Miller Fisher Syndrome
Table of Contents
What is Miller Fisher Syndrome?
Miller Fisher Syndrome (MFS), also called Fisher’s syndrome, commonly begins with the rapid development, over days, of 3 problems:
- Weak eye muscles, double or blurred vision, and sometimes drooping eyelids with facial weakness,
- Weak balance and coordination with sloppy or clumsy walking,
- on physical examination, decrease in deep tendon reflexes, such as the knee and ankle jerk.
- Miller Fisher Syndrome(MFS) is named after Dr. C. Miller Fisher who described it in 1956 as a limited different of ascending paralysis, Guillain- Barre syndrome (GBS).
How common is Miller Fisher Syndrome(MFS)?
- Miller Fisher Syndrome(MFS) is a rare disorder.
- Guillain-Barré syndrome affects only 1 in 100,000 people trusted Source.
- Miller Fisher Syndrome(MFS) makes up just 1-5 percent of trusted sources of these cases in Western countries, but more in Taiwan and Japan.
- Because Miller Fisher Syndrome(MFS) is such a rare condition, it can sometimes be challenging to diagnose.
- A person who thinks they have either of these conditions may need to look for a specialist.
Who is at risk?
- Anyone can develop Miller-Fisher syndrome(MFS), but some are more prone than others.
They include:
- Men. The Journal of the American Osteopathic Association notes that men are twice as likely to have Miller-Fisher syndrome(MFS) as women.
- People who are of middle age.
- The mean age of developing Miller-Fisher syndrome(MFS) is 43.6 years.
- People who are Taiwanese or Japanese.
- According to a case, reportTrusted Source published in the Hawai‘i Journal of Medicine & Public Health, 19 percent of GBS cases in Taiwan fall under the Miller-Fisher syndrome(MFS) category.
- That number jumps to twenty-five percent in Japan.
Miller Fisher syndrome(MFS) triad
- Background and objective: Miller-Fisher syndrome (MFS) is considered the most usual variant of Guillain-Barré syndrome (GBS) and is characterized by the clinical triad of ophthalmoplegia, ataxia, and areflexia.
- Respiratory involvement and relapses are uncommon.
What Are the Causes of Miller Fisher Syndrome?
- Both Miller-Fisher syndrome(MFS) and Guillain-Barré syndrome(GBS) develop in response to an illness.
- The illness triggers antibodies to attack your nerves.
- Experts are not sure why this occurs.
- Miller Fisher syndrome commonly develops a few days or up to 4 weeks after an illness, especially a diarrheal disease or respiratory infection.
- Campylobacter jejuni is a usual species of bacteria that triggers Miller Fisher syndrome and Guillain-Barré syndrome.
- These bacteria may source diarrhea and abdominal pain.
Viruses that trigger both diseases involve:
- Zika
- Human immunodeficiency virus (HIV)
- Epstein-Barr (mononucleosis)
What Are the Symptoms of Miller Fisher Syndrome?
- People usually seek medical assistance because their vision decreases rapidly over days.
- They may also have difficulty walking.
The 3 main symptoms of Miller Fisher syndrome are:
- Weakness of your eye muscles, which CONDUCTs to double vision and difficulty controlling eye movements (ophthalmoplegia),
- Problems with limb coordination (ataxia),
- Loss of reflexes in your tendons (areflexia).
Certain people may also have:
- dilated or enlarged pupils
- weakness in their facial muscles
- a decreased gag reflex.
- If you have these symptoms and develop weakness in your breathing muscles and limbs, you may have GBS-MFS overlap syndrome.
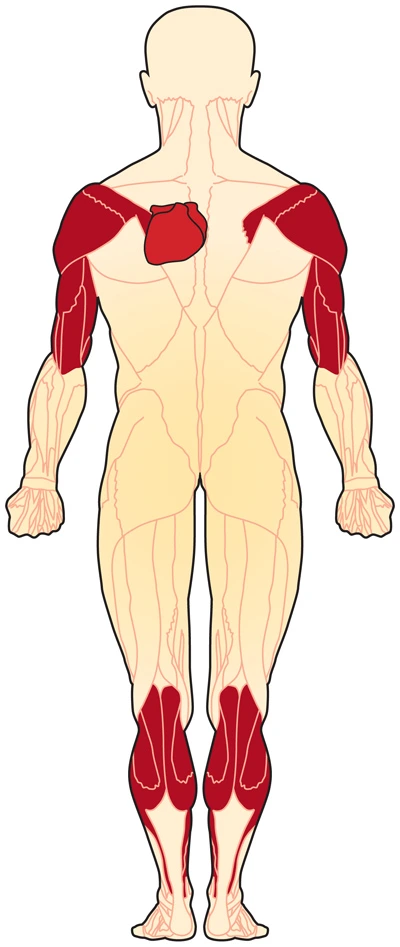
- The main symptom of Guillain-Barré syndrome is the weakness that begins in your legs and spreads to your arms and body.
