which could be due to the bones rubbing against each other.
- Pain during Physical Activities: Activities that involve running, jumping, or squatting might trigger or worsen hip pain and discomfort.
- Painful Activities: Certain movements, such as crossing the legs, putting on socks, or getting in and out of a car, can cause pain in individuals with FAI.
- Muscle Weakness: Weakness in the muscles surrounding the hip joint might develop due to pain and limited mobility.
- Radiating Pain: In some cases, hip pain might radiate to the thigh or knee.
Diagnosis
The diagnosis of femoroacetabular impingement (FAI) typically involves a combination of medical history, physical examination, and diagnostic imaging.
Medical History: The healthcare provider will start by asking about the individual’s symptoms, including the location and nature of the pain, any activities that trigger or worsen the pain, and how long time the symptoms have been present.
Physical Examination: The doctor will perform a physical examination to assess the range of motion in the hip joint, as well as any signs of discomfort or pain during specific movements. They might also conduct tests to determine if certain positions or actions elicit pain.
Imaging: Diagnostic imaging plays a crucial role in confirming the presence of FAI and assessing its severity.
- X-rays: X-rays can help visualize the hip bones and identify any abnormalities, such as irregularities in the femoral head or acetabulum, characteristic of FAI.
- MRI (Magnetic Resonance Imaging): MRI scans provide detailed images of the soft tissues and structures within the hip joint. This can help assess the extent of damage or abnormalities and rule out other possible causes of hip pain.
- CT (Computed Tomography) Scan: CT scans can provide three-dimensional images of the hip joint, allowing for a more detailed assessment of bone structures and potential impingement.
Diagnostic Injections: In some cases, a diagnostic injection of a local anesthetic into the hip joint might be performed. If the injection provides temporary relief from pain, it could indicate that FAI is contributing to the discomfort.
Differential Diagnosis
- Hip Labral Tear: A tear in the labrum, a ring of cartilage that surrounds the hip socket, can cause symptoms similar to FAI. Labral tears can result from trauma or repetitive stress on the hip joint.
- Osteoarthritis: Hip osteoarthritis can lead to pain, stiffness, and limited mobility. While FAI can contribute to the development of arthritis, they are distinct conditions.
- Trochanteric Bursitis: Inflammation of the bursa, a fluid-filled sac that cushions the hip joint, can cause pain on the outer side of the hip.
- Hip Flexor Strain: Straining the hip flexor muscles, which help with hip movement, can cause pain and discomfort in the front of the hip and groin.
- Inguinal Hernia: This occurs when a portion of the intestines or other tissues protrudes through a weak spot in the abdominal wall, causing pain and discomfort in the groin area.
- Stress Fracture: A stress fracture of the hip joint or pelvis joint can cause pain that worsens with activity and eases with rest.
- Referred Pain: Conditions affecting the lower back or spine, such as herniated discs, can cause pain that radiates to the hip and groin area.
- Muscle Strain: Straining muscles around the hip or pelvis, such as the adductors or hamstrings, can lead to pain that can be mistaken for FAI.
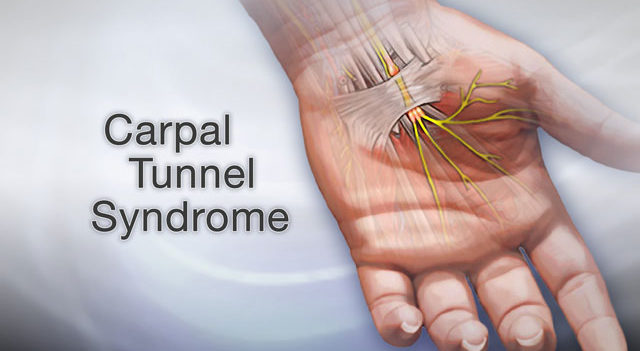
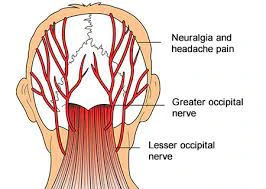
