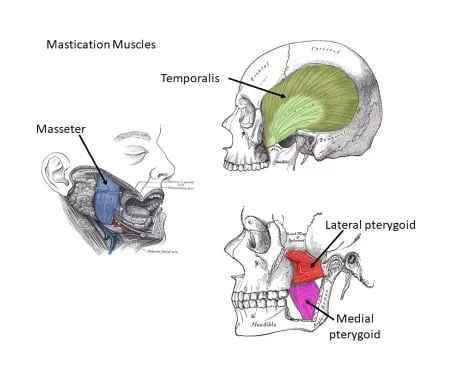
Muscles Of Mastication
Table of Contents
Introduction
Muscles Of Mastication are a set of muscles that are responsible for the chewing movement of the jaw at the temporomandibular (TMJ) joint, they improve the eating process, help with food crushing, and also function to approximate the teeth.
The four basic masticatory muscles originate from the surface of the skull and relate to the mandible’s rami at the TMJ. Elevation, depression, protrusion, retraction, and side-to-side movement are all possible with these muscles. Three of the major muscles control mandibular adduction, whereas one controls mandibular abduction.
- Protrusion (protraction) is the movement of the mandible forward.
- Retraction is the pulling back of the mandible.
- Elevation is a technique that raises the jaw and shuts the mouth.
- Depression causes the mandible to depress and the mouth to open.
- Rotation results in side-to-side movement of the mandible.
Unlike the facial nerve (CN VII), which innervates the muscles of expression, the muscles of mastication are innervated by motor branches of the trigeminal nerve’s mandibular division (CNV3), with the predominant arterial supply obtained from branches of the maxillary artery.
Muscles Of Mastication
The masticatory muscles are classified as primary muscles and secondary or accessory muscles.
- The major muscles are as follows:
- Masseter
- Temporalis
- Pterygoid lateralis
- Pterygoid medialis
2. The secondary or accessory muscles are as follows:
- Buccinator
- The muscles classified as suprahyoid are the geniohyoid, mylohyoid, and digastric muscles.
- Among the infrahyoid muscles are the omohyoid, thyrohyoid, sternohyoid, and sternothyroid muscles.
Primary Muscles
Masseter muscle
The masseter muscle is a powerful quadrangular muscle that covers the lateral portion of the mandible’s ramus. It is made up of two layers with somewhat different attachments:
- Its bigger, superficial layer is formed by the zygomatic bone’s maxillary process and the front two-thirds of the zygomatic arch. These muscle fibers go inferiorly and posteriorly from this point to attach to the lateral surface of the angle and the bottom portion of the ramus of the mandible.
- The masseter muscle’s deep layer develops from the zygomatic arch’s medial surface and inferior edge. These fibers extend vertically downwards to attach to the upper section of the mandible’s ramus and the coronoid process.
The masseter muscle is innervated by the masseteric nerve, a branch of the mandibular nerve. It supplies blood from the masseteric artery, which branches from the maxillary artery. The masseter muscle’s primary function is to raise the jaw, with a modest contribution to mandibular protrusion.
Temporalis muscle
The temporalis muscle is a big, flat muscle located within the skull’s temporal fossa. This fan-shaped muscle comes from the deep surface of the temporal fascia as well as the entire temporal fossa below the temporal line. Its muscle fibers congregate anteriorly to create a tendon that extends deep into the zygomatic arch. The tendon then inserts on the coronoid process’s apex and medial surface, as well as the anterior border of the ramus of the mandible.
The muscle is innervated by the mandibular nerve’s deep temporal branches and vascularized by the maxillary artery’s deep temporal branches and the superficial temporal artery’s middle temporal branches.
The temporalis muscle primarily serves as a mandibular elevator. This function is mostly produced by its anterior vertical fibers, which are constantly active and oppose gravity while the mouth is closed. When the posterior, more horizontal fibers of the muscle contract, the mandible retracts, drawing the jaw rearward. Furthermore, the temporalis muscle aids grinding actions by shifting the jaw from side to side.
Medial Pterygoid Muscle
The quadrangular medial pterygoid muscle is located in the infratemporal fossa. It is made up of two heads, each with its own set of origins.
- The greater deep head develops from the medial surface of the sphenoid bone’s lateral pterygoid plate and the neighboring palatine bone’s pyramidal process.
- The tuberosity of the maxilla gives rise to the smaller superficial head.
Both heads ring the lateral pterygoid muscle’s bottom fibers. The muscle heads converge and run posterolaterally in an oblique direction from their points of origin to insert on the medial surface of the mandibular ramus, near the angle of the jaw.
The medial pterygoid branch of the mandibular nerve innervates the medial pterygoid muscle. It receives its primary blood supply from the pterygoid branches of the maxillary artery.
This muscle’s primary function includes mandibular elevation and side-to-side movements during grinding and chewing. The mandibular protrusion is also caused by the medial pterygoid.
Lateral Pterygoid Muscle
The infratemporal fossa contains the lateral pterygoid muscle, which is a triangle muscle. The lateral pterygoid muscle, like the medial pterygoid, has two heads with two separate sources.
- The inferior surface of the greater wing and the infratemporal crest of the sphenoid bone, which constitute the ceiling of the infratemporal fossa, give rise to the smaller, superior head.
