Congenital Muscular Dystrophy(CMD)
Table of Contents
What is Congenital Muscular Dystrophy (CMD)?
Congenital Muscular Dystrophy like CMD is present at birth. A neonate may have weak muscles or curved spine and joints that are too stiff or loose. Children with CMD may have learning seizures, vision problems, and disabilities. It belongs to a larger group of disorders known as muscular dystrophies. This dystrophy is characterized by weakness and degeneration of various voluntary muscles of the body. This disease affects various muscles and has different inheritance patterns, severity, and ages of onset.
As researchers learned more about the CMD, such as determining many of the particular genes involved, a comprehensive picture of these disorders has appeared. It is a rapidly growing disease family and information about these disorders is constantly changing.
The difference between congenital myopathies and muscular dystrophies is that dystrophies are increasingly and are connected with increased muscle damage with age. Congenital myopathies indicate disorders associated with muscle weakness in the neonatal age group, which could be genetic, metabolic, or other disorders and usually have a non-progressive route. Classification of these groups of disorders is based on findings from muscle biopsy and genetic evaluation. The muscle biopsy findings common for these disorders are muscle fiber atrophy and fibrofatty infiltration of tissue. It is caused by genetic mutations affecting some of the proteins necessary for muscles and sometimes for the eyes and or brain.
Classification:
The sub-types of CMD have been determined through differences in multiple genes. Phenotype, as well as, genotype classifications are used to determine the subtypes.
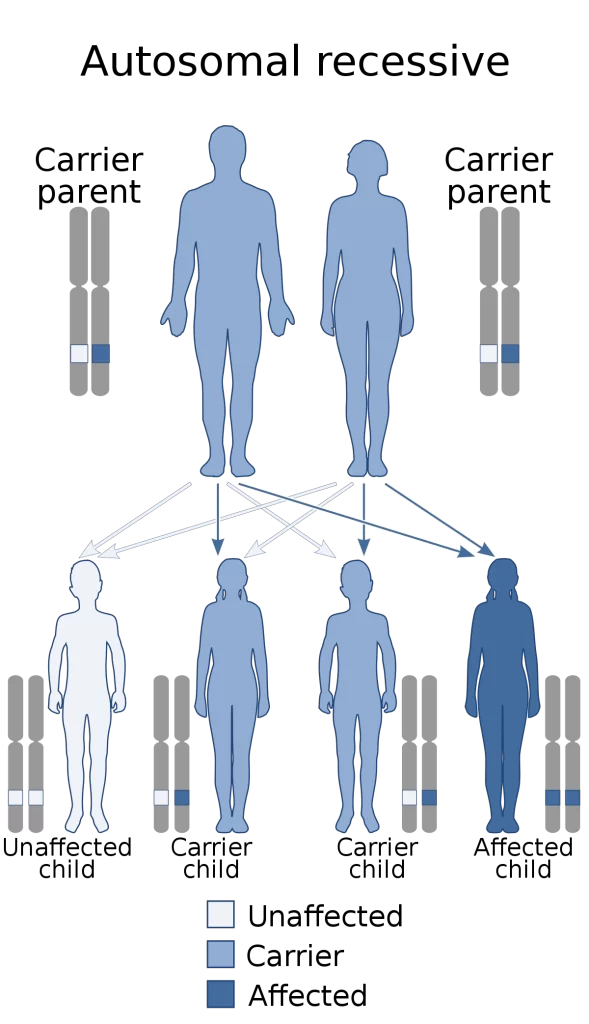
Congenital muscular dystrophies can be either autosomal dominant or autosomal recessive in terms of the heritage pattern, though the latter is much more common.
Congenital muscular dystrophy falls into one of the following types:
CMD with brain-eye: It is also called a muscle-eye-brain disorder. It is an uncommon type of congenital muscular dystrophy (autosomal recessive disorder) cause a lack of normal muscle tone which can delay walking due to weakness, also intellectual disability, and paralysis of eye muscles. This affects the people’s path of reprocessing information. A mutation in the POMGNT1 gene causes it.
CMD with adducted thumbs (drawn inward), is an uncommon type of CMD that cause a lack of muscle tone and permanent shortening of the toe joints. Which can retard walking due to the people being weak. A person with this type of congenital muscular dystrophy might have mild cerebellar hypoplasia in some cases.
CMD/LGMD without MR-first years of a newborn begins with weakness, which affects the walking can be accomplished in adolescence, deformity and motive skills and rigidity of joints. The joints, neck, and spine; gradual cardiomyopathy at an initial age; cardiac rhythm abnormalities may be present in the people.
Large related CMD at the beginning of the newborn time, the issues the infant receives are; weak motor function and poor muscle tone the people will present with intellectual disability and the structure of the brain will be abnormal.
CMD with cerebellar atrophy poor muscle tone, delayed motor milestones, severe cerebellar hypoplasia, involuntary movements, poor muscle tone, lack of coordination in motive skills, difficulty speaking, and some intellectual disability. Furthermore, muscle biopsy does not reveal any deficiency.
Walker–Warburg syndrome at the beginning a gradual low muscle tone and weakness at birth or during initial infancy; small muscles; the majority of affected children do not live more than 3 years of age. With accompanying visual impairment, eye structure problems are present.
CMD with primary laminin-a2 (merosin) deficiency (MDC1A) intellect in such person is unaffected, proximal muscle weakening and rigid spine are present along with respiratory involvement (with disease progression).
CMD/LGMD with MR weakness, rigidity joints and deformity present at birth, poor muscle tone, slowly gradual; people may present with cortical problems (cerebellar cysts), microcephaly may be present as well. Abnormal flexibility and spinal curvature might occur.
CDG I (DPM3) some of the symptoms at birth and throughout the infant’s life are poor muscle tone or weakness and cerebellar cysts. The people may present with no outflow obstruction( cardiomyopathy ), and an increase in serum creatine kinase might be present. Some IQ problems present, along with weakness in the proximal muscles. Also of note, is a reduction of dolichol phosphate mannose.
CDG I (DPM2) weak muscle tone starting in the first weeks of the infant, the people show severe neurologic physical characteristics that result in fatality initial in life. Hypotonia and myopathic facies may be present in such person, while contractures of joints may also be present. Finally, myoclonic seizures may occur at a very initial age (3 months).
CDG Ie (DPM1) at birth the infant will have a weakness with involvement of the respiratory system, as well as, severe psychomotor and mental problems. At the age of 3, people may be blind with speech problems. Microcephaly may occur in the initial stage of childhood, as well as seizures.
Fukuyama CMD-in Western countries this type of CMD is unusual, but it is common in Japan. The effects of this disease on infants are on a spectrum of severity. They include weakness in muscle tone in the first year, seizures, deformation, eye involvement, intellectual disability rigid joints, spinal curvatures, and Some patients may achieve limited walking mobility.
CMD with spinal rigidity present at birth can have weakness and poor muscle tone, reduced respiratory capacity, beginning early ages stabilization, muscles could be deformed or slow decline spinal rigidity, limited mobility to flex the neck and spine, normal intelligence spinal curvature, and progressing deformity and rigidity joints, minor cardiac abnormalities.