- In certain people, this weakness spreads to the face, throat, and breathing muscles.
How Is Miller Fisher Syndrome Diagnosed?
It can be hard to diagnose this syndrome because it is similar to several other neurological diseases like:
- Basal meningitis
- Botulism
- Diphtheria
- Brainstem stroke
- Brainstem encephalitis
- Myasthenia gravis.
- There is no specific diagnostic test for Miller-Fisher syndrome.
- Your doctor will do the physical exam and take a medical history.
- They may do a spinal tap (lumbar puncture).
- Many people with Miller Fisher syndrome(MFS) have a high protein count in their cerebrospinal fluid.
- You may need to do a blood test to check for anti-GQ1b antibodies.
- This antibody is found in about 95% of people with Miller Fisher syndrome.
- Your doctor may carry out a nerve conduction study and electromyography (EMG).
- These tests use fewer electric shocks to check the activity of your muscles and sensory nerves.
- If you have Miller Fisher syndrome(MFS), the tests may show abnormalities of your sensory nerves.
- Magnetic resonance imaging (MRI) of your brain may be done to rule out brainstem encephalitis and Guillain-Barré syndrome(GBS).
- In Miller Fisher syndrome(MFS), an MRI is usually normal, but there may be abnormalities for the other diseases.
Miller Fisher syndrome(MFS) antibody
- Miller Fisher syndrome (MFS) is characterized by a clinical triad of ophthalmoplegia, ataxia, and areflexia, and is considered to be a variant of Guillain-Barré syndrome(GBS).
- The presence of the IgG anti‐GQ1b antibody in serum is an excellent diagnostic marker for Miller Fisher syndrome(MFS).
What are the treatment options?
- There is no cure for Miller Fisher Syndrome(MFS).
- The aim of treatment is to fewer the severity of symptoms and speed recovery.
- The 2 main forms of treatment are immunoglobulin therapy and plasmapheresis.
- These are the same treatments used for Guillain-Barré syndrome(GBS).
Immunoglobulin therapy
- This treatment includes delivering (through an injection into a vein) high doses of proteins the immune system uses to attack infections.
- Researchers are not exactly sure why this helps to lessen the immune system’s attack on the nervous system, but it does seem to speed recovery.
Plasmapheresis
- This is a procedure in which red and white blood cells(WBCs) are removed from the plasma (or liquid) portion of the blood.
- These cells are later reintroduced into the body, without the plasma.
- Both these procedures seem to be equally effective trusted Sources in improving the disorder.
- Though, intravenous immunoglobulin therapy is easier to administer.
- It may be the 1st therapy tried.
- Physical therapy to assist the affected muscles to regain strength may also be recommended.
- There is no prevention for Miller Fisher syndrome.
- But treatment can assist your symptoms to improve faster.
- People with Miller Fisher syndrome(MFS) are usually treated in the hospital.
- This will allow doctors to rule out Guillain-Barré syndrome(GBS), which can be fatal.
- Because Miller Fisher syndrome(MFS) is related to Guillain-Barré syndrome(GBS), treatments for Guillain-Barré syndrome(GBS) are usually given.
- These treatments may involve plasma exchange (plasmapheresis) and intravenous immunoglobulin (IVIg).
- Intravenous immunoglobulin is commonly the first treatment given because it is more widely available and convenient than plasmapheresis.
- Intravenous immunoglobulin is usually given for five days.
- These infusions contain antibodies found in the blood.
- They come from plasma that is pooled from thousands of healthy people and then purified.
- In plasmapheresis, a thin plastic tube attaches your vein to a machine.
- Your blood travels between the tube and into the machine.
- The machine withdraws the plasma in your blood and replaces it with substitute plasma.
- This substitutes plasma and you’re allowed blood cells are then returned to your body.
- For Miller Fisher syndrome(MFS), you will need about 5 rounds of plasmapheresis over about 2 weeks.
- If your muscles are severely weakened by the disease, you may require physiotherapy for 1 to 2 weeks.
