Crohn’s Disease
- Crohn’s disease (A type of inflammatory bowel disease (IBD)) causes your digestive tract to suit swollen and irritated. If you have Crohn’s, you might experience symptoms such as abdominal pain, diarrhea, weight loss, and rectal bleeding.
- This is a life-long condition that cannot be prevented. However, treatments typically assist manage your symptoms and allow you to live an active life.
- Crohn’s disease is a type of inflammatory bowel disease (IBD). As many as 780,000 Americans (US) have the condition, recordmaintained by the Crohn’s & Colitis Foundation of America (CCFA).
- More research about Crohn’s disease is required. Researchers are not sure how it starts, who is most likely to develop it, or how to best manage it. Despite major treatment advances in the last three decades, no prevention is available yet.
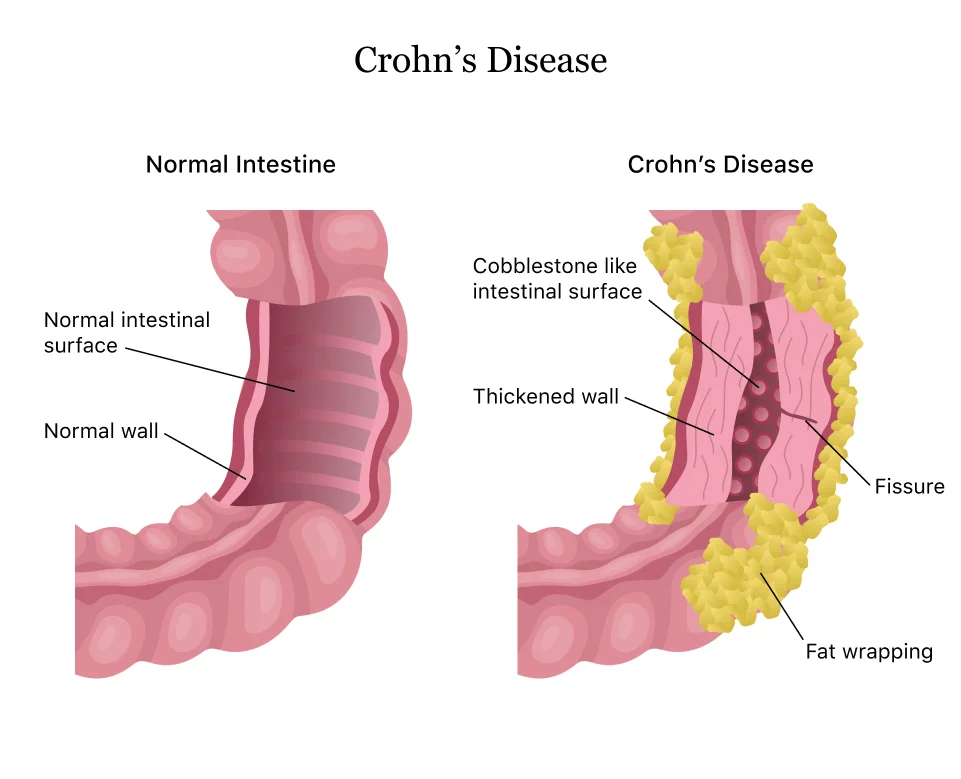
- Crohn’s disease most typically occurs in the small intestine and the colon. It can harm the area of your gastrointestinal (GI) tract, from the mouth to the anus. It can involve certain parts of the gastrointestinal (GI) tract and skip other parts.
- The range of seriousness for Crohn’s is mild (light) to debilitating. Symptoms vary and can change a great time. In serious cases, the disease can conduct to life-threatening flares and complications.
- Here is everything you require to know about Crohn’s disease.
Table of Contents
What is Crohn’s disease (CD)?
- Crohn’s disease, known as regional enteritis or ileitis, is a lifelong form of inflammatory bowel disease (IBD). The condition inflames & irritates the digestive tract — specifically the little and big intestines. Crohn’s disease can cause diarrhea & stomach cramps. It is common to experience periodic disease flare-ups.