- The bigger, inferior head develops from the lateral surface of the sphenoid bone’s lateral pterygoid plate.
The fibers from both heads join and run posterolaterally to implant onto the pterygoid fovea, a shallow depression on the anterior aspect of the mandible’s neck. Furthermore, some fibers intrude on the temporomandibular joint (TMJ) joint capsule and articular disc.
The lateral pterygoid muscle is innervated by the mandibular nerve’s lateral pterygoid branch and vascularized by the maxillary artery’s pterygoid branches.
The lateral pterygoid’s function is determined by the degree to which it contracts. Bilateral pterygoid muscle contraction protrudes and depresses the jaw. A unilateral contraction on one side, together with the ipsilateral medial pterygoid muscle, causes the mandible to shift to the opposite side. This enables alternating side-to-side movements while chewing.
Secondary
Suprahyoid muscles
The digastric muscle, mylohyoid muscle, and geniohyoid muscle comprise the suprahyoid muscle group. When the infrahyoid muscles fix or depress the hyoid bone, they depress the mandible against opposition.
Infrahyoid Muscles
They consist of the omohyoid, sternohyoid, sternothyroid, and thyrohyoid glands. They either fix or depress the hyoid bone.
Buccinator
The buccinator is a facial expression muscle that assists with mastication by pushing food back into the oral cavity.
Clinical Significance
Myofascial discomfort and dysfunction, myositis, and neoplasms are all examples of masticatory muscle problems.
Myofascial discomfort and dysfunction can be caused by a variety of factors. The most prevalent are nocturnal bruxism, chronic mouth clenching, and whiplash injuries sustained during a trauma. An imbalance of forces within the masticatory muscles can cause temporomandibular joint (TMJ) dysfunction. Teeth grinding at night (bruxism) is a common cause of TMJ discomfort due to an imbalance in the muscle of mastication forces caused by excessive grinding of the teeth.
A trismus (masticatory muscular spasm) can be an indication of a tumor or infection. Tetanus, for example, can cause “lockjaw” or trismus. Other infections or inflammations of the muscles can manifest as myositis or pain when moving the jaw.
Tumors, even uncommon, can develop in the masticator area, which is surrounded by the deep cervical fascia. These cancers may spread from neighboring areas. The fascia is linked to the skull base on the medial side and extends to the temporalis muscle on the lateral side. It is linked to the mandible’s body anteriorly at the level of the oblique line, and posteriorly to the mandible’s ramus.
Summary
The muscles of mastication are a group of four muscles that control the movement of the lower jaw (mandible). They are responsible for chewing, grinding food, and speaking.
The four muscles of mastication are:
- Masseter: The masseter muscle is the most powerful muscle of mastication and is responsible for closing the mouth.
- Temporalis: The temporalis muscle is located on the side of the head and helps to close the mouth and move the jaw forward and backward.
- Medial pterygoid: The medial pterygoid muscle is located deep in the cheek and helps to close the mouth and move the jaw from side to side.
- Lateral pterygoid: The lateral pterygoid muscle is also located deep in the cheek and helps to open the mouth and move the jaw from side to side.
The mandibular branch of the trigeminal nerve innervates all masticatory muscles. This nerve is responsible for sending sensory and motor signals to the face, including the muscles of mastication.
The muscles of mastication are also supplied with blood by the maxillary artery. This artery is responsible for supplying blood to the face, including the muscles of mastication.
The muscles of mastication are essential for chewing, grinding food, and speaking. Without these muscles, we would not be able to eat or speak properly.
Problems with the muscles of mastication can cause a variety of symptoms, including:
- Pain in the jaw, face, or neck
- Difficulty chewing
- Limited jaw movement
- Temporomandibular joint disorder (TMJ)
FAQs
The muscles of mastication are a group of four muscles that control the movement of the lower jaw (mandible). They are responsible for chewing, grinding food, and speaking. The four muscles of mastication are:
Masseter
Temporalis
Medial pterygoid
Lateral pterygoid
The muscles of mastication work together to move the mandible in a complex pattern that allows us to chew food. They also help to grind food into smaller pieces, which makes it easier to digest. Additionally, the muscles of mastication are involved in speaking, helping to move the mandible in a way that allows us to produce different sounds.
Problems with the muscles of mastication can cause a variety of symptoms, including:
Pain in the jaw, face, or neck
Difficulty chewing
Limited jaw movement
Temporomandibular joint disorder (TMJ)
Treatment for problems with the muscles of mastication will vary depending on the underlying cause. However, some common treatments include:
Medication to reduce pain and inflammation
Physical therapy to strengthen and stretch the muscles of mastication
Mouth guards to prevent grinding and clenching of the teeth
Surgery in some cases
There are a few things you can do to keep your muscles of mastication healthy, including:
Eating a balanced diet
Getting regular exercise
Avoiding smoking and excessive alcohol consumption
Practicing good oral hygiene
Seeing a dentist for regular checkups and cleanings
References:
MSc, E. O. M. (2023, October 23). Muscles of mastication. Kenhub. https://www.kenhub.com/en/library/anatomy/the-muscles-of-mastication
Muscles of Mastication. (n.d.). Physiopedia. https://www.physio-pedia.com/Muscles_of_Mastication