CMD with lamin A/C abnormality within the first year the infant is weak, people may have problems after some time lifting arms and head. May need a nasogastric tube, limb weakness, and elevated serum creatine kinase. People may show a diaphragmatic approach when breathing.
Integrin a7 weakness which is present at birth, loss of muscle tissue, poor muscle tone with late walking, and intellectual disability. Furthermore, the creatine kinase level was increased.
Merosin-deficient CMD- the spectrum of severity; may show hypotonia, weakness in muscle tone present at birth, and poor motor development. Most people have periventricular white matter problems. However, intellectual disability is uncommon in most cases.
Merosin-positive CMD some forms of merosin-positive CMD are initial spinal rigidity, CMD with muscle hypertrophy, CMD with muscle hypertrophy, and respiratory failure.
Ullrich congenital muscular dystrophy present at birth is poor muscle tone and weakness,
will have some deformity and rigidity joints, some joints will have respiratory impairment, excessive flexibility, curvature, spinal rigidity, soft skin, normal intelligence, and normal cardiac function.
Causes of congenital muscular dystrophy (CMD):
What causes congenital muscular dystrophy (CMD)?
Muscle cells are included in a web-like structure known as the extracellular matrix (ECM). The ECM is a difficult mix of molecules, including many kinds of proteins linked to glycoproteins (called carbohydrates). Glycoproteins have several functions in the ECM, including connecting individual muscle cells to each other, transmitting the force of muscle contraction to the skeleton, promoting development and repair, and transmitting signals among cells. Many CMDs are occurred to mutations in glycoproteins or in the enzymes that create them. One group of CMDs occurs to mutations in genes that help add sugar molecules to (glycosylate) the protein alpha-dystroglycan, a key glycoprotein of the ECM.
Loss of glycoproteins owing to mutation interferes with normal muscle function. A consequence of most CMD-cause mutations is evaluated susceptibility to cellular injury from normal contraction, and a reduced ability to repair the damage.
It isn’t known why the CMDs cause muscle weakness initially than other sorts of genetic defects. One possibility is that the muscle proteins affected are required initially within the development of an infant’s muscle, while muscle proteins connected to other muscular dystrophies, don’t become important until the muscles begin to urge lots of use as a child grows.
It’s important to notice that simply because the muscle weakness in CMD starts within the initial phase, CMD isn’t automatically more severe than other sorts of dystrophy. the speed and degree of progression of muscle weakness differ with various sorts of CMD and from one child to the following one.
In the mid-1990s, researchers found that a deficiency of a protein called merosin and now more often called laminin 211 was the underlying explanation for a minimum of some cases of CMD. Merosin normally attach muscle cells to a structure that covers them (like the skin on a hot dog) called the basal lamina.
Researchers began to suspect that Ullrich’s disease, now known as Ullrich CMD, it was caused by a lack of collagen 6, a rope-like protein situated in the area where laminin 211 is found. Collagen 6, which helps support the fiber of muscle, probably affects muscle cells via its connection to laminin 211. Laminin 211, connects to muscle cells via either of two other proteins: integrin or dystroglycan.
Dystroglycan connects the outer surface of muscle cells with structures outside them via branches, made of sugar molecules, that protrude from its surface and stick to laminin.
The branch structure helps mutations in so many diverse genes all appear to cause CMD. Each of these proteins contributes in various ways to the process of “sugar-coating” (glycosylating) dystroglycan. Various types of CMD — such as Fukuyama CMD, muscle-eye-brain disorder, and Walker-Warburg syndrome — arise from these glycosylation proteins.
The illustration shows the physical relationships between these proteins.
Many forms of congenital muscular dystrophy stem from the loss of firm connections between muscle fibers and their surroundings (extracellular matrix).
Inheritance:
What are the inheritance patterns in CMD?
Congenital muscular dystrophies are caused by genetic deformities that affect important muscle proteins. The most common type of CMD is inherited in an autosomal recessive pattern.
If a disease is recessive, two copies of the faulty gene (one from each parent) are needed to produce the disease. Each parent would be a bearer of the gene flaw but wouldn’t usually have the disease.
If a disease is dominant, then only one copy of the genetic faulty is needed to cause the disorder. Anyone with the gene flaw will have disorder signs and symptoms and can pass the disorder to children. One or both parents may be bearers, unknowingly harboring the genetic mutation. Many parents have no idea they are bearers of the disorder until they have a child who has the disease.
Signs and Symptoms of Congenital Muscular Dystrophy:
CMD can cause contractures in many joints such as the wrists, ankles, and many more. The term congenital muscular dystrophy (CMD) is the name for a group of muscular dystrophies united by muscle weakness that begins in infancy or the very initial phase in childhood (before age 2). The symptoms of congenital disorders are present at or soon after birth.
Most of the child with CMD show some gradual muscle weakness, although they can have severe, various symptoms and rates of progression.
Firstly, weakness identified as hypotonia, or lack of muscle tone, can make a child seem “floppy” and in the later phase, infants and toddlers may be slow to meet motor milestones such as sitting up or walking, rolling over, or may not meet some milestones at all. Some of the unusual types of CMD are also attended by significant learning disabilities.
Other signs and symptoms include:
- Trouble in swallowing.
- Heart problems, such as heart failure (cardiomyopathy) and arrhythmia
- Stiff or loose joints.
- Curved spine (scoliosis).
- Breathing problems.