- Crohn’s disease obtains its name from American gastroenterologist Dr. Burrill Crohn (1884-1983). He was one of the 1st physicians to describe the illness in 1932. Ulcerative colitis is another commonly diagnosed inflammatory bowel disease (IBD).
How common is Crohn’s disease?
- An estimated 1/2 a million Americans have Crohn’s disease. This can include men, women, & children.
Who might get Crohn’s disease (CD)?
- Crohn’s disease typically appears in younger people – sometimes in their late teens, 20s, or early 30s. However, this condition can occur at any age. It is equally usual in men and women. Crohn’s disease can also be looked at in young children.
- If you are a cigarette smoker, your risk of Crohn’s disease might be greater than non-smokers.
What are the types of Crohn’s disease (CD)?
Crohn’s disease can harm various sections of the digestive tract. Types of Crohn’s disease involve:
- Ileocolitis: Inflammation occurs in the small intestine and area of the large intestine, or colon. Ileocolitis is the most usual type of Crohn’s disease.
- Ileitis: Swelling and inflammation develop in the little intestine (ileum).
- Gastroduodenal: Inflammation and irritation harm the stomach and the top of the small intestine (the duodenum).
- Jejunoileitis: Patchy parts of inflammation develop in the upper half of the small intestine (called the jejunum).
What are the symptoms of Crohn’s disease (CD)?
- People with Crohn’s disease can experience periods of serious symptoms (flare-ups) followed by periods of no or very mild symptoms (remission). Remission can last weeks or even years. There is no way to predict when flare-ups will occur.
- The symptoms of Crohn’s disease often develop gradually. Certain symptoms may become worse over time. Although it is possible, it is rare for symptoms to develop suddenly and dramatically.
If you have Crohn’s disease, symptoms you might have can involve:
- Abdominal pain
- Chronic diarrhea
- A feeling of fullness
- Fever
- diarrhea
- A loss of your appetite
- Weight loss
- fatigue
- Abnormal skin tags (commonly on your buttocks)
- Anal fissures
- Anal fistulas
- Rectal bleeding.
- It is often possible to mistake these symptoms for those of another condition, like food poisoning, an upset stomach, or an allergy. You should look to your doctor if any of these symptoms persist.
- The symptoms may become more serious as the disease progresses.
- Early detection and diagnosis can assist you to avoid severe complications and allow you to start treatment early.
More troublesome symptoms may involve:
- a perianal fistula, which causes pain and drainage close to your anus
- ulcers that may happen anyplace from the mouth to the anus
- inflammation of the joints and skin
- shortness of breathing or reduced ability to exercise due to anemia.
What causes Crohn’s disease (CD)?
There is no known cause of Crohn’s disease. Certain factors may increase your risk of developing the condition, involving:
- Autoimmune disease: Bacteria in the digestive tract may cause the body’s immune system to harm your healthy cells.
- Genes: Inflammatory bowel disease (IBD) sometimes runs in families. If you have a parent, sibling, or another family member with Crohn’s, you may be at an improved risk of also having it. There are several personal mutations (changes) to your genes that can predispose people to develop Crohn’s disease.
- Smoking: Cigarette smoking could as much as double your risk of Crohn’s disease.
Crohn’s disease and its treatments can also harm the immune system, making these types of infections worse.
Yeast infections are usual in Crohn’s and can affect both the lungs and the intestinal tract. It is important that these infections are diagnosed and properly treated with antifungal medications to prevent further complications.
Is Crohn’s an autoimmune condition?
- An autoimmune condition causes your immune system to mistakenly harm your body, sometimes causing inflammation. Though the immune system could be a potential contributor to inflammation in Crohn’s, it has not been classified as an autoimmune condition as the causes are still not fully understood.
How is Crohn’s disease (CD) diagnosed?