- The goal of rehabilitation is to strengthen your muscles and get function next to as close as normal as possible.
- On average, recovery from this disease will take about eight to 12 weeks.
- Most people fully recover within six months.
- Lesser than 3% have a recurrence.
Are there complications?
- Miller Fisher Syndrome (MFS) symptoms tend to progress for several weeks, plateau, and then start to improve.
- Typically, Miller Fisher Syndrome (MFS) symptoms begin to improve within four weeks.
- Most people recover within six months of trusted Source, although some residual weakness can linger.
- Because the muscle weakness of Miller Fisher Syndrome (MFS) can also affect the heart and lungs, resulting in cardiac and breathing problems, hospitalization and careful medical supervision are necessary during the course of the illness.
What is the outlook?
- Miller Fisher Syndrome (MFS) is an exceedingly rare condition that is, fortunately, short-lived.
- While there can be serious complications, like breathing issues, most people are successfully treated and make full, or nearly full, recoveries.
- Relapses are rare, occurring in less than 3 percent of trusted sources of cases.
- Learn about two women diagnosed with Guillain-Barré syndrome(GBS) who went on to have normal lives.
- Talk to your doctor about the 1st sign of symptoms.
- Early treatment can assist in speedy recovery.
Miller Fisher syndrome (MFS) in COVID-19
- Miller Fisher syndrome (MFS), also known as the Miller Fisher different of Guillain-Barré syndrome(GBS), is an acute peripheral neuropathy that can develop after exposure to various viral, bacterial, and fungal pathogens.
- It is sometime immune-mediated and associated with anti-GQ1b antibodies, characterized by a triad of ophthalmoplegia, gait ataxia, and areflexia.
- Ophthalmoplegia is due to the inclusion of cranial nerves III, IV, or VI.
- Ataxia is the concept to be due to cerebellar involvement, and areflexia is due to lower motor neuron involvement.
- Miller Fisher syndrome(MFS) has lately been described in the clinical setting of the novel coronavirus disease 2019 (COVID-19) without accompanying imaging findings.
- While patients with COVID-19 commonly present with fever, shortness of breath, and cough, neurologic manifestations, including headache, ataxia, cognitive impairment, anosmia, and stroke, have been reported.
- One retrospective review of 214 patients found neurologic symptoms in 36.4% of patients, with involvement of the CNS (24.8%) greater than the peripheral nervous system (8.9%).4 In this case, we report the first presumptive case of COVID-19–associated Miller Fisher syndrome(MFS) with imaging.
- A 36-year-old man with a distant history of left eye strabismus (asymptomatic for 30 years) was brought to the emergency department by ambulance, presenting with left eye drooping, blurry vision, and reduced sensation and paresthesia in both legs for two days.
- He was in his usual state of health until four days before presentation when he developed viral symptoms in a COVID-19 endemic region, reporting subjective fevers, chills, and myalgia.
- Physical examination was notable for a partial left third nerve palsy and decreased sensation under the knees to all modalities.
- MR imaging of the brain, involving high-resolution imaging of the orbits and retro-orbital region, with and without gadolinium, was notable for striking enlargement, prominent enhancement with gadolinium, and T2 hyperintense signal of the left cranial nerve (CN) III (Figure).
- No other cranial nerves demonstrated abnormal signals or enhancement of characteristics.
- MR imaging of the brain had the usual findings.
- No cerebellar lesions were seen to explain the patient’s ataxia.
- There were no findings of meningitis, encephalitis, demyelination, or infarction.
- MR imaging(MRI) of the spine, which may have provided that imaging correlates for the patient’s areflexia, was not performed.
- The diagnosis of COVID-19 was confirmed by qualitative detection of Severe Acute Respiratory Syndrome coronavirus.
- RNA in a nasopharyngeal swab specimen by real-time reverse transcription polymerase chain reaction amplification & detection using TaqMan fluorescent oligonucleotide probes (Altona Diagnostics) on the Rotor-Gene Q instrument.
- Serologic ganglioside antibody testing was performed by the semi-quantitative enzyme-linked immunosorbent assay (ARUP Laboratories) and showed Asialo GM1 antibody in the equivocal range, while testing for other antibodies, including anti-GQ1b, was negative.
- Nonetheless, the patient’s hospital course was characterized by progressive ophthalmoparesis (including initial left CN III and eventual bilateral CN VI palsies), ataxia, and hyporeflexia, and the clinical picture was thought to be consistent with Miller Fisher syndrome(MFS) from COVID-19 infection.