- Nerve Impingement: Conditions like sciatica or meralgia paresthetica can cause nerve-related symptoms that radiate into the hip and thigh.
- Iliotibial Band Syndrome: Irritation of the iliotibial band, a thick band of tissue that runs along the outer side of the thigh, can cause hip pain, especially in runners.
Medical Treatment of Femoroacetabular Impingement
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs can help manage pain and inflammation associated with FAI. However, they are typically used as a short-term solution and might not address the underlying issue.
- Injections: Injections of corticosteroids may offer momentary relief from hip pain and inflammation. These injections are typically administered by a healthcare professional and might be considered if conservative measures alone are not sufficient.
Physiotherapy Treatment
In order to effectively treat FAI, physical therapy is essential. Therapists can design exercises to improve hip joint mobility, strengthen muscles around the hip, and correct movement patterns that might be contributing to impingement.A physical therapist can provide guidance on proper movement techniques and activity adjustments.
- Hip Mobility Exercises: Physiotherapists will design a range of motion exercises to improve the flexibility and mobility of the hip joint. These exercises might involve gentle stretching and controlled movements.
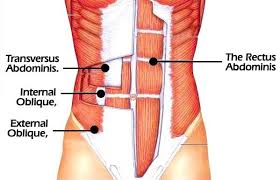
- Strengthening Exercises: Strengthening the muscles around the hip joint, including the hip flexors, abductors, and rotators, can help stabilize the joint and improve its function. Strengthening exercises might involve resistance bands, bodyweight exercises, or the use of exercise equipment.
- Core Strengthening: Strengthening the core muscles can help improve overall stability and posture, which can indirectly benefit the hip joint by reducing unnecessary stress.
- Proprioception and Balance Training: These exercises help improve the body’s awareness of its position in space and enhance balance, which is important for hip joint stability during various activities.
- Functional Training: Physiotherapists often design exercises that mimic real-life movements and activities, helping individuals regain the ability to perform daily tasks without exacerbating their symptoms.
- Manual Therapy: Hands-on techniques such as joint mobilization and soft tissue massage can help alleviate pain, improve joint mobility, and reduce muscle tension.
- Postural Correction: Addressing poor posture can help reduce strain on the hip joint and prevent exacerbation of symptoms.
- Activity Modification: Physiotherapists provide guidance on modifying activities and movement patterns to reduce hip joint stress while allowing individuals to remain active.
- Pain Management Techniques: Physiotherapists can teach techniques for managing pain, such as ice or heat application, and provide advice on pain relief strategies.
- Education: Educating individuals about their condition, proper body mechanics, and strategies for preventing future issues is an essential component of physiotherapy.
- Assistive Devices: Using crutches or other assistive devices can help reduce weight-bearing on the affected hip, allowing it to rest and heal.
Exercise
- Hip Flexor Stretch: Kneel position on one knee with the other foot on the front side, keeping both knees at a 90-degree angle position. Gently shift your weight forward to stretch the hip flexors of the back leg.