- Most people with Crohn’s first see a healthcare provider (doctor) because of ongoing diarrhea, belly cramping, or unexplained weight loss. If you have a child who has been experiencing the symptoms of Crohn’s disease, hold out to your pediatrician.
- No single test result is enough for your provider (doctor) to diagnose Crohn’s disease. They will start by eliminating other possible causes of your symptoms.
To find the cause of your symptoms, your healthcare provider (doctor) may order one or more of these tests:
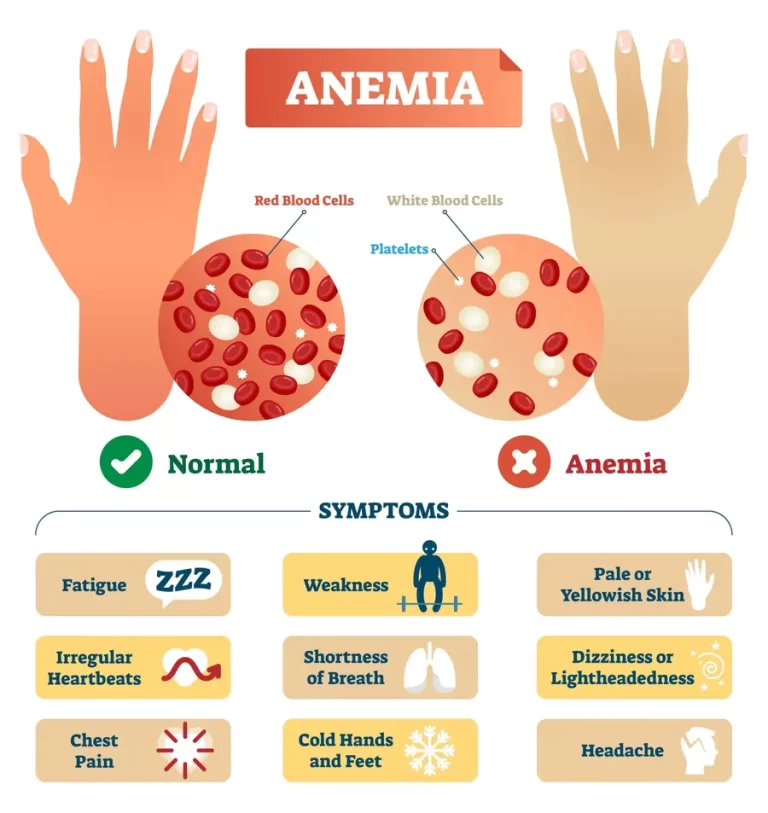
- Blood test: A blood test checks for high numbers of white blood cells (WBCs) that may indicate inflammation or infection. The test also checks for low red blood cell (RBC) count or anemia. Approximately one in 3 people with Crohn’s disease have anemia.
- Stool test: This test seems at a sample of your stool to check for bacteria or parasites. It can rule out infections that cause chronic diarrhea.
- Colonoscopy: During a colonoscopy, your provider (doctor) uses an endoscope (thin tube with an attached light and camera) to examine the inside of your colon. Your doctor may give a tissue sample (biopsy) from the colon to test for signs of inflammation.
- Computed tomography (CT) scan: A CT scan makes images of the digestive tract. It tells your healthcare provider (doctor) how severe the intestinal inflammation is.
- Upper gastrointestinal (GI) endoscopy: Your doctor threads a long, thin tube known as an endoscope through your mouth and into your throat. An attached camera allows your provider (doctor) to see inside. During an upper endoscopy, your doctor may also take tissue samples.
- Upper gastrointestinal (GI) exam: X-ray images used during an upper gastrointestinal (GI) exam allow your doctor to watch as a swallowed barium liquid moves through your digestive tract.
Your doctor may go on to request these tests so many more times to look for harmed tissue and determine how the disease is progressing.
The Healthline FindCare tool can provide options on your part if you need help finding a primary care doctor or a gastroenterologist.
How is Crohn’s disease (CD) managed or treated?