Some symptoms which typically appear in early childhood might include:
- Falls frequently
- Difficulty in rising from sitting position and lying position
- Trouble in running and jumping
- Waddling gait
- Walking on the toes
- Calf muscles become enlarge
- Muscle spasm, pain, and stiffness
- Disability in learning
- Growth delayed
Investigations of Congenital Muscular Dystrophy (CMD):
An early, accurate diagnosis is important for children born with congenital muscular dystrophy because a previous diagnosis leads to faster treatment.
Diagnosing your child may include:
Medical history and physical examination, including a family history of any neuromuscular disease.
Electrodiagnostic tests (EMG/NCS): Neuromuscular neurologists examine muscle and nerve function by using a machine that measures electrical signals in individual person’s muscles and nerves.
Electromyography(EMG): For the test, an electrode needle is inserted into the muscle. Electrical activity is measured by relaxing and gently tightening the muscle. Electrical activity changes in the pattern can confirm a muscle disease.
Laboratory tests: These tests may be use to check muscle enzymes. Impaired muscles release enzymes, such as creatine kinase (CK), into the blood. In case some person who hasn’t had high blood levels of CK, traumatic injury, suggests a muscle disease.
Imaging studies: Detected by undergoing ultrasound or magnetic resonance imaging (MRI).
Muscle Biopsy: Muscle and nerve cells are examined by a microscope. A small piece of muscle can be removed by an incision or with a hollow needle. After that analysis of the tissue sample can identify muscular dystrophies from other muscle diseases.
Genetic testing: For known to cause congenital muscular dystrophies, examines individual genes to look for abnormalities. Blood samples can be also examined for mutations in some of the genes that cause muscular dystrophy.
Heart-monitoring tests (electrocardiography and echocardiogram): These tests are used to check heart function.
Lung-monitoring tests: These tests are used to check lung function.
Differential Diagnosis:
Differential diagnosis of patients with weakness in early infancy includes:
Congenital myopathies – the most common ones are centronuclear myopathy, central core, and nemaline road. These may also present metabolic disorders that affects the metabolism of many molecules, carbohydrates, and fats.
Disorders of the myoneural junction – These are very rare in happening but should be part of differential diagnosis of infants presenting with weakness. These include congenital infant botulism and myasthenia gravis.
Neuropathies – These disorders primarily affect the nerve roots in the peripheral nerves and spinal cord. Common neuropathies shown in the initial phase of childhood include spinal muscular atrophy (SMA) and hereditary motor sensory neuropathy (HMSN).
Treatment of Congenital Muscular Dystrophy:
Medical Treatment:
Treatment of these diseases is helpful since the replacement of specific genes and proteins has been tested mostly in animal specimens. The use of these medications and gene therapy in humans has been part of clinical experiments. If respiratory muscles are affected, assisted automatic ventilation is done at home with the help of parents and home nursing.
Intensive physical and occupational therapy is an important part of the care of these patients while they are admitted to the hospital and should be continued at home. These patients require surgical intervention for other morbidities like scoliosis due to placement of feeding gastrostomy, prolonged immobility, or gastrojejunostomy tube to keep up with nutritional requirements.
Nutritional support plays an important role in the long-term treatment of these patients as they are underweight, and macro/micronutrient insufficiencies in them can magnify the underlying muscle weakness.
Many patients can have normal mental abilities and require support in the form of psychologists and psychiatrists to help them deal with the stress of chronic disease.
Physiotherapy Treatment for Congenital Muscular Dystrophy(CMD):
Physiotherapists work with children who have muscular dystrophy to inhibit or reduce joint contractures, maintain or increase cardiorespiratory and strength of muscle, modify activities or the child’s home or school environments to encourage the movement and mobility skills, and increase daily activities, which encourage participation in the community.
Improvement of developmental skills. Your physiotherapist will help your child learn motor skills such as Improvement of developmental skills. Your physical therapist will help your child learn to master motor skills such as crawling, walking, getting up to stand, and jumping.
Physical fitness and activity. Your physiotherapist will help specify the specific exercises, diet, and community involvement that will promote your child’s good health. When needed, mobility aids such as splints and braces, wheelchairs, and home devices may be suggested to help maintain mobility.
Physiotherapy may be provided in the home or at another location, such as a community center, school, or physiotherapy clinic. Physiotherapists work with other health care professionals, including speech/language.
If you expected to have corrective orthopedic surgery for scoliosis or contractures, your physiotherapist can assist in assessing the need for equipment, orthopedic appliances used for support, or bracing that might be needed to foster a quick recovery during postop rehabilitation.
If a child has been diagnosed with muscular dystrophy, treatment may include:
Exercises for Congenital Muscular Dystrophy(CMD):
Stretching exercises:

Wrist flexor stretch:
Position: sitting
Instructions: With your palm up and bending your wrist extend your arm in front of you, showing your hand toward the floor. Gently bend your wrist further with your other hand until you feel a mild to moderate stretch in your forearm. Hold for at least 15 to 30 seconds
Repeat 2 to 4 times.
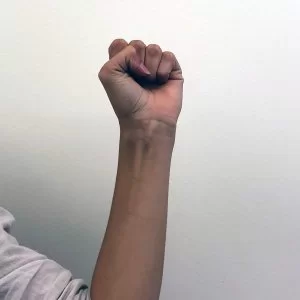
Raised fist stretch:
Position: sitting
Instructions: Keep your thumb outside and make a fit, with your arm up beside your head with your hand open. Slide your fingers toward your wrist until you feel a stretch. This position was held for 3–5 seconds.
Repeat 2 to 4 times.
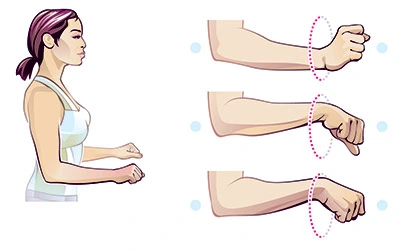
Wrist rotations:
Position: sitting
Instruction: Stretch your one arm around a 90-degree flexion in front of you. The elbow is straight and keeps the palm facing towards the ceiling. Slowly, move your fingers downward until you feel the stretch, and then use the other hand to slowly pull the raised hand downward and inward toward the body and hold that position for 3-5 seconds.
Then move your fingers toward the ceiling until you feel a stretch. Now use another hand to slowly pull the raised hand toward the body and hold that position for 3-5 seconds.
Repeat this 3 times.

