Cervical Plexus
Table of Contents
Introduction
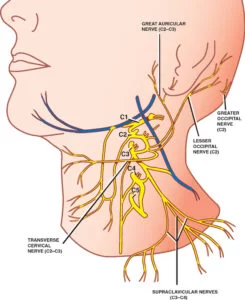
The cervical plexus is a complex network of nerves that originates from the spinal nerves of the cervical region of the spinal cord, specifically from the ventral rami of the first four cervical nerves (C1-C4). This intricate arrangement of nerves plays a crucial role in innervating various structures in the neck, head, and shoulders.
The cervical plexus forms within the posterior triangle of the neck, beneath the sternocleidomastoid muscle. Its primary function is to provide motor and sensory innervation to muscles of the neck and shoulder region, as well as to supply sensation to the skin of the neck and scalp.
It is situated on the cervical fascia’s prevertebral surface, midway up the sternocleidomastoid muscle, and the posterior triangle of the neck. The plexus is specific through the anterior rami (divisions) of cervical spinal nerves C1-C4.
The first (i.e., uppermost) four cervical spinal nerves C1–C4 form the anterior rami of the nerve plexus known as the cervical plexus. The cervical plexus gives some diaphragm and neck muscles motor awareness, and it gives certain head, neck, and chest organs sensory awareness.
The anterior (ventral) rami of spinal nerves C1–C4 combine to produce the cervical plexus, which is an accumulation of cervical nerves. These are the source (limbs) of the cervical plexus.
Due to its involvement in the development of the phrenic nerve, one of the motor branches of the cervical plexus, the fifth cervical nerve (also known as the anterior ramus of spinal nerve C5) may also be regarded as a component of the plexus. Therefore, the cervical plexus can also do defined as a network of nerves formed by the anterior rami of spinal nerves C1 – C5 that give both motor (deep) and sensory (superficial) branches.
Anatomy
The cervical plexus could be related to a web of nerves. A plexus is a mixture of nerves. The anterior portions of spinal nerves C1 through C4 and a piece of C5 come together to form the cervical plexus.
When referring to the anterior and posterior portions of spinal nerves, there is some ambiguous terminology. All spinal nerves are composed of a combination of anterior (ventral, front, motor) and posterior (dorsal, back, sensory) nerve roots that occur from the spine.
Each spinal nerve then divides once more into an anterior and a posterior branch (rami) after forming its anterior and posterior components. Any given spinal nerve’s anterior and posterior rami don’t always travel in the same direction.
Anterior and posterior rami could be motor nerves, sensory nerves, or both. The anterior rami of the respective cervical spinal nerves are where the cervical plexus gets its start.
Structure
There are six sizable nerves that branch off into smaller ones in the cervical plexus. The primary nerves of the cervical plexus are:
- Ansa cervicalis: The ansa cervicalis is shaped similarly to an arc and is made up of branches from the C1, C2, and C3 vertebrae.
- Lesser occipital nerve: included branches from C2 and C3, this nerve treks up toward the ear.
- Great auricular nerve: This nerve journey up towards the ear and is determined by branches from C2 and C3.
- Transverse cervical nerve: This nerve, which is made up of a combination of C2 and C3 branches, wraps around the neck to receive sensory input from neck tissues.
- Supraclavicular nerve: This nerve, which is composed of branches from C3 and C4, connects to form the anterior, middle, and posterior parts.
- Phrenic nerve: The longest nerve of the cervical plexus, the phrenic nerve is decided by branches of C3, C4, and C5.
Location
They are situated lateral to the transverse processes that join them. scalenus, m. levator scapulae, and m. splenius cervicis vertebral muscles from the lateral side and the medial side, respectively. There is a junction with the accessory nerve, hypoglossal nerve, and sympathetic trunk. It is finding the neck, deep to the sternocleidomastoid muscle.
It is under the sternocleidomastoid (SCM) muscle, opposite the upper four cervical vertebrae. It rests upon the levator anguli scapulae and scalenus medius muscles and comes from the posterior border of the SCM.
The cervical plexus branches leave the posterior triangle at the nerve point, which is situated midway along the sternocleidomastoid’s posterior surface.
For instance, before the ansa cervicalis divides into its numerous smaller nerve branches that continue up towards the mouth, the anterior cervical rami that make up this nerve curve downward in the neck as they combine.