- Treatment for Crohn’s disease (CD) differs depending on what’s causing your symptoms and how severe they are for you. In children, the goal of treatment is to induce remission (the time between symptom flare-ups), keep remission, and manage any complications of Crohn’s disease over time.
- A cure for Crohn’s disease is not available yet, but the disease can be managed. Different treatment options exist that can lessen the severity and frequency of your symptoms.
Your healthcare provider (doctor) may recommend one or more of these treatments for Crohn’s disease:
- Antibiotics: Antibiotics can cure or treat infections. Severe infections can conduct to abscesses (pockets of pus). Or they can cause fistulas (openings or tunnels that connect two organs that do not normally connect).
- Antidiarrheal medication: Prescription medications like loperamide (Imodium A-D) can stop serious diarrhea.
- Biologics: These medications involve monoclonal antibodies to suppress the immune response.
- Bowel rest: To give your intestines a chance to heal, your provider (doctor) may recommend going without food or drink for several days or longer. To get the nutrition you require, you may receive intravenous (parenteral) nutrition. At most drink a prescribed liquid or have a feeding tube during this time.
- Corticosteroids: Cortisone, prednisone, and another corticosteroid ease inflammation brought on by the autoimmune disease.
- Immunomodulators: These drugs quite an inflammation by suppressing an overactive immune system. They involve azathioprine and cyclosporine.
- Surgery: Surgery won’t prevent Crohn’s disease, but it can treat complications. You may require surgery to correct intestinal perforations (holes), blockages, or bleeding.
Medications
- So many types of medications are available to treat Crohn’s. Antidiarrheal and anti-inflammatory drugs are typically used. More advanced options involve biologics, which use the body’s immune system to treat the disease.
- The medications, or combination of medications, you require to depend on your symptoms, your disease history, the seriousness of your condition, and how you respond to treatment.
Anti-inflammatory drugs
- The two important types of anti-inflammatory drugs doctors use to treat Crohn’s are oral 5-aminosalicylates and corticosteroids. Anti-inflammatory drugs are sometimes the first drugs you take for Crohn’s disease treatment.
- You commonly take these drugs when you have mild symptoms with infrequent disease flares. Corticosteroids are used for more serious symptoms yet should only be taken for a short time.
Immunomodulators
- An overactive immune system causes the inflammation that conducts to the symptoms of Crohn’s disease. Drugs that harm the immune system, known as immunomodulators, may reduce the inflammatory response and limit your immune system’s reaction.
Antibiotics
- Certain doctors believe antibiotics may help reduce some of the symptoms of Crohn’s and some of the possible triggers for it.
- For example, antibiotics can decrease drainage and heal fistulas, which are abnormal connections between tissues that Crohn’s can cause.
Biologic therapies
- If you have serious Crohn’s, your doctor may try one of a number of biological therapies to treat the inflammation and complications that can happen from the disease. Biologic drugs can block important proteins that may trigger inflammation.
Surgery
- If less invasive treatments and lifestyle changes do not improve your symptoms, surgery may be necessary. Ultimately, about 75 percent of people with Crohn’s disease will require surgery at a certain point in their lives, according to the Crohn’s & Colitis Foundation of America (CCFA).
- Some types of surgery for Crohn’s involve removing damaged portions of your digestive tract and reconnecting the healthy sections. Other procedures repair harmed tissue, manage scar tissue, or treat deep infections.
Diet
- Food does not cause Crohn’s disease, but it can trigger flares.
- Later a Crohn’s diagnosis, your doctor will likely suggest making an appointment with a registered dietitian (RD). A registered dietitian (RD) will help you understand how food may harm your symptoms and how your diet may help you.
- In the beginning, they may ask you to retain a food diary. This food diary will detail what you eat and how it made you perceive it.
- Using this information, the registered dietitian (RD) will help you create an eating plan. These dietary changes should assist you to absorb more nutrients from the food you eat while also limiting any negative side effects food may be causing.