- Hip Abduction Exercise: Lay on your side, with the leg that is hurting on top. raise the top leg upward while keeping it straight, then lower it back down. This helps strengthen the hip abductor muscles.
- Clamshell Exercise: Lie on your side with both knees bent. Keep your feet touching and open your knees like a clamshell, then close them again. This targets the muscles on the side of the hip.
- Glute Bridge: Lie on your back with your knees flexed and feet flat on the ground. Lift your hips off the ground by squeezing your glute muscles and driving through your heels.

- Seated Hip Stretch: Sit on the edge of a chair and cross the affected ankle over the opposite knee. Gently press down on the crossed knee to stretch the hip.
- Piriformis Stretch: Lie on your back and cross the affected leg over the opposite knee. Pull the lower knee toward the patient’s chest to stretch the piriformis muscle.
- Wall Squats: Stand against a wall with your feet hip-width apart and about 2 feet away from the wall. Slide down the wall into a squat position, keeping your knees aligned with the patient’s toes.
- Sidelying Leg Lift: Lie on your unaffected side with your legs extended. Lift the affected leg upward, keeping it straight. Lower it back down.

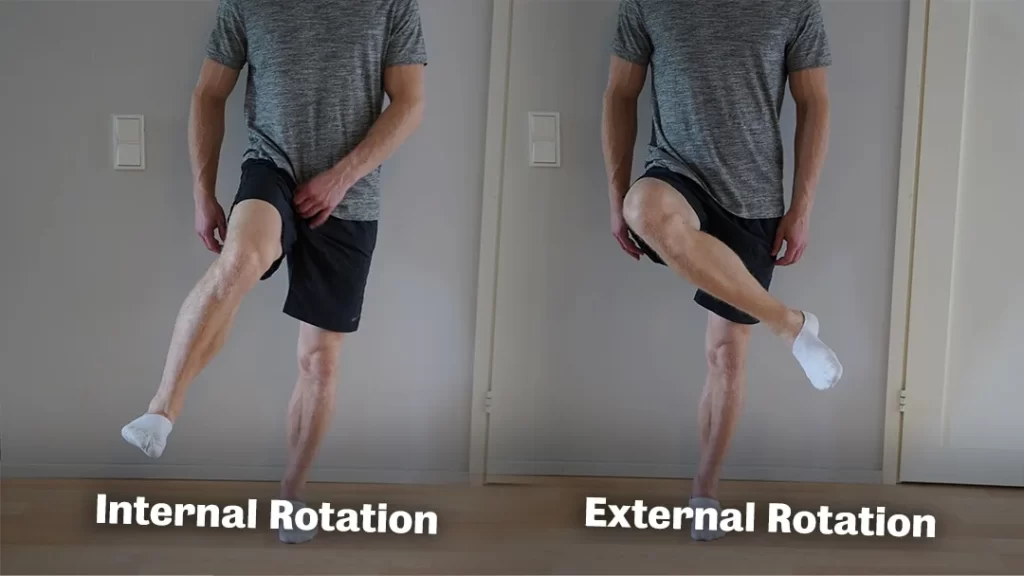
- Internal and External Rotation: Sit on a chair with a resistance band around your thighs. Gently press your knees outward against the band for external rotation, and then press them inward for internal rotation.
- Standing Hip Abduction: Stand while holding onto a stable surface. Lift the affected leg out to the side while keeping it straight. Lower it back down.

- Hip External Rotation Stretch: Lie on your back with both knees flexed. Cross the affected ankle over the opposite knee and gently press the crossed knee away from your body to stretch the outer hip.
- Lunges: Take a step forward with the unaffected leg and lower your body into a lunge position. Make sure the patient’s knee does not go beyond your toes. Push back to the initial position and repeat the exercise.

- Single-Leg Balance: Stand on the unaffected leg while lifting the affected leg off the ground. Hold this position, maintaining your balance, for a set duration. You can use a stable surface for support if needed.

- Step-ups: Using a sturdy step or platform, Step up with the unaffected leg and lift the affected knee toward your chest. Step back down and repeat.

- Mini-Band Walks: Place a resistance band around your ankles. Keep the band taut while moving sideways in short movements. The hip abductor muscles are the focus of this.
- Prone Leg Raises: Lie on your stomach and lift the affected leg off the ground while keeping it straight. Lower it back down and repeat.

- Hip Hinge: Stand with your feet hip-width apart. Hinge at your hips and lower your upper body forward while keeping your back straight. Return to the upright position.

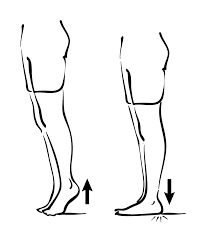
- The calf Raises Standing position on the edge of a step or platform with the patient’s heels hanging off the edge. Rise up onto the patient’s toes, then lower heels below the step level.
- Standing Hip Flexor Stretch: Stand next to a sturdy surface for balance. Bend the affected knee and hold your ankle behind you, bringing your heel toward your glutes to stretch the front of your hip.
- Cross-Legged Sitting Stretch: Sit on the floor with your legs crossed. Gently press down on the affected knee to stretch the hip.
- Bridging with Leg Lift: Perform a glute bridge while lifting the affected leg straight up toward the ceiling. Lower the leg and then lower your hips back to the ground.