Prayer position:
Position: Standing
Instruction: Take a standing position, place your both palm together in a praying position and your elbows touch each other. Try that your plan should be in front of your face. Your arms should be touching each other from your fingers to your elbows, then pressing your palm together, slowly moving your elbows apart. Perform this while slowly lowering your hands at the height of waits, then stop the motion when your hands are in front of your umbilicus or you sense the stretch. Then hold that position for 10-30 seconds.
Repeat 3 times.
Finger stretch:
Position: sitting or standing
Instructions: Extend your arm in front of you in flexion, then make a fist and hold that in front of you. After that try to open and flat your hand and open your fist and stretch your every finger together.
Repeat 10 times.
Fist-opener:
Position: sitting or standing
Instructions: Extend your arm in front of you, then make a fist and hold that in front of you. After than open your fist and stretch each and every finger together until you feel a stretch and until your hand opens and is flat.
Repeat this 10 times.

Sponge-squeeze:
Position: Sitting
Instructions: In this movement, you need a stress ball or sponge. Hold a ball in your hand and squeeze that ball by making a fist. Hold this position for 10 seconds or until you feel a stretch and then relax.
repeat 10 times.

Windshield wiper wrist movement:
Position: Standing
Instructions: Patient with standing position facing toward the wall, then hold a resistance band in both hands (one end is in one hand and another one is on other hand). Put both arms on a wall and one hand is stable on the wall while the other one is moving away from the body. Stretch a wrist as much as you can without moving your elbow. Hold this position for 3-5 seconds and then do the same with the other hand.
Repeat 3 times on each hand.

Thumb pull:
Position: sitting
Instruction: Grasp your left thumb by your right hand and then slowly pull the thumb back, away from your left hand. When you feel the stretch then stop there and hold that position for 25 seconds.
Repeat this on the right thumb.

Alternate finger stretch:
Position: sitting
Instructions: To perform this movement, bring the ring and middle finger together. While separating the index and little fingers from the ring and fingers.
Repeat this stretch 10 times.