Physical Therapy Management
Individuals may need physiotherapy to treat the following.
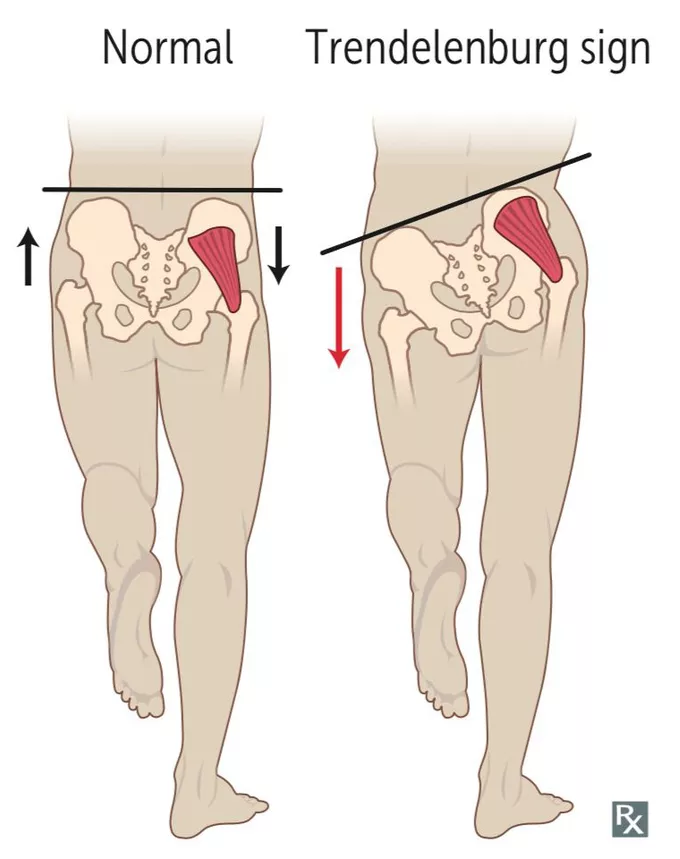
- Crohn’s disease (CD) is associated with arthritis, notably arthritis of the lumbar spine and sacroiliac joints. Though arthritis usually harms older people, Crohn’s-related arthritis is common in young people with the disease. When a patient presents to physical therapy with low back, sacroiliac, or hip pain, it is vital for the therapist to screen for potential organic sources of the pain and for a history of inflammatory bowel disease. See links for re-treatment.
- Crohn’s disease (CD) prevents the correct absorption of nutrients through the intestines into the body. Vitamin D and calcium are key nutrients for bone health, and deficiency can conduct to osteoporosis. Osteoporosis often leads to insufficiency fractures eg in the vertebrae. Vertebral fractures can cause converts in spinal curvatures such as scoliosis, and kyphosis of the spine, leaving other vertebrae more susceptible to fracture. Pain may outcome from the fracture itself, inflammation, and/or biomechanical changes. Educated clients regarding osteoporosis.
- Hydration is very important in patients with Crohn’s disease so the therapist should be aware of signs of dehydration when exercising, for example, headache, dry lips, and disorientation.
- Exercise prescriptions have the ability to boost the immune system, reduce depression, and increase the body image of the patient. In addition to providing this exercise program, therapists can better make coping mechanisms as well as techniques to manage the unexpectedness of Crohn’s Disease.
How does Crohn’s disease (CD) affect pregnancy?
- Women with Crohn’s disease can, and commonly do, have normal pregnancies. Your healthcare provider (doctor) may recommend trying to conceive while the disease is in remission. Flare-ups during pregnancy may increase the risk of:
- Miscarriage (loss of pregnancy previous the baby fully develops).
- Premature labor (childbirth previous to the 37th week of pregnancy).
- Low birth weight (newborn weight of decrease than 5 pounds, 8 ounces).