Surgery
Surgery is an option for individuals with femoroacetabular impingement (FAI) when conservative treatments have not provided sufficient relief from symptoms or when there is significant joint damage.
- Hip Arthroscopy: This minimally invasive procedure involves making small incisions around the hip joint and using a camera (arthroscope) to guide the surgeon. Through these incisions, the surgeon can reshape the bones, repair damaged cartilage or labrum, and address any other issues contributing to impingement. Arthroscopy tends to have shorter recovery times compared to traditional open surgery.
- Open Hip Surgery: In more severe cases of FAI, or when additional procedures are needed, an open surgical approach may be considered. This involves a larger incision, which provides the surgeon with direct access to the hip joint. Open surgery might be chosen if there are complex or extensive bone abnormalities that cannot be addressed adequately through arthroscopy.
Prevention
- Maintain a Healthy Weight: Excess weight can place additional stress on the hip joint. This stress can be lessened by maintaining a healthy weight with a balanced diet and regular exercise.
- Stay Active: Engaging in regular physical activity helps keep the muscles around the hip joint strong and flexible. Focus on exercises that promote hip mobility and stability.
- Warm Up and Cool Down: Properly warming up before exercise and cooling down afterward can help prevent strains and injuries to the hip and surrounding muscles.
- Proper Technique: Whether you’re engaging in sports, exercise, or daily activities, using proper technique and body mechanics can reduce the risk of undue stress on the hip joint.
- Avoid Overuse: While staying active is important, avoid excessive or repetitive activities that could lead to hip joint overuse and potential damage.
- Listen to Your Body: If you experience hip pain or discomfort during activities, it’s important to address it promptly. Ignoring pain could exacerbate any underlying issues.
- Proper Footwear: Wearing appropriate footwear that provides support and cushioning can help reduce stress on the hip joint during various activities.
- Cross-Training: Engage in a variety of exercises and activities to prevent overloading specific muscle groups or joints.
- Maintain Good Posture: Proper posture can help distribute body weight evenly and reduce strain on the hip joint.
- Stay Hydrated: Staying hydrated supports overall joint health and helps maintain cartilage integrity.
- Limit Prolonged Sitting: If your lifestyle involves a lot of sitting, take breaks to stand, stretch, and move around to prevent stiffness in the hip joint.
- Consult a Professional: If you have concerns about your hip joint or any discomfort, consult a healthcare professional. Early intervention and appropriate guidance can help prevent potential issues.
Home Advice
- Rest and Modify Activities: Avoid activities that worsen your hip pain, especially those involving repetitive hip movements or high-impact exercises. Modify your daily activities to reduce strain on your hip joint.
- Ice and Heat Therapy: Applying ice packs for 15-20 minutes several times a day can help reduce inflammation and pain. Heat therapy might help relax muscles; alternate between ice and heat if it provides relief.
- Pain Management: Over-the-counter pain relievers like ibuprofen or acetaminophen can help alleviate pain and inflammation. However, consult a doctor before using them regularly.
- Gentle Stretching and Strengthening: Consult a physical therapist for exercises that can help improve hip flexibility and strengthen the surrounding muscles to provide better support to the joint.
- Maintain a Healthy Weight: Excess weight can place additional stress on the hip joint. Maintaining a healthy weight can help reduce pressure and discomfort.
- Ergonomics: Ensure your workstations and seating arrangements are ergonomic to promote proper posture and minimize strain on your hips.
- Proper Footwear: Wearing supportive shoes with cushioning can help alleviate hip pain. Avoid high heels or shoes that contribute to poor posture.
- Avoid Prolonged Sitting: Take breaks if you have a desk job. Walk around and stretch periodically to prevent stiffness.
- Sleeping Position: If your hip pain affects your sleep, try sleeping on your back with a pillow between your knees for support.
FAQ
FAI is a condition where there is abnormal contact between the hip ball (femoral head) and socket (acetabulum), potentially leading to pain and hip joint damage.
FAI is mainly caused by structural abnormalities in the hip joint, such as irregularly shaped femoral heads, deep acetabula, or excessive acetabular coverage.
Common symptoms include hip pain, especially during activities like sitting, squatting, or sports. Limited hip range of motion and clicking sensations might also occur.
People with certain hip anatomy, genetic predisposition, engaging in sports with repetitive hip motions, and those with poor movement mechanics might be at a higher risk.
Diagnosis involves a combination of physical exams, imaging studies like X-rays and MRI, and a review of medical history and symptoms.
Surgical options include hip arthroscopy to reshape the femoral head or acetabulum, and in more severe cases, open surgery to reposition the hip joint.