Neck stretch:
Position: Supine lying
Instructions: Lie down on a flat surface or plinth and then roll up a towel and place the towel under the neck where it naturally bends. After then gently tip your chin back and hold this position for 5-10 seconds. You feel the stretch in the muscles on the front and sides of your neck. Repeat this 2 times a day to relieve your neck muscles.
Quad stretch:
Position: Prone lying
Instructions: Lie flat on your stomach and fold your arms under your forehead to support your head. Your partner should hold your left leg around the ankle and gently lift it up to move it towards the left buttock. Push against this movement for 5 seconds to build resistance and feel your quadriceps stretch. Relax for5 seconds.
Repeat 3 times. Repeat with the right leg.
Butterfly stretch:
Position: supine lying
Instructions: Lie flat on your back with arms at the side. Press the heel of your feet together and put your knees slightly apart. The partner should hold your knees and gently push them out and down towards the floor. Push back to create resistance against this movement for 5 seconds.
Then relax for 5 sec. Repeat the stretch four more times.
Back stretch:
Position: supine lying
Instruction: Patient is in lie down position and places the towel roll under the shoulder blades, roughly around the middle of the back. You can also place a towel roll under the neck for support. Rest your arms on the floor at a 45-degree angle away from your body, and hold this position for 5 seconds.
Repeat 2 times a day to stretch out the back and chest muscles.

Hamstrings stretching:
Position: Long sitting
Instructions: The patient is in a long sitting position on the flat surface or plinth, with both legs out straight on the floor. Extend your arms and reach forward and try to touch your toe by bending at the waist as far as possible during this try to keep your knees straight. Hold this position for 15 to 30 seconds.
Relax back into the starting position.
Repeat three times.

Hip adductors stretching:
Position: supine lying
Instructions: The patient is lying on your front bend the knee to 90 degrees and then slowly let the footfall away from the body. Try to keep your knees together and hold that position till you are comfortable.
Repeat 3 times.

Hip abductors stretching:
Position: Standing
Instruction: The patient is in a standing position. He/she stands facing a wall with the feet together. Place the hands on the wall or the hips for balance. Raise the left leg out to the side as high as possible, without rotating the hips. 5 seconds hold and then return to the starting position, then repeat on another side
Repeat 10 times.
Calf stretching:
Position: Standing position
Instructions: Ask the patient to stand and face toward the wall from 3 feet away. Take one step toward the wall with your foot. Both palms placed on the wall. Bend your right knee. Lean forward, keep the other leg straight and the heel on the floor. 5 seconds hold and return to the sarting position.
Repeat 10 times.

Retraction:
Position: Sitting
Instruction: Ask the patient to sit on a chair or table, then put the band around a solid object, such as a bedpost at waist level, with your elbows at your sides and bent to 90 degrees, and pull the band back to move your shoulder edges toward each other.
Repeat 8 to 12 times.
Lateral flexion of the neck:
Position: Sitting
Instructions: The patient should sit on a chair or table, then ask the to patient gently bend his neck and try to touch his right ear to his shoulder. When you feel the stretch on the left side of the neck, stop. Hold for 20 seconds and then back to starting position.
Repeat 3-4 times.

Neck forward flexion:
This exercise is used to loosen the tension of the neck and shoulders.
Position: Sitting
Instructions: The patient should sit on a table or chair, then bend your chin toward your chest and gently tilt your head to the left to stretch your right shoulder. You will feel a stretch in the back side of your neck. Hold this position for up to 1 minute.
Repeat on the opposite side. Do each side 3–5 times.
Strengthening exercise:

Straight leg raise (SLR):
Position: Supine lying
Instructions: Patient is lying on his/her, and ask them to keep back and legs straight and together. Keep your legs straight and lift them up to the ceiling until your butt comes off the floor. Lower your legs back down slowly till they’re just above the floor. Hold for 10 seconds and your legs back to the starting position.
Repeat.

Donkey kicks:
Position: Quadriped position
Instructions: Ask the patient to brace his/her core with knees and hips slightly bent, and use the glute to kick their working leg directly back as high as possible, it will go without compromising your hip position. Resist the weight and slowly put down your foot back to the real position. Complete 10-12 reps for 2-4 sets on each leg.
Repeat.

Bodyweight Squat or Mini-Squat:
Position: Standing
Instructions: The patient stand with his/her feet hip-width apart, toes pointing slightly outward or straight outside. Try to put your body weight on heels and your hips backward, bending your knees as if sitting down on a chair. 5-second hold.
Repeat 5 times.
Trunk Exercises:

Trunk rotations:
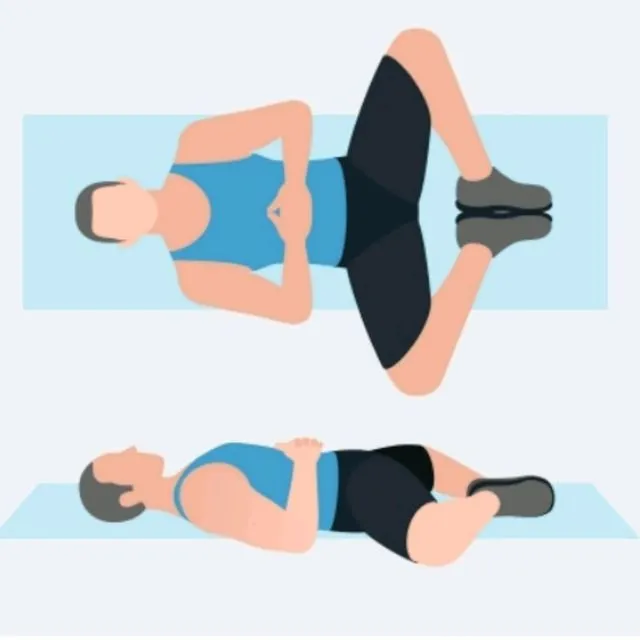
Position: Supine lying
Instructions: The patient is supine on the flat surface or a plinth, bring both knees to bend and keep your feet flat on the surface, then just rotate your knees from one side to another side and try to keep your upper body flat on the ground and then switch to the other. Side you.
Repeat 10 times.

Lateral bending of trunk:
Position: Standing position
Instructions: The patient is in a standing position and then, shoulder width apart, feet are a little wider. Raise your right arm over your head and slowly lean to the left/side. Keep your stomach tight. You feel the hip and stomach muscles pulled during leaning. Repeat with the other side.

Crunches:
Position: Supine lysing
Instructions: The patient is lying on a flat surface or a plinth, then starting with forwarding crunches to maintain posture. For stability, hands behind your head and balance crunch forward so as to squeeze the muscles just below the ribcage. 5 seconds hold and return to starting position.
Repeat.
Breathing Exercise:

Deep breathing:
Position: Standing or sitting.
Instructions: Draw your elbows back slightly to allow your chest to expand, and then take a deep inhalation through your nose. Retain your breath for a count of 5. After then slowly release your breath by exhaling through your nose.

Pursed lip breathing:
This technique is practiced at any time. This is especially useful during some exercises or activities such as lifting, stair climbing, or bending. Practice this breath 4 to 5 times a day.
Position: Sitting on a couch or a chair.
Instructions: The patient is in a relaxed and comfortable position and relaxes the neck and shoulders. Your mouth is closed and then, slowly inhales through your nose and purses your lips as though you were going to whistle. Exhale slowly like blowing air through your pursed lips.
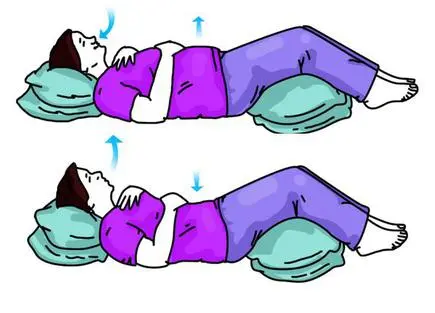
Diaphragmatic breathing:
This type of breathing technique is used for your diaphragm properly. Do these exercises when you’re feeling relaxed and rested. Practice and do diaphragmatic breathing for 5 to 10 minutes 3 to 4 times per day. When you may feel tired, but over time the technique should become easier and should feel more natural.
Position: Semi-flower position.
Instructions: Lie on your back with support and your knees slightly bent and your head on a pillow. For support, you may place a pillow under your knees. One hand is placed on your upper chest and another one is below your rib cage then, allowing you to feel the movement of your diaphragm. Slowly inhale through your nose, feeling your stomach pressing into your hand, and then, exhale using pursed lips as you tighten your stomach muscles.
Repeat.
Complications:
Respiratory: Chronic respiratory failure and muscle weakness leads to pneumonia and atelectasis.
Cardiac: Cardiomyopathy can be a common co-morbidity, and it can have chronic heart failure, which can require medical therapy.
Musculoskeletal: They can have scoliosis due to increased risk of fractures, immobility, and osteopenia. Pressure ulcers and joint contractures may also develop.
Endocrine: Adrenal insufficiency is common in these patients, and they may require steroid supplements in case of stress. Vitamin D and thyroid levels should also be assessed as a part of the comprehensive evaluation.
Neurological: Some of these patients can have seizures, and the burden of psychological disorders like depression and anxiety is high in these patients due to underlying chronic disease.