Crohn’s disease (CD) in children
- Most people with Crohn’s disease receive a diagnosis in their 20s and 30s, but Inflammatory bowel disease (IBD) can develop in children, too. Approximately 1 in 4 people trusted Source with Inflammatory bowel disease (IBD) show symptoms before age 20, according to a 2016 review.
- Crohn’s disease which only includes the colon is common in children and adolescents. That means distinguishing between Crohn’s and UC is difficult until the child starts showing other symptoms.
- Proper treatment for Crohn’s disease in children is main because untreated Crohn’s can conduct to growth delays and weakened bones. It may cause significant emotional distress at this stage in life. Treatments involve:
- antibiotics,
- aminosalicylates,
- biologics,
- immunomodulators,
- steroids,
- nutrition plans.
Crohn’s medications can have certain significant side effects on children. It is vital you work closely with your child’s doctor to find the right options.
What are the variations of Crohn’s disease (CD)?
There are six different of Crohn’s disease, all based on location in the digestive system. They are:
- Gastroduodenal Crohn’s disease. This uncommon condition mainly harms your stomach and the duodenum, which is the 1st part of your small intestine.
- Jejunoileitis. This type occurs in the second portion of your intestine, known as the jejunum. Like gastroduodenal Crohn’s, this variation is less usual.
- Ileitis. Ileitis includes inflammation in the last part of the small intestine, or ileum.
- Ileocolitis. This harms the ileum and the colon and is the most common variation of Crohn’s.
- Crohn’s colitis. This harms the colon only. Both ulcerative colitis and Crohn’s colitis impact the colon only, yet Crohn’s colitis can affect deeper layers of the intestinal lining.
- Perianal disease. This often includes fistulas, abnormal connections between tissues, deep tissue infections, as well as sores and ulcers on the outer skin around the anus.
Crohn’s disease and ulcerative colitis
- Crohn’s disease and ulcerative colitis (UC) are 2 types of IBD. They have many similar characteristics. You may even mistake them for 1 another.
They have the following characteristicsTrusted Source in usual:
- The 1st signs and symptoms of both Crohn’s disease and ulcerative colitis (UC) are very similar. These can involve diarrhea, abdominal pain and cramping, rectal bleeding, weight loss, and fatigue.
- Both ulcerative colitis (UC) and Crohn’s disease occur more commonly in people ages 15 to 35 and people with a family history of either type of IBD.
- In general, IBD tends to harm all sexes equally, but this can vary depending on age.
- Despite decades of research, scientists still do not know what causes either disease. In both cases, an overactive immune system is a likely culprit, yet other factors likely play a role.
Here’s how they vary:
- Ulcerative colitis (UC) only affects the colon. Crohn’s disease can harm any part of your GI tract, from the mouth to the anus.
- Ulcerative colitis (UC) only affects the outermost layer of tissue lining your colon called the mucosa. Crohn’s disease can harm all the layers of your intestinal tissue from superficial to deep.
- Ulcerative colitis (UC) is just one type of colon inflammation. So many other types of colitis exist. Not all forms of colitis cause a similar type of intestinal inflammation and damage as ulcerative colitis (UC).
What are the complications of Crohn’s disease (CD)?
Crohn’s disease can conduct to serious complications, including:
- Abscesses: Injured pus-filled pockets form in the digestive tract or abdomen.
- Anal fissures: Little tears in the anus (anal fissures) can cause pain, itching, and bleeding.
- Bowel obstructions: Scar tissue from inflammation, fistulas or a narrowed intestine can obstruct the bowel partially or completely. Waste matter and gases build up. A blockage in the small bowel or large bowel needs surgery.
- Colon cancer: Crohn’s disease (CD) in the large intestine improves the risk of colon cancer.
- Fistulas: Inflammatory bowel disease (IBD) can cause abnormal tunnel-like openings, called fistulas, to form in the intestinal walls. These fistulas often become infected.
- Malnutrition: Chronic diarrhea can create it hard for your body to absorb nutrients. One usual problem in people with Crohn’s disease is a lack of iron. Too little iron can conduct to anemia (low red blood cell count) when your organs can not get enough oxygen.