- The patient was treated with intravenous immunoglobulin, with the subsequent improvement of neurologic symptoms.
- The patient also received hydroxychloroquine to treat the underlying COVID19 infection.
- No repeat MR imaging was performed, and the patient was discharged after four days of hospitalization.
- Miller Fisher syndrome(MFS) accounts for 1%–5% of cases of Guillain-Barré syndrome in Western countries, affects men twice as often as women, and is preceded by an upper respiratory illness in most patients.
- Miller Fisher syndrome(MFS) presents commonly with diplopia (78%), ataxia (48%), or both (34%).6 Our patient presented with symptoms of COVID-19 as well as diplopia, which was found to be due to a CN III palsy noted on the patient’s clinical examination.
- MR imaging(MRI) demonstrated corresponding enlargement, T2 hyperintensity, and enhancement of the affected CN III from the cavernous sinus through the orbit.
- This is the first presumptive case report of Miller Fisher syndrome(MFS) associated with COVID-19 infection with imaging findings.
- Although testing was negative for anti-GQ1b, the clinical picture was consistent with Miller Fisher syndrome(MFS), and the patient improved with treatment.
- Negative ganglioside antibody testing is a limitation of this report; however, a review of 123 patients with Miller Fisher syndrome(MFS) found that 15% were negative for anti-GQ1b.
- The GQ1b ganglioside is a cell surface component that is concentrated in the paranodal regions, cranial nerves(CN) III, IV, and VI.
- Anti-GQ1b antibodies have been shown to bind to fractions of Campylobacter jejuni and Haemophilus influenza and are thought to cause the symptoms of Miller Fisher syndrome(MFS) through molecular mimicry.
- When antibody testing is negative in patients with Miller Fisher syndrome(MFS), symptoms may be due to viral neurotropism rather than immune-mediated injury.
- The functional receptor for COVID-19 is angiotensin-converting enzyme two which is present in neural tissue.
- Access to the CNS may be either hematogenous or via retrograde neural propagation through bipolar cells.
- Retrograde propagation along the olfactory pathway may account for the occurrence of anosmia in certain patients with COVID-19.
- It has been proposed that retrograde propagation could lead to brain stem involvement and contribute to respiratory symptoms by affecting the nuclei that regulate respiratory rhythms such as chemoreceptors that detect changes in oxygen(O2) and carbon dioxide CO2.
- Understanding of COVID-19 pathophysiology in the CNS and peripheral nervous system and its contribution to morbidity and mortality is unmoving in its infancy.
- Whether Miller Fisher syndrome(MFS) is the result of immune-mediated injury or viral neurotropism, this potential complication should be recognized by clinicians and radiologists so that appropriate treatment can be offered to these symptomatic patients.
FAQs
What are the symptoms of Miller Fisher syndrome?
Features involve weakness of the eye muscles causing difficulty moving the eyes; impaired limb coordination and unsteadiness; and absent tendon reflexes.
Other symptoms may involve facial, swallowing, and limb weakness, as well as respiratory failure.
Miller Fisher syndrome(MFS) can affect both children and adults.What is the cause of Miller Fisher syndrome?
Miller Fisher Syndrome (MFS) is one of the infrequent forms of a spectrum of Guillain-Barré syndrome (GBS).
It is a neurological condition that is rooted in mild to severe muscle weakness.
It is rooted in an immune system reaction against some proteins in our nerves important for movement, sensation, and function.Is Miller Fisher syndrome genetic?
Additional physical abnormalities can happen in some cases.
Intelligence is not affected.
Miller syndrome is inherited in an autosomal recessive pattern rooted in mutations in the DHODH gene.
Miller syndrome was 1st described in the medical field between 1969 and 1979 through several independent reports.Does Miller Fisher syndrome go away?
The prognosis for most individuals with Miller Fisher syndrome(MFS) is good.
In most cases, recovery begins within 2 to 4 weeks of the onset of symptoms and may be almost complete within six months.
Certain individuals are left with residual deficits.
Relapses may happen rarely (in less than 3 percent of cases).What can mimic Guillain-Barré syndrome?
Other neurological conditions, which usually mimic this Guillain-Barré syndrome (GBS) variant include brainstem stroke, myasthenia gravis, botulism, infective or inflammatory rhombencephalitis, and bacterial, carcinomatous, or lymphomatous meningitis.