The phrenic nerve travels down the process through the chest, near the heart and lungs, to the diaphragmatic muscle. The phrenic nerve’s structure and course on the left and right sides differ slightly as they descend towards the diaphragm because the heart and lungs are not symmetrical.
The sensory nerve ends of the greater auricular nerve and the smaller occipital nerve are located close to the ears. The transverse cervical nerve, as its name suggests, travels across the neck, whereas the supraclavicular nerve carries sensory fibers to the upper back and upper chest.
Branches of the Cervical Plexus
Increases are distributed by the cervical plexus to a number of branches that serve the head and neck structures. They can significantly be separated into two groups – muscular branches and sensory branches.
We should now examine these branches in more detail.
Muscular Branches
- The muscular branches of the cervical plexus are found deep in the sensory branches.
- They provide some of the muscles of the neck, back, and diaphragm.
- The muscle branches are ready to move first in an anteromedial orientation after emerging from the cervical plexus.
- This is in distance to the cutaneous branches, which travel posteriorly.
Phrenic Nerve
- The phrenic nerve comes from the anterior rami of C3-C5. It provides motor awareness to the diaphragm.
- After onset from the cervical plexus, the nerve moves down the surface of the anterior scalene muscle and enters the thorax.
- In the thoracic cavity, the nerve descends anteriorly to the source of the lung to achieve the diaphragm.
- A good memory aid for the source of the phrenic nerve is C3,4,5 have the diaphragm alive.
Nerves to Geniohyoid and Thyrohyoid
- The geniohyoid, which expands the airway by moving the hyoid bone anteriorly and upward, and the thyrohyoid, which depresses the hyoid bone and elevates the larynx, receive more nerves from the C1 spinal nerve.
- These nerves move with the hypoglossal nerve to reach their respective muscles.
Ansa cervicalis
The ansa cervicalis is an arc of nerves, formed by nerve roots C1-C3. It gives off four muscular branches:
- Superior belly of the omohyoid muscle.
- Inferior belly of the omohyoid muscle.
- Sternohyoid nerve (C1 – C3).
- Sternothyroid(C1 – C3).
- Thyrohyoid nerve (via hypoglossal nerve) (C1).
These muscles (the infrahyoid) act to depress the hyoid bone; an important role for swallowing and speech.
Other Muscular Branches
Several other minor branches begin from the nerve roots to supply muscles of the neck and back:
- C1-C2: Rectus capitis anterior and lateralis.
- C1-C3: Longus capitis.
- C2-C3: Present to the prevertebral muscles and sternocleidomastoid.
- C3-C4: present to the scalenus medial, trapezius, and levator scapulae.
Additionally, the cervical plexus provides direct innervation to the middle and anterior scalenus muscles.
Sensory Branches
- The skin of the neck, upper thorax, scalp, and ear is supplied by the cutaneous branches of the cervical plexus.
- These nerves all process the skin at the middle of the posterior border of the sternocleidomastoid.
- This region is connected while executing a cervical plexus nerve block and is referred to as the nerve point of the neck (Erb’s point).
Greater Auricular Nerve
- The greater auricular nerve is structured by fibers from C2 and C3 roots.
- It gives the skin above the parotid gland and the external ear sensibility.
- It is the big ascending branch of the plexus.
- The nerve also connects to the facial nerve’s posterior auricular branch, which innervates a few tiny muscles surrounding the ear, and the vagus nerve’s auricular branch.
Transverse Cervical Nerve
- The transverse cervical nerve is also structured by fibers from C2 and C3.
- It curves around the posterior aspect of the sternocleidomastoid and gives sensation to the anterior neck.
- The nerve subsequently picks up the deep cervical fascia, dividing into superior and inferiorly passing branches, and supplying the anterolateral skin of the neck and upper sternum.
Lesser Occipital Nerve
- The C2 root serves as the origin of the lesser occipital nerve, with some C3 input.
- It distributes cutaneous sensation to the posterosuperior scalp and commonly relates to the posterior branch of the greater auricular nerve.
- After its evolution, the nerve curves around the accessory nerve, and reach superiorly, close to the posterior border of the sternocleidomastoid.
Supraclavicular Nerves
- The C3 and C4 roots combine to form a group of nerves known as the supraclavicular nerves.
- They happen from behind the posterior border of the sternocleidomastoid and provide sensation to the skin extending the supraclavicular fossa and upper thoracic region and sternoclavicular joint.
Course and distribution
Sensory branches
- Lesser occipital nerve: This branch is formed by the second cervical nerve (C2) only, and courses to deliver the skin of the neck and the scalp posterosuperior to the clavicle.
- Great auricular nerve: This sensory branch comes from the C2 and C3 nerves. It courses upwards in an oblique fashion and crosses the sternocleidomastoid muscle onto the parotid gland. It then separates and innervates the skin over the parotid gland, the posterior aspect of the auricle, and an area of skin increase from the angle of the mandible to the mastoid process.
- Transverse cervical nerve: The second and third cervical nerves’ axons combine to produce the transverse cervical nerve. It provides the skin for the neck’s anterior triangle. This branch crosses the sternocleidomastoid muscle deep into the platysma muscle, curving across the center of its posterior border.
- Supraclavicular nerves: These branches are decided by the C3 and C4 spinal nerves, and emerge as a common trunk under cover of the sternocleidomastoid muscle. To reach the neck skin, this splits into three smaller branches (medial, middle, and lateral). Some branches also cross the clavicle to give the skin over the shoulder.
Motor branches
- The ansa cervicalis: The five motor branches of the ansa cervicalis arc listed above, originate from C1 to C3 nerves. Superior and inferior sources that are determined by fibers from the anterior rami of the cervical spinal neurons make up the ansa cervicalis. They provide the infrahyoid muscles in the anterior cervical triangle.
- The phrenic nerve: The third and fifth cervical nerves (C3 and C5) also contribute to the development of the phrenic nerve, which is mostly derived from the fourth cervical nerve (C4). It is decided at the superior part of the lateral border of the anterior scalene muscle, at the level of the superior border of the thyroid cartilage. Motor, sensory, and sympathetic nerve fibers can all be found in the phrenic nerve. It provides the sole motor provides to the diaphragm as well as sensation to its central part. The mediastinal pleura and pericardium of the heart are both innervated by the phrenic nerve in the thorax. The transverse cervical and suprascapular arteries, as well as the prevertebral layer of the deep cervical fascia, are all reached by the phrenic nerve as it descends obliquely across the anterior scalenus muscle. It runs posterior to the subclavian vein and anterior to the internal thoracic artery as it accesses the thorax.
Function
Numerous nerve branches exit the cervical plexus, many of which carry sensory data from various body regions and some of which stimulate muscles.
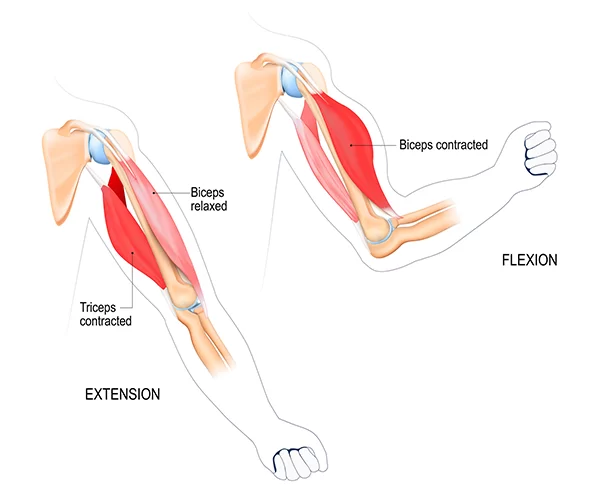
Motor
Motor nerves release neurotransmitters to nearby muscles, which produce the muscles to become activated (contract or shorten). The motor terminals of the cervical plexus’s branches activate their respective muscles and cause some bodily motions.
- Chewing and Swallowing: The omohyoid, sternohyoid, and sternothyroid muscles of the jaw and neck are activated by the motor nerve branches that emerge from the ansa cervicalis. These movements assist in chewing and swallowing.
- Breathing: One of the primary motor elements of the cervical plexus is the phrenic nerve, which causes the diaphragm to contract in order to power breathing. This nerve runs to the diaphragm, a muscle that divides the abdominal cavity, which houses your stomach and intestines, from the chest cavity, which contains your ribs, heart, and lungs. The matching phrenic nerve stimulates the contraction (shortening) of each side of the diaphragm. The chest opens up when the diaphragm contracts, allowing the lungs to fill with air. As you inhale and exhale, the diaphragm alternately expands and shrinks.
Sensory
The sensory branches of the cervical plexus gather sensory data from the ear, neck, and upper chest and send it up to the brain after passing through the spinal nerves to the brain, where it is integrated into the cerebral cortex’s sensory region.
Branches of the larger auricular nerve and lesser occipital nerve carry sensation to the area around the ear. The transverse cervical nerve receives sensation from the neck, and branches of the supraclavicular nerve carry sensation from the upper back and chest.
When you have visceral discomfort from infections or other medical conditions, the sensory branches of the phrenic nerve typically bring messages from deep portions of the chest.
Clinical Significance
Cervical plexus block
- In order to give regional anesthesia, a cervical plexus block is typically utilized during neck surgeries such as carotid endarterectomy, thyroidectomy, and cervical lymph node excision.
- A nerve block is a procedure to suppress the conductance of nerve impulses, typically used for regional anesthetic prior to surgery.
- In a cervical plexus block, an anesthetic is injected at several locations along the sternocleidomastoid muscle’s posterior border, primarily at the intersection of the muscle’s superior and middle thirds, which is the neck nerve point.
- Patients with pulmonary or cardiac problems are not candidates for this surgery since the cervical plexus block paralyzes the phrenic nerve, which supplies the diaphragm pericardium.
Phrenic nerve severance
- Diaphragm paralysis comes from phrenic nerve severance (injury).
- A phrenic nerve block can potentially lead to temporary diaphragm paralysis.
- In this case, the nerve is surrounded by an anesthetic injection at its location on the anterior surface of the middle part of the anterior scalene muscle.
- A prolonged duration of paralysis will result from a surgical phrenic nerve crush (for instance, for weeks after a diaphragmatic hernia repair).
Summary
The cervical plexus is a complicated neurologic structure located within the head and neck. The large portion of the cervical plexus is the connection between the anterior divisions of C1 through C4 nerves.
FAQS
The cervical plexus is a complicated neurologic structure located within the head and neck. The large portion of the cervical plexus is the connection between the anterior divisions of C1 through C4 nerves.
The most significant motor branch of the cervical plexus is the phrenic nerve. The plexus also give motor fibers to the spinal accessory nerve and to the paravertebral and deep muscles of the neck. Each nerve, with the exception of the first cervical nerve, gives significant cutaneous sensory awareness.
It has both a shallow and deep set of branches. The great auricular nerve, smaller occipital nerve, transverse cervical, suprasternal, and supraclavicular nerves are the superficial branches. The phrenic, cervical, connecting, and muscle branches are the deep branches.
The first (i.e., uppermost) four cervical spinal nerves C1–C4 form the anterior rami of the nerve plexus known as the cervical plexus. The cervical plexus provides motor awareness to give sensory innervation to parts of the head, neck, and chest.
Of the four major nerve plexuses (cervical, brachial, lumbar, and sacral), only the brachial plexus and sacral plexus could be analyzed sufficiently in the EDX laboratory. Fortunately, brachial plexus diseases are much more common than those of any other plexus.
Some of the structures in the neck and trunk receive knowledge from the cervical plexus, a network of nerve fibers. It is located in the cervical fascia’s prevertebral layer, halfway up the sternocleidomastoid muscle, and the posterior triangle of the neck.
The anterior (ventral) rami of spinal nerves C1–C4 (also known as the first–fourth cervical nerves) combine to form the cervical plexus, a collection of cervical nerves. These are the source (limbs) of the cervical plexus.
One of the spinal nerves in the cervical division is called the cervical spinal nerve 1 (C1). The C1 transmits primarily motor fibers, but it also has a short meningeal branch that, via dorsal rami, delivers sensation to areas of the brain around the foramen magnum.
Superficial cervical plexus block gives dense anesthesia for procedures like carotid endarterectomies, lymph node dissection, plastic surgery, laceration repairs, and incision and drainage of abscesses. It avoids the potential for under- or overdosing when applying oral or parenteral analgesics.
The phrenic nerve is a very significant nerve in the cervical plexus as it is responsible for the movement of the diaphragm, which is the muscle that controls breathing. The phrenic nerve comes from the cervical spine and travels down to the diaphragm.