- Ulcers: Open sores known as ulcers can form in your mouth, stomach, or rectum.
How can I prevent Crohn’s disease (CD)?
There is no way to prevent Crohn’s disease. These healthy lifestyle changes can ease symptoms and reduce flare-ups:
- Stop smoking.
- Eat a healthy, low-fat diet.
- Exercise regularly.
- Manage stress.
What is the outlook for people with Crohn’s disease (CD)?
- Most people with Crohn’s disease like healthy, active lives. While there is no cure for Crohn’s disease, treatments and lifestyle changes can retain the disease in remission and prevent complications.
- Lifestyle changes can involve changes to your diet. People with Crohn’s disease (CD) often require to adapt their diets so that they get enough calories each day. Lactose intolerance can be a problem for those with Crohn’s disease. You may require to avoid certain dairy products if you find that you are having issues with this dietary intolerance. You should keep away from smoking if you have Crohn’s disease. Smoking can only create your condition worse.
- Your healthcare provider (doctor) might recommend you receive preventative colonoscopies after you are diagnosed with Crohn’s disease. Talk to your provider about how sometimes you should have colonoscopies and what your risks are for other medical conditions.
When should I call the doctor?
You should call your healthcare provider (doctor) if you experience:
- Blood in stool.
- Constipation.
- Extreme weight loss.
- Fever.
- Inability to pass gas.
- Nausea and vomiting.
- Severe abdominal pain.
- Signs of a flare-up.
- Uncontrollable diarrhea.
- Weakness or fatigue may be signs of anemia.
What questions should I ask my doctor?
If you have Crohn’s disease, you may provide to ask your healthcare provider (doctor):
- Why did I get Crohn’s disease?
- What form of Crohn’s disease do I have?
- What’s the best treatment for this disease type?
- How can I prevent flare-ups?
- If I have a genetic form, what steps can my family members take to reduce their risk of Crohn’s disease?
- Should I make any dietary changes?
- What medications should I avoid?
- Should I take supplements?
- Should I get tested for anemia?
- Do I need to cut out alcohol?
- Should I look out for signs of complications?
NOTE
- Crohn’s disease (CD) flare-ups are unpredictable and can drain your daily life. Ask to your healthcare provider (doctor) about the steps you can take to retain the disease in check. With the right treatment and lifestyle changes, you can manage symptoms, keep away complications and live an active life.
FAQs
The cause of Crohn’s disease (CD) is unknown. Researchers think that an autoimmune reaction may be one cause. An autoimmune reaction happens when your immune system attacks healthy cells in your body. Genetics may also play a role since Crohn’s disease can run in families.
Crohn’s disease (CD) can lead to serious complications, including Abscesses: Infected pus-filled pockets form in the digestive tract or abdomen. Anal fissures: Small tears in the anus (anal fissures) can cause pain, itching, and bleeding.
Some of the earliest signs include:
Appetite loss.
Abdominal pain.
Fever.
Exhaustion.
Joint pain.
Nausea.
Pain and redness in eyes.
Red bumps on the skin.
One cause of Crohn’s disease (CD) may be an autoimmune reaction—when your immune system attacks healthy cells in your body. Experts think bacteria in your digestive tract can mistakenly trigger your immune system. This immune system response causes inflammation, leading to symptoms of Crohn’s disease.
Most people with Crohn’s disease (CD) need to take steroids (such as prednisolone) from time to time. Steroid medicines: can relieve symptoms by reducing inflammation in your digestive system – they usually start to work in a few days or weeks. are usually taken as tablets once a day – sometimes they’re given as injections.
Conditions That Can Look Like Crohn’s Disease (CD)
Ulcerative Colitis (UC)
Irritable Bowel Syndrome (IBS)
Celiac Disease.
Food Allergy.
Food Intolerance.
Colon Cancer.
Vasculitis.
Common Variable Immune Deficiency.



